Analysis of the Impact of Size of Brain Metastases in the Overall Survival of Patients with Primary Head and Neck Cancer, Melanoma and Sarcoma
1Radiation Oncology, Portuguese Institute of Oncology Francisco Gentil, Portugal
2Nova Medical School, Portugal
- *Corresponding Author:
- António Manuel
Silva Mota
Radiation Oncology, Portuguese
Institute of Oncology Francisco Gentil
Nova Medical School, Portugal
Tel: 215-537-7400
E-mail: amsrmota@gmail.com
Received: March 27, 2019; Accepted: May 03, 2019; Published: May 13, 2019
Citation: Mota AMS, Roldão M, Netto E, Silva P, Pedro C, et al. (2019) Analysis of the Impact of Size of Brain Metastases in the Overall Survival of Patients with Primary Head and Neck Cancer, Melanoma and Sarcoma. J Med Oncol. Vol.2 No.1:3
Abstract
Introduction: Management of brain metastases (BMs) depends on important prognostic factors such as age, performance status (PS), primary cancer and the status of extracranial metastases. At this moment, the size of brain metastasis (BM) is used to decide the therapeutic approach but not as a prognostic factor. Methods: A retrospective and single center study, of patients with primary head and neck cancer, melanoma or sarcoma with diagnosis of BMs from 2006 to 2015 were analysed. Patients were selected by number of BMs (≥ 4) and/or by size of the largest BM (≥ 3 cm). The aim was to evaluate the association between the size of BM and overall survival (OS), in months, and the second outcome was to evaluate the association between whole brain radiotherapy (WBRT) and OS, in months. We compared the association by baselines covariates using log-rank test and Cox proportional hazards regression. Results: 66 patients were collected (median age 63 years old) with primary head and neck cancer, melanoma or sarcoma. In univariate analysis, there was no difference in OS between gender, number of BMs and primary cancer. However, there was a statistical difference in OS when the diameter of the largest metastasis is ≥ 3 cm (difference in median OS=1.3 months, p<0.05). There was also an increase in OS among patients treated with WBRT (difference in median OS=2.5 months, p<0.05). In a multivariate analysis, there was no difference in association between the size of BM and OS (Hazard Ratio (HR)=1.6, 95% CI: 0.82-3.2), p=0.16). Conclusion: This retrospective study shows no association between BMs’ size and OS in patients with primary head and neck cancer, melanoma or sarcoma.
Keywords
Size of brain metastasis; Whole brain radiotherapy; Prognostic factor; Overall survival
Introduction
Brain metastases (BMs) are the most common primary malignant lesions of central nervous system, with the total number diagnosed annually outnumbering all other intracranial tumours combined [1]. With the increasing survival of patients with extracranial metastases, the incidence of the BMs in the most common cancers (lung, breast, renal and colon) is thought to be rising [1]. One important factor with impact in the overall survival (OS) for patients with BMs is the primary cancer. Patients with BMs with breast cancer have a higher median OS when compared to patients with other types of cancers such as melanoma, sarcoma or head and neck cancer [1,2].
There are established factors associated with OS among patients with this diagnosis such as age (OS is higher in individuals <65 years old), number of BMs, performance status (PS) and primary disease status (with or without extracranial metastases) [3,4]. In current clinical practice, the size of brain metastasis (BM) is considered to decide the best therapeutic approach but not as a prognostic factor [3,4]. The more we know about prognostic factors for each primary cancer, the better and more relevant treatment for BMs can be provided for this group of patients. There are several therapeutic options to treat BMs such as: glucocorticosteroids, surgery and radiotherapy (whole brain radiotherapy (WBRT) and/or stereotactic radiosurgery (SRS)) [3- 5].
What we know is that there is an association between the risk of radionecrosis and the size of BMs, when the largest diameter is ≥ 3 cm, when patients are treated with SRS [6,7]. Can we consider the size of BM as a prognostic factor? Is there an association between the size of BMs and OS? Based on the current data about the association between size and radionecrosis, in this study it will be considered the cut-off of 3 cm for the size of the largest BM, to evaluate its association with OS in patients with primary head and neck cancer, melanoma or sarcoma. In this research, in the group of patients mentioned above, we will evaluate if there is an association between WBRT and OS.
Materials and Methods
This is a retrospective, single center study (Instituto Português de Oncologia de Lisboa Francisco Gentil, in Lisbon) using data collected from the Portuguese Oncology Database (ROR-SUL) and from patients' charts, according to the criteria described below.
Study Population
The authors received a database from ROR-SUL. In this database, they searched for all patients with the diagnosis of primary head and neck cancer, melanoma or sarcoma with BMs diagnosis, from 2006 to 2015. After that, the authors reviewed all consecutive patients and selected the patients per the following criteria described below (Table 1).
| Inclusion criteria | Exclusion Criteria |
|---|---|
| Age = 18 years old | Any prior cranial irradiation |
| Pathology exam of the primary cancer (head and neck cancer, melanoma or sarcoma). | Any prior brain surgery |
| CT or MRI with the report of the number and size of BMs (= 4 BMs and/or one BM = 3 cm in diameter) | Any prior primary brain cancer |
| Treatment for BMs: WBRT (yes or no). | Missing date of death/missing follow-up |
Table 1 Inclusion and exclusion criteria.
Once eligibility was established we collected clinical information for the following variables for each patient: gender, primary cancer, date of diagnosis of BM, age at the time of BM diagnosis (<65 or ≥ 65 years old), extracranial metastases (present/absent), number of BMs (1, 2, 3 or ≥ 4), size of the largest BM (at least one BM ≥ 3 cm in diameter), Eastern Cooperative Oncology Group (ECOG) Performance Status (PS), 0 to 4, for each patient at the time of BMs diagnosis, treatment for BMs with WBRT (yes or no) and date of death/last follow-up. In terms of treatment with WBRT, all patients were treated in accordance with the Radiation Therapy Oncology Group (RTOG) guidelines: 20 Gy to 30 Gy in 5 sessions (4 Gy per session) to 10 sessions (3 Gy per session), respectively, in consecutive days, Monday to Friday [7].
Outcomes
The aim is to verify if there is an association between the size of the BM (≥ 3 cm in diameter) and the OS (in months) and, for second outcome, is to identify the association between WBRT and OS (in months), in patients with ≥ 4 BMs and/or with one BM ≥ 3 cm, with primary head and neck cancer, melanoma or sarcoma.
Statistical Analysis
The OS was defined by the number of months that each patient is alive between the date of diagnosis of BMs and the date of death/ last follow-up. Factors affecting the OS were tested using the logrank test for univariate analysis, and Cox regression’s model in multivariate survival analysis. Univariate survival analysis will be presented using Kaplan-Meir curves and multivariate survival analysis by hazard ratios. Statistical significance was set up p<0.05. All statistical tests were conducted using STATA v.14.2.
Ethics
This protocol was approved by the Institutional Review Board (IRB) from Instituto Português de Oncologia de Lisboa Francisco Gentil.
Results
All baseline patients’ characteristics of this cohort are described in Table 2. Data referring to sixty-six patients (40 men and 26 women) were collected from 2006 and 2015. The median age of patients with BMs at the time of diagnosis was 63 years old (50-70; CI 25%-75%). Melanoma was the most prevalent primary cancer (76%), followed by head and neck cancer (18%) and sarcoma (6%). Melanoma primary site was unknow in 5 patients and from skin in 45 patients. The primary site for head and neck cancer was oropharynx (3 patients), oral cavity (1 patient), and unknow primary head and neck cancer (2 patients). In the group of patients with sarcoma, the primary location was limbs (4 patients). The distribution by ECOG PS was the following: 45% with PS2 and PS3 and 55% with PS4 and only 12% of patients didn't have extracranial metastases at the time of BMs diagnosis. In terms of number of BMs, 74% of this cohort had at least ≥ 4 BMs and 67% of patients had at least one BM ≥ 3 cm. In terms of treatment for BMs, 55% were treated with WBRT. The other 45% of patients underwent dexamethasone only. The median survival (in months) of this cohort was 1.8 months. In univariate analysis, patients <65 years had an increase in 1 month in OS when compared with patients ≥ 65 years (2.73 months compared to 1.70 months, p<0.05). There was also an increase of OS according to the patients' PS, at the time of BMs' diagnosis (PS 2 (12.7) vs PS 3 (3.4) vs PS 4 (1.0), p<0.05).
| Covariates | Number (%) | |
|---|---|---|
| Age at diagnosis of Brain Metastases | <65 years | 35 (53%) |
| = 65 years | 31(47%) | |
| Gender | Male | 40 (61%) |
| Female | 26 (39%) | |
| Primary Cancer | Head and Neck Cancer | 12 (18%) |
| Melanoma | 50 (76%) | |
| Sarcoma | 4 (6%) | |
| ECOG PS2 | PS 2 and PS3 | 30 (45%) |
| PS 4 | 36 (55%) | |
| 1 Metastasis | 9 (14%) | |
| Brain Metastases, number | 2 Metastases | 5 (8%) |
| 3 Metastases | 3 (4%) | |
| = 4 Metastases | 49 (74%) | |
| One Brain Metastasis = 3 cm in diameter | Absent | 22 (33%) |
| Present | 44 (67%) | |
| Treatment of Brain Metastases | Dexamethasone | 36 (55%) |
| 3WBRT+Dexamethasone | 30 (45%) | |
| Extracranial metastases | Absent | 8 (12%) |
| Present | 58 (88%) | |
Table 2: Baseline characteristics of patients.
However, there was no statistical difference in median survival between men and women (2.3 months for men vs 2.1 months for women, p=0.69), number of brain metastases (1 (2.1) vs 2 (0.9) vs 3 (2.1) vs ≥ 4 (2.4), p=0.08) or primary cancer (head and neck cancer (2.4) vs melanoma (2.2) vs sarcoma (1.8), p=0.89).
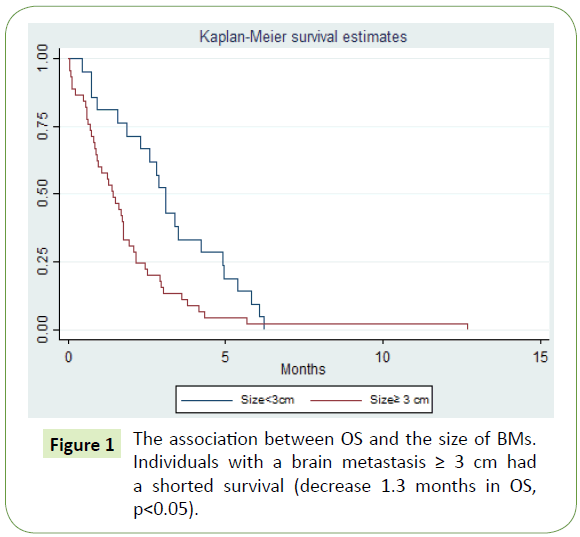
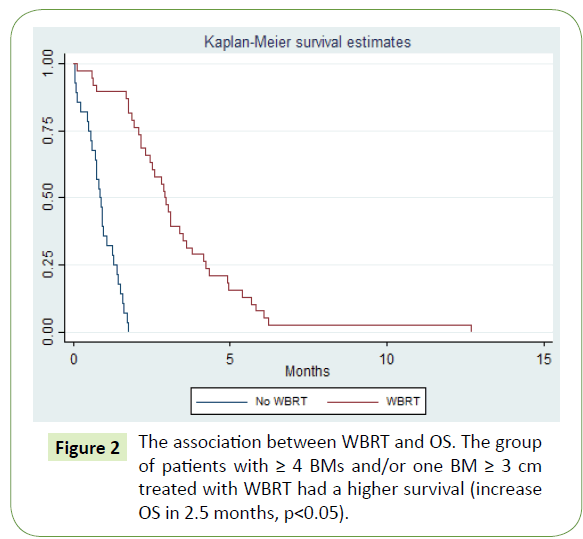
In terms of the size of BMs, when one metastasis is ≥ 3 cm in diameter, there is a decrease in OS=1.3 months (no (3.1) vs yes (1.8), p<0.05) (Figure 1). For this cohort of patients, there is also a benefit in WBRT in OS (no (0.8) vs yes (3.3), p<0.05) (Figure 2). In a multivariate analysis, with adjustment for covariates established as prognostic factors in BMs (age, number of BMs, PS and extracranial metastases) the size of the largest BM was not associated with OS in patients with a BM ≥ 3 cm (HR=1.6, 95% CI: 0.82:3.2, p=0.16). There was a strong association between survival and patients' PS at the time of BMs diagnosis (HR=9,1, 95% CI: 4.0-20.0, p<0.05) (Table 3).
Figure 1: The association between OS and the size of BMs. Individuals with a brain metastasis = 3 cm had a shorted survival (decrease 1.3 months in OS, p<0.05).
| Covariates | Number (%) | |
|---|---|---|
| Age at diagnosis of Brain Metastases | <65 years | 35 (53%) |
| = 65 years | 31(47%) | |
| Gender | Male | 40 (61%) |
| Female | 26 (39%) | |
| Primary Cancer | Head and Neck Cancer | 12 (18%) |
| Melanoma | 50 (76%) | |
| Sarcoma | 4 (6%) | |
| ECOG PS2 | PS 2 and PS3 | 30 (45%) |
| PS 4 | 36 (55%) | |
| 1 Metastasis | 9 (14%) | |
| Brain Metastases, number | 2 Metastases | 5 (8%) |
| 3 Metastases | 3 (4%) | |
| = 4 Metastases | 49 (74%) | |
| One Brain Metastasis = 3 cm in diameter | Absent | 22 (33%) |
| Present | 44 (67%) | |
| Treatment of Brain Metastases | Dexamethasone | 36 (55%) |
| 3WBRT+Dexamethasone | 30 (45%) | |
| Extracranial metastases | Absent | 8 (12%) |
| Present | 58 (88%) | |
2PS: Performance Status
3WBRT: Whole Brain Radiotherapy
`Table 2 Baseline characteristics of patients.
Discussion
The knowledge of prognostic factors in patients with BMs is important to predict OS and to perform the best treatment for each individual case. There are already very well-established prognostic factors such as age, PS, the presence or absence of extracranial metastases and the number of brain metastases [1,2].
The aim of this study was to identify if the size of BM could be a prognostic factor. Therefore, we evaluated the association between the size of the largest BM (≥ 3 cm) with OS. The data analysis did not find that BMs bigger than 3 cm were associated with increased mortality, after controlling for all covariates together (p=0.16). The second outcome was to evaluate the impact of WBRT in OS. The results of this study indicate that the group of patients who were treated with WBRT had an increase of survival (p<0.05) when compared with the group of patients treated with dexamethasone only (increase OS in 2.5 months) [6,7]. The results confirm the importance of ECOG PS at the time of BM diagnosis and its association with OS (HR=9.1, 95% CI: 4.0- 20) and the association between OS and the presence/absence of extracranial metastases (HR=3.3, 95% CI: 1.1-8.0).
However, the authors consider there are important limitations in this study. This is a study performed in a single center, with a small number of patients, despite 10 years of follow up. Although there were examinations (pathology, MRI and CT) we need to be aware of possible missing data. For example, it was not possible to have access to all comorbidities from each patient, and that was the reason for the absence of this information at the baseline characteristics of the patients in this sample. Besides that, the ECOG PS can be under or overestimated by the physician at the time of the patients' BMs diagnosis. All facts mentioned above can promote the existence of confounders from many sources and can have an important impact in this data analysis. The authors encourage the scientific community to develop more trials to evaluate not only the association between the size of BMs and OS but also to investigate other prognostic factors to predict survival, with the purpose to offer these patients the best treatment option.
Acknowledgments
The authors wish to thank the Portuguese Oncology Database (ROR-SUL) for sharing the Database that allowed to conduct this study and to Ciaran McMullan, António Mota's Harvard Advisor.
References
- Mehta MP, Tsao MN, Whelan TJ, Morris DE, Hayman JA, et al. (2005) The American Society for Therapeutic Radiology and Oncology (ASTRO) evidence-based review of the role of radiosurgery for brain metastases. Int J Radiat Oncol Biol Phys 63: 37-46.
- Tsao MN, Lloyd N, Wong RK, Chow E, Rakovitch E, et al. (2006) Whole brain radiotherapy for the treatment of multiple brain metastases-Full review. Cochrane Database Syst Rev 3.
- Gaspar LE, Mehta MP, Patchell RA, Burri SH, Robinson PD, et al. (2010) The role of whole brain radiation therapy in the management of newly diagnosed brain metastases: a systematic review and evidence based clinical practice guideline. J Neurooncol 96: 17-32.
- Mehta MP, Paleologos NA, Mikkelsen T, Robinson PD, Ammirati M, et al. (2010) The role of chemotherapy in the management of newly diagnosed brain metastases: a systematic review and evidence-based clinical practice guideline. J Neurooncol 96: 71-83.
- Inoue HK, Sato H, Suzuki Y, Saitoh J, Noda SE, et al. (2014) Optimal Hypofractionated Conformal Radiotherapy for Large Brain Metastases in Patients with High Risk Factors: A Single-Institutional Prospective Study. Radiation Oncology (London, England) 9: 231.
- Lee CC, Yen CP, Xu Z, Schlesinger D, Sheehan J (2014) Large intracranial metastatic tumors treated by Gamma Knife surgery: outcomes and prognostic factors. J Neurosurg 120: 52-59.
- National Comprehensive Cancer Network (NCCN) (2018) Guidelines for Central Nervous System. Accessed 11th December 2017.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences