A Case Report on 8-Year Survival of a 23-year old with Endometriod Adenocarcinoma of the Uterus Stage 4b
Juliana Yusof1*, Rushdan Mohd Noor2, Ismail Aliyas2, Ahmad Muzamir Ahmad Mustafa2and Nor Hafiza Ahmad3
1Department of Medicine, UiTM Sg Buloh, Selangor, Malaysia
2Department of Gynaecology, Gynaecology Oncologist, Sultanah Bahiyah Hospital, Alor Star, Malaysia
3Department of Gynaecology, Obstetrics&Gynaecology, Sultanah Bahiyah Hospital, Alor Star, Malaysia
- *Corresponding Author:
- Juliana Yusof
Department of Medicine
Faculty of Medicine
UiTM Sg Buloh, Selangor
Malaysia
E-mail: juliana.yusof@yahoo.com
Received Date: January 21, 2021; Accepted Date: February 04, 2021; Published Date: February 11, 2021
Citation: Yusof J, Noor RM, Aliyas I, Mustafa AMA and Ahmad NH (2021) A Case Report on 8-Year Survival of a 23-year-old with Endometriod Adenocarcinoma of the Uterus Stage 4b. J Women’s Health Reprod Med Vol. 5 No. 2:8.
Abstract
Endometrial Carcinomae (EC) usually occurs at after their thirties. A patient with stage IV EC usually shows short life expectancy. Here, we describe a unique stage IV EC patient, unique in that 1) she was 23 years old and 2) she survived 8 years. A 23-year old woman had heavy bleeding and the condition was diagnosed as uterine myoma: myomectomy was performed; during the surgery bloody ascites was noted and histological examination of resected uterine tissue (initially considered as myoma) revealed EC. Diagnosing this condition as EC, after informed consent, total abdominal hysterectomy with bilateral salpingo-oophorectomy with omentectomy was performed. Also, intra-surgical examination revealed the presence of sub-diaphragmatic metastatic lesion, which was resected. Reduction surgery was successfully performed; however, the cancer recurred, to which chemotherapy and irradiation was performed; she died after 8 years. We did not save her life; however, she lived 8 years in self-dependent manner.
Keywords
Advance endometriod adenocarcinoma of the Uterus; Young female; Prolong survival
Introduction
Endometrial cancer is usually seen in post menopause women but 2%-14% may occur in younger women less than 40 years old who wants to preserve their fertility [1]. We report a 23-year old single nulliparous with endometrial cancer stage 4 who had prolonged survival for 8 years.
Case Report
Patient was a 23-year-old factory worker who presented with the first episode of heavy menstrual bleeding (HMB) in May 2010 for 2 months. She attained her menarche at the age of 13 years old, her menses was regular of 7 days' duration, 28 days' interval until the age of 23 years old in 2010, and she experienced HMB. She experienced heavy menstrual flow especially on day 3 menses and severe dysmenorrhea especially on day 1 menses.
At gynaecology clinic Sultanah Bahiyah Hospital (HSB), she was diagnosed to have uterine fibroid by a trans abdominal scan of 18 weeks' size and was given tranexamic acid from day 2 to day 5 menses. Her body mass index was 21 kg/m2. The fibroid was located posteriorly measuring 4 × 5 cm, with endometrial thickness of 5 mm and uterine size was of 9 × 7 cm. Her ovaries were normal.
Intra-operatively, there was a pelvic mass measuring 18 weeks size with blood stained peritoneal fluid of 1.2 litres. There was a posterior fundal fibroid measuring 6 × 5 cm with no obvious capsule seen, hence the ennucleation was difficult. Both of her ovaries and fallopian tubes were normal. The blood loss during the operation was only 200 ml. She was fortuitous as the myomectomy was actually done by a Gynaecologist Oncologist who had suspected uterine carcinoma intraoperative based on the blood stained ascetic fluid. True enough, the Histo Pathological Examination (HPE) of the fibroid came as endometriod endometrial adenocarcinoma FIGO grade II. Unfortunately, expression of steroid hormone receptors through immunostaining could not be performed at that time as the immunostaining facility was not available. Taking into account the findings of HPE, the patient was recalled immediately after undergoing myomectomy for 12 days. She was advised for urgent CT Thorax Abdomen and Pelvis (CT TAP) succeeded by Extrafascial Hysterectomy+Bilateral Salpingoohorectomy as delaying the treatment may result in dissemination of the disease resulting in advanced stage of disease. The patient was extremely shocked, but after thorough consultation, she agreed to a major operation.
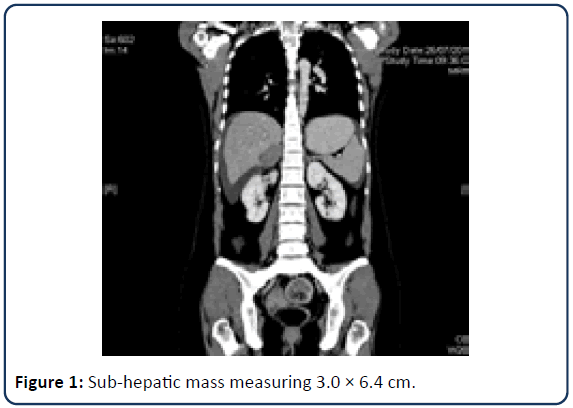
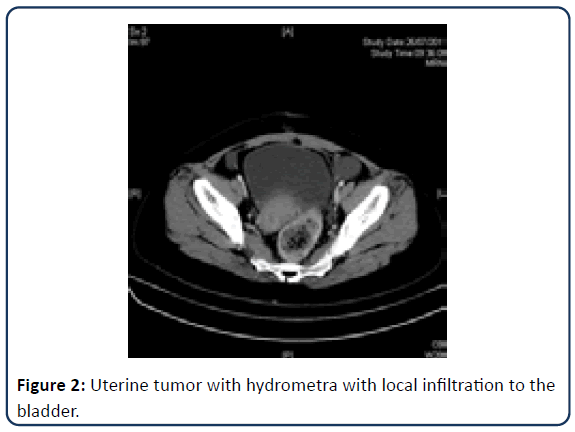
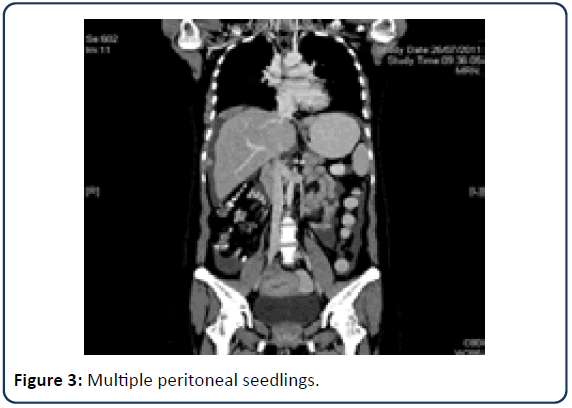
She had a CT TAP examination on July 26, 2011, which revealed metastatic endometrial cancer. Her sub hepatic mass was 3.0 × 6.4 cm (Figure 1). Her uterus was large, with fluid accumulation and local infiltration into the bladder and rectum. There was no clear fat plane with the urinary bladder anteriorly and upper rectum posteriorly (Figure 2). She also had moderate to gross ascites and several peritoneal seedlings (Figure 3).
The final impression of CT TAP made was correlating with HPE finding-Endometrium cancer with peritoneal metastases. Before the operation, her Ca125 was normal at 13. She underwent midline laparotomy Total Abdominal Hysterectomy Bilateral Salpingo Ophorectomy (TAHBSO)+Infracolic omentectomy+tumour debulking on 27th July 2011 which was 3 weeks after her myomectomy. The results of her surgery showed that she had 700 cc of haemorrhagic ascites and the uterine volume was 10 weeks. The cross section showed a small growth area, and the cavity area was 2 × 2 cm. The Hepatobiliary team was called in to proceed with the debulking of the peritoneal nodule over the sub diaphragmatic region measuring 3.0 × 6.4 cm. The final diagnosis HPE of her TAHBSO specimen was Endometriod Adenocarcinoma of the uterus (EAC) Stage 4B with the metastasis to the right ovary and tumour deposits located at sub diaphragmatic tissue and peritoneal wall. Six weeks after the operation, she visited the gynaecological cancer clinic. She had no complaint. Her scar had healed well. She has undergone her 1st cycle of chemotherapy on 1st September 2011 which was doxorubicin and cisplatin. She endured the first chemotherapy well with no serious adverse effect after her HPE report was reviewed. Prior to chemotherapy, she had a baseline echocardiogram done on 10th August 2011 as doxorubicin can cause cardiotoxicity. Her baseline echocardiogram was normal with good ejection fraction of 60%. Besides that, she also had 24 hours urine creatinine clearance done prior to chemotherapy and the value was 93.1 ml/min which was normal (normal value is >70 ml/min). She was given 107 mg (75 mg/m2) cisplatin in 500 ml over 6 hours followed by IV Doxorubicin 72 mg (50 mg/m2) slow bolus within 5 minutes. Her chemotherapy was given every 3 weeks interval and she was covered with a prepitant 80 mg OD for 3 days upon discharge for antiemetics. Her tumour markers prechemotherapy were normal.
She completed her 6 cycles (#) of doxorubicin and cisplastin in January 2012 and her Disease Free Interval (DFI) was 5 years (2011-2016). She was regularly monitored by CT TAP 6 monthly to once a year. Unfortunately, she complained of persistent pain in her right hip in May 2016. She denied numbness or difficulty walking around. Clinically, there was an obvious lump in her right hip area with a size of 4 × 5 cm. Pelvic X-ray was done which revealed a mass measuring 4 × 4 cm at the right iliac crest. CT TAP was done in May 2016, which revealed multiple sclerotic and lytic lesion and erosion of right iliac bone with right psoas mass measuring 8 × 15 cm. She also developed splenic, peritoneal and mesenteric metastases detected on CT TAP. A bone biopsy was taken by the orthopaedic team of which the HPE came back as metastatic carcinoma consistent with endometriod adenocarcinoma. Besides being treated with Pregabalin 100 mg daily, she agreed for palliative chemotherapy, which was 6# paclitaxel/carboplatin as well as treated with hormonal therapy, which was Medroxy Progestrone Acetate (MPA) 100 mg daily. After completing palliative chemotherapy-6# Paclitaxel/ Carboplatin, she was monitored by CT TAP in November 2016. CT TAP showed that the lesions of the spleen had been reduced, but the size of the mass seen on the right psoas muscle was still similar to that in May 2016.
Discussion
Endometriod Adeno Carcinoma (EAC) of the uterus occurred in 2%-14% of cases, in patients less than 40 years of age [1]. The youngest age reported was a 13 year old girl from Korea who presented with heavy menstrual bleeding due to stage 1 endometriod carcinoma [2] detected on MRI pelvis and treated conservatively with levonorgestrel intrauterine system device. This 13 year old girl noted to have polycystic ovaries on MRI pelvis. However for this unfortunate patient, the risk factor for her to develop stage 4 endometriod adenocarcinoma of the uterus at the age of 23 years old was uncertain. She had no family history of malignancy, she was not overweight and her ovaries intra-operatively were not morphologically polycystic. With the surgical pathology diagnosis of EAC stage 4B, she tremendously survived for 8 years. According to statistics on uterine cancer in the UK, their 1-year survival rate in EAC stage 4 is 10% [3]. Therefore, some factors help prolong survival in this patient were identified and discussed as follows:
Role of cytoreduction surgery
Although the majority of patients with endometrial cancer are diagnosed at an early stage, from 10% to 15% will present with advanced‐stage disease, and their prognosis is poor. When disease is primarily intra peritoneal, management is often extrapolated from that of ovarian cancer. Cytoreduction to <2 cm has also been correlated with survival, with the maximum benefit in patients who can be reduced to no visible disease remaining [4].
Role of chemotherapy in advance stage vs. abdominal irradiation
The most common chemotherapy regime used in HSB for endometrial cancer is combination of Doxorubicin and Carboplatin in about 60% of cases. Combination of paclitaxel and platinum were given to approximately 40% of patients. Report that carboplatin paclitaxel regimen is well tolerated, active regimen for the treatment of resected stage III or IV with 3 year survival rate of 56% and median survival of 47 months [5]. The GOG122 trial also reported that the overall survival of patients receiving adjuvant chemotherapy was better than that of peritoneal disease and residual nodules with stage III or IV total abdominal irradiation <2 cm [6,7]. However, reported no difference between therapies in terms of overall survival in 345 high-risk patients receiving cisplastin, doxorubicin, and cyclophosphamide or external pelvic radiation. Histopathological biomarkers (grade, depth of invasion, histology, lympho vascular space invasion) and patient’s age have been evaluated to define risk strata in patients with early-stage disease, but they have not been used to predict which patients will respond to chemotherapy. As for, this patient, she achieved 5-year-disease free survival following diagnosis of endometriod adenocarcinoma stage 4B treated with adjuvant chemotherapy of doxorubicin and cisplastin with no pelvic lymph node dissection [8-10].
Any role of pelvic lymphadenectomy and oophorectomy for prolonged survival?
As mentioned before, this patient had undergone midline laparotomy Extrafascial hysterectomy bilateral Salpingo oophorectomy in 2011 at the age of 23 years old. She did not have menopausal symptoms following the operation. Oophorectomy is usually included to identify micro metastases in the ovary and to decrease circulating estrogen production, which could theoretically promote the proliferation of metastatic cells outside of the uterus [4]. As for this patient, she developed metastases to the right ovary 3 weeks following the myomectomy. Study revealed that ovarian preservation was associated with improved survival hence decreased risk of cardiovascular death but only if Lynch syndrome was excluded [4]. For this patient, oophorectomy was performed as she developed metastases to the ovary. Meanwhile, National Comprehensive Cancer Network (NCCN) and [11] suggested performing pelvic lymphadenectomy in all patients because the most important prognostic factor in endometrial cancer is nodal involvement.
Conclusion
Although endometrial cancer most commonly occurs in post menopause patients especially in obese patients, it still can occur in young patient. This case also revealed that regular surveillance and discussion with oncologist are essential not only it prolongs survival but also may improve this patient’s quality of life.
Acknowledgement
I would like to express my gratitude to Dr Izzuan Khirman Adnan, my family and my fellow colleagues from O&G Department of Sultanah Bahiyah Hospital, Alor Star Malaysia.
References
- Fadhlaoui A, Hassouna JB, Khrouf M, Zhioua F, Chaker A (2010) Endometrial adenocarcinoma in a 27-year-old woman. Clinical Medicine Insights: Case Reports 3:CCRep-S5346.
- Kim SM, Shin SJ, Bae JG, Kwon KY, Rhee JH (2016) Endometrial adenocarcinoma in a 13-year-old girl. Obstet Gynecol Sci 59(2):152-156.
- Fallowfield L, Jenkins V, Farewell V, Saul J, Duffy A, et al. (2002) Efficacy of a Cancer Research UK communication skills training model for oncologists: A randomised controlled trial. Lancet 359(9307):650-656.
- Brooks RA, Fleming GF, Lastra RR, Lee NK, Moroney JW, et al. (2019) Current recommendations and recent progress in endometrial cancer. CA: Cancer J Clin 69(4):258-279.
- Sovak MA, Hensley ML, Dupont J, Ishill N, Alektiar KM, et al. (2006) Paclitaxel and carboplatin in the adjuvant treatment of patients with high-risk stage III and IV endometrial cancer: A retrospective study. Gynecol Oncol 103(2):451-457.
- Hsiao SM, Wei LH (2011) Controversies in the adjuvant therapy of endometrial cancer. ISRN Obst Gynecol 1-4.
- Nout RA, Putter H, Schultz IM, Jobsen JJ, Lutgens LC, et al. (2007) 5000 ORAL Quality of life after radiotherapy for endometrial cancer: First results from the randomized PORTEC-2 trial. EJC Supplements 4(5):311.
- Masciullo V, Amadio G, Lo Russo D, Raimondo I, Giordano A, et al. (2010) Controversies in the management of endometrial cancer. Obstet Gynecol Int 1-7.
- Rauh-Hain JA, Del Carmen MG (2010) Treatment for advanced and recurrent endometrial carcinoma: Combined modalities. Oncologist 15(8):852.
- Gottwald L, Pluta P, Piekarski J, Spych M, Hendzel K, et al. (2010) Long-term survival of endometrioid endometrial cancer patients. Archives of Medical Science: AMS 6(6):937.
- Ayhan A, Taskiran C, Celik C, Yuce K (2004) The long-term survival of women with surgical stage II endometrioid type endometrial cancer. Gynecol Oncol 93(1):9-13.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences