A Case Report of Cure of Acromegaly after Pituitary Apoplexy
Husain Taha Rhadi*, Ebtihal Yusuf and Eman Ebrahim
Department of Endocrinology, Salmanyia Medical Complex, Ministry of Health, Bahrain
- *Corresponding Author:
- Husain Taha Rhadi
Departement of Endocrinology
Salmanyia Medical Complex
Ministry of Health, Bahrain
Tel: +973 39639960
E-mail: husaintaha74@yahoo.com
Received Date: October 11, 2017; Accepted Date: October 25, 2017; Published Date: November 01, 2017
Citation: Rhadi HT, Yusuf E, Ebrahim E (2017) A Case Report of Cure of Acromegaly after Pituitary Apoplexy. J Clin Med Ther. 2:26.
Abstract
Pituitary apoplexy is a rare life threatening condition. Clinical manifestation cause acute severe headache, fever, impaired conscious level, ocular palsies, visual disturbance and signs of meningeal irritation. Presentation can mimic and misdiagnosed as meningitis. Here, we report a 33-year- old man who was suspected to have pituitary macroadenoma causing acromegaly due to clinical features and high IGF-1. He presented with severe headache, fever, impaired conscious level, and left ocular palsy. Laboratory data showed leukocytosis and neutrophils pleocytosis in cerebrospinal fluid. Bacterial meningitis was suspected, so he was kept on antibiotics and dexamethasone with quick improvement. Magnetic resonance imaging showed necrotic pituitary macroadenoma and laboratory test confirmed resolution of acromegaly, which was confirmed by normalization of IGF-1 and was kept on Octerotide. He was remained hypopituitarism and kept on replacement. On further follow up, MRI showed marked regression of pituitary adenoma. Whether he really had meningitis which lead to apoplexy or it was pituitary apoplexy mimicking meningitis is questionable. There is a bidirectional relationship between pituitary apoplexy and meningitis. This case adds the importance fact of keeping the differential diagnosis in mind in patients with pituitary adenoma who presents with acute neurological symptoms.
Keywords
Pituitary apoplexy; Acromegaly; Meningitis
Introduction
Acromegaly is a disorder caused by overproduction of growth hormone from anterior pituitary gland. Excessive growth hormone leads to overproduction of insulin like growth factor 1 (IGF-1) which causes multisystemic disease characterized by overgrowth of body tissues, metabolic dysfunction, multiple comorbidities and mortality. This condition has an incidence of 3-4 cases per million and prevalence of 60 cases per million [1]. Only few patients with acromegaly seek medical opinion for the change in appearance and extremities enlargement. However, they are more often present due to systemic comorbidities or local tumour effects [2]. Pituitary apoplexy is a rare condition. It results from infarction or haemorrhage into a pre-existing pituitary adenoma. It causes significant morbidity. It is life-threatening condition as it can lead to cardiovascular collapse and endocrine crises. It often presents with acute severe headache, visual field defects, ocular palsies and hypopituitarism. The diagnosis of this condition is challenging because it can resemble other intracranial pathologies in its presentation such as meningitis [3]. Associated meningeal irritation signs in pituitary apoplexy cases are rare and usually not reported as presenting signs. In the literature, there are only few cases presented with pituitary apoplexy after meningitis [4-5], but there is more reported case of misdiagnosis of pituitary apoplexy as meningitis [6-10]. Depending on the severity of the symptoms and signs, conservative or surgical treatment is recommended. Surgical intervention is recommended for patients with visual field defects and ocular palsy. Treatment may be unnecessary in some cases as the pituitary tumour can spontaneously regress [11]. There have been several reports describing cases of regression of pituitary adenomas and cure of acromegaly after pituitary apoplexy [12-14]. We present a case of a patient who developed remission of acromegaly and regression of pituitary macroadenoma after presenting with pituitary apoplexy which resembled meningitis or it was a consequence of meningitis.
Case Report
A 33 years old male was referred to the endocrinology clinic after his dermatologist suspected acromegaly because of recurrent cystic acne along with distinct signs and symptoms of acromegaly. He had a history of diabetes mellitus which was poorly controlled on oral hypoglycemic agents for the last 4 years. The patient’s main concern was about treating acne. He was not aware of any other changes in his appearance. Although he was having prominent supraorbital edges, nasal bone hypertrophy, tooth separation and enlarge hands and feet. The laboratory tests had shown an elevated growth hormone (GH) and insulin-like growth factor I (IGF-1) levels (Table 1).
| Variable | Result | Reference range | units | ||
|---|---|---|---|---|---|
| On presentation | After apoplexy | Follow up | |||
| GH | >40 | 0.4 | 0.2 | <5 | mcg/L |
| IGF-1 | 1529 | 134 | 124 | 116-352 | mcg/L |
| 8 am cortisol | 653 | <13 | 59 | 138-690 | nmol/L |
| TSH | 1.5 | 0.24 | 0.71 | 0.30-5.00 | mlU/L |
| Free T4 | 22.7 | 9.8 | 10.1 | 8.0-24 | pmol/L |
| LH | 5.5 | 0.3 | 0 | 1.5-6 | IU/L |
| FSH | 5.3 | 0.8 | 0.6 | 1.6-11 | IU/L |
| Testosterone | 13.1 | 0.71 | 18 | 9.0-40.0 | nmol/L |
| Prolactin | 11.4 | 1.76 | 2 | 2.7-16.8 | ng/mL |
| Na | 139 | 129 | 138 | 136-145 | mmol/L |
| HbA1C | 78 | 69 | 49 | 29-42 | mmol/mol |
Table 1: Biochemical results upon presentation, after apoplexy and on subsequent follow up.
At that point Magnetic resonance imaging scan (MRI) has been advised, but he refused to do it because of his claustrophobia despite adequate explanation and offering it to be done under sedation. His subsequent visit to endocrinology clinic after 8 months, he complained of generalized weakness, fatigue, dizziness and significant weight loss. He has been found to have postural hypotension, pallor, and he looked unwell.
On further detailed history, the patient stated that he was admitted to the hospital during the preceding month. His medical documents were reviewed and it showed that he was admitted under neurology care after he got a severe form of sudden headache associated with fever. He was having impaired level of consciousness, signs of meningeal irritation, double vision and left VI nerve palsy.
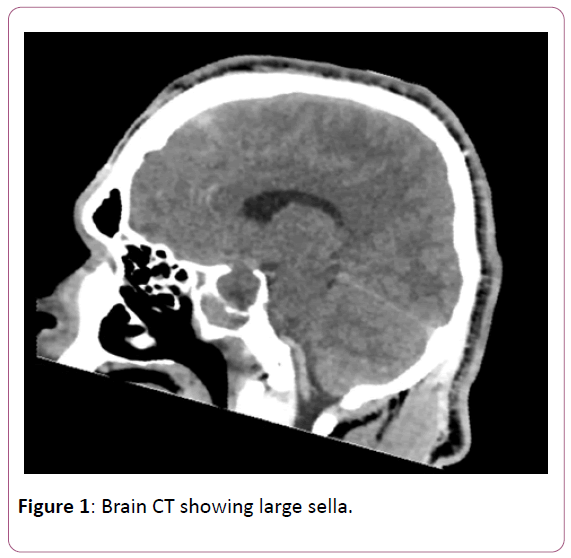
Laboratory data showed leukocytosis and neutrophils pleocytosis in cerebrospinal fluid. He was managed as bacterial meningitis with antibiotics and intravenous dexamethasone. CT Brain does not showed any significant meningeal changes, however there is a note that sella was enlarged (Figure 1).
Figure 1: Brain CT showing large sella.
MRI was arranged during his hospital stay, but was failed to be done due to claustrophobia. Pituitary apoplexy has been suspected. Laboratory studies were requested to rule out pituitary dysfunction and results confirmed hypopituitarism (Table 1).
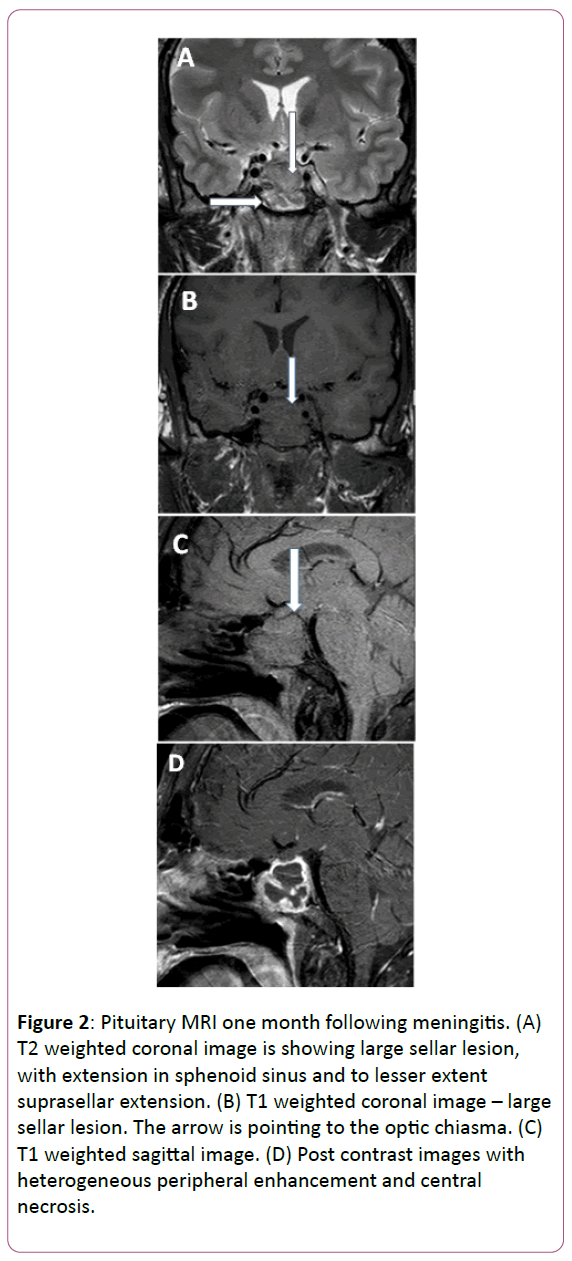
MRI was done after patient’s acceptance. It showed pituitary macroadenoma with necrosis (Figure 2). That confirmed the diagnoses of pituitary apoplexy occurring in pituitary macroadenoma. He was put on replacement with hydrocortisone, levothyroxine, and sex hormone, and he is maintained on Octreotide to prevent the regrowth of the adenoma.
Figure 2: Pituitary MRI one month following meningitis. (A) T2 weighted coronal image is showing large sellar lesion, with extension in sphenoid sinus and to lesser extent suprasellar extension. (B) T1 weighted coronal image – large sellar lesion. The arrow is pointing to the optic chiasma. (C) T1 weighted sagittal image. (D) Post contrast images with heterogeneous peripheral enhancement and central necrosis.
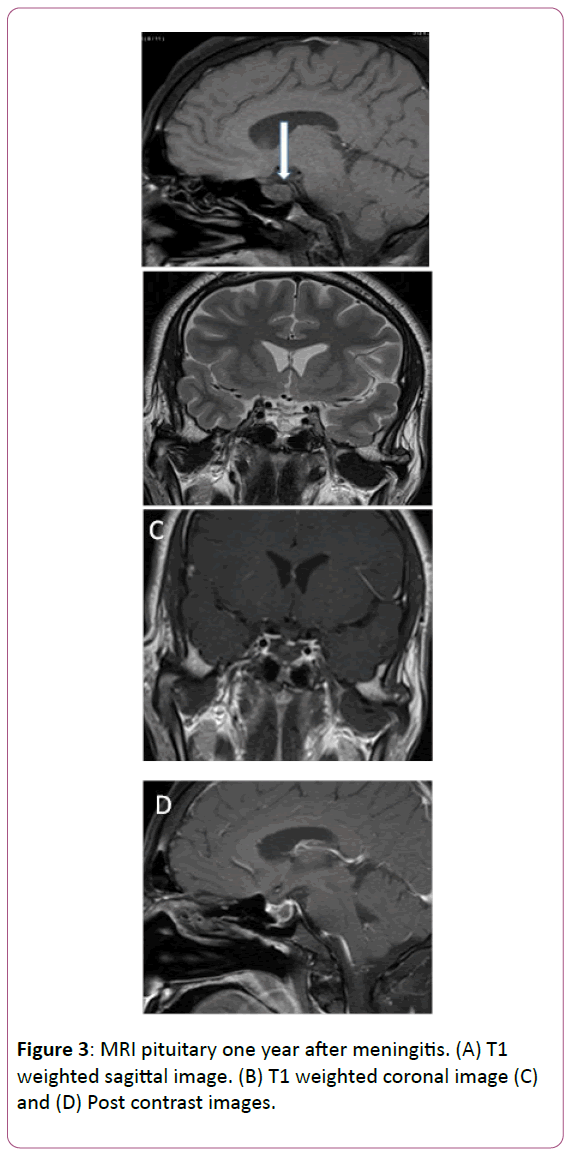
On subsequent follow up, one year after, MRI pituitary was repeated and it showed radiological regression of the size of the previous necrotic macroadenoma (Figure 3). Repeated Laboratory investigation confirmed the remission of acromegaly with normal IGF-1 level and suppressible GH after a 75-g oral glucose tolerance test. However the patient remained in pituitary dysfunction from glucocorticoid, thyroid and gonadal access, but he is on replacement and well controlled. (Tables 1 and 2) Ophthalmological study results are normal. At present he shows marked improvement of signs and symptoms of previous acromegaly including, improvement of glycemic control and improvement of acne.
| Time | 0 time | 60 minutes | 120 minutes |
|---|---|---|---|
| Growth hormone level (mcg/L) |
9.2 | 0.20 | 0.21 |
Table 2: Growth hormone suppression test using 75 G glucose tolerance test, 1 year after pituitary apoplexy.
Discussion
This is an atypical case presenting with regression of growth hormone secreting pituitary adenoma and remission of acromegaly after pituitary apoplexy. The question is whether the patient really had meningitis leading to apoplexy or if apoplexy was misdiagnosed as meningitis. Apoplexy as a consequence of meningitis is rare. In the literature we found only two case reports describing the remission of acromegaly following a presentation of meningitis [4,5]. On the other hand, several case reports have described misdiagnosis of pituitary apoplexy as meningitis [6-10].
The physiology behind the chemical meningitis caused by pituitary apoplexy is due to the release of debris from the sella to the CSF. The patient presents with similar signs and symptoms of meningitis in the form of fever, neck stiffness, and photophobia. The physician will think about pituitary apoplexy rather than meningitis if there is minimal or no response to antimicrobial therapy within the first few days [3].
In this case it is either apoplexy mimicking aseptic meningitis or apoplexy caused by meningitis, both could be possible. Points going with meningitis are: fever, CSF fluid analysis is compatible with bacterial meningitis, clinical response to antibiotic. Points going with apoplexy are: sudden onset of headache, absence of organism in CSF fluid culture, hyponatremia which could be due to hypocortisolism, improvement after dexamethasone, ocular palsy, and decrease level of consciousness.
Radiology differentiating pituitary apoplexy from other neurological conditions requires MRI or CT scan. CT scan is easier to obtain, but MRI is superior to CT for diagnosis of apoplexy because it is more sensitive (sensitivity of 91% for MRI versus 28% for CT) [15]. The underlying mechanism that cause the disappearance or regression of a pituitary adenoma following apoplexy is poorly understood. Rapid enlargement of a pituitary tumour resulting in compression of surrounding structures, potentially causing pituitary insufficiency is the contributing mechanism [16]. Head trauma, pregnancy, thrombocytopenia, anticoagulant therapy, increased intracranial hypertension, dopamine agonist therapy, radiotherapy, diabetes mellitus, upper respiratory tract infection, meningitis, coronary artery bypass surgery, carotid angiography, and hypophyseal dynamic testing are all documented triggering factors for pituitary apoplexy in the literature [17]. In this case, predisposing factors could be diabetes mellitus or meningitis or both.
Most of the patients who experience pituitary apoplexy will be asymptomatic later on and only minority of them will have minor disabilities. It is published in several case reports 60% were asymptomatic and 19% were with minor disabilities. Monitoring of hormones is essential in these cases and more than of 50% of those patients will require hormones replacement therapy following pituitary apoplexy [15]. Recently, apoplexy prognosis has been improved dramatically. Neurosurgical intervention for the pituitary apoplexy in the acute stage is not mandatory for all patients. Conservative management can lead to complete recovery in some cases [18]. Recurrence of tumor is always a possibility because even if the MRI shows complete disappearance of the adenoma, some tumor cells may not have been fully destroyed, so those patients will require continuous follow up.
In conclusion, pituitary apoplexy can mimic meningitis, however meningitis can cause pituitary apoplexy, This fact high lights the importance of keeping in mind the differential diagnosis in patients with pituitary macroadenoma who present with acute neurological symptoms.
Informed Consent
Yes
References
- Melmed S (2006). Medical progress: acromegaly. N Engl J Med 355: 2558e73.
- Vilar L, Vilar C, Lyra R, Lyra R, Naves L (2016) Acromegaly: clinical features at diagnosis. Pituitary 20: 22-32.
- Jankowski P, Crawford J, Khanna P, Malicki D, Ciacci J, et al. (2015) Pituitary Tumor Apoplexy in Adolescents. World Neurosurgery 83: 644-651.
- Katsuno M, Yamazaki M, Tahara S, Murai Y, Teramono A, et al. (2003) Spontaneous remission of acromegaly after meningitis: a case report. No to Shinkei 55: 967-971.
- Villar-Taibo R, Ballesteros-Pomar M, Vidal-Casariego A, Álvarez-San Martín R, Kyriakos G, et al. (2014) Spontaneous remission of acromegaly: apoplexy mimicking meningitis or meningitis as a cause of apoplexy? Arquivos Brasileiros de Endocrinologia & Metabologia 58: 76-80.
- Valente M, Marroni M, Stagni G, Floridi P, Perriello G, et al. (2003) Acute sterile meningitis as a primary manifestation of pituitary apoplexy. J Endocrinological Investigation 26: 754-757.
- Jassal D, McGinn G, Embil J (2004) Pituitary Apoplexy Masquerading as Meningoencephalitis. Headache: The J Head and Face Pain 44: 75-78.
- Smidt M, Van der Vliet A, Wesseling P, De Vries J, Twickler T, et al. (2007) Pituitary apoplexy after mild head injury misinterpreted as bacterial meningitis. European J Neurology 14: e7-e8.
- Huang W, Chien Y, Wu C, Weng W, Peng T, et al. (2009) Pituitary adenoma apoplexy with initial presentation mimicking bacterial meningoencephalitis: a case report. The American J Emergency Medicine 27: e1-517.e4.
- Paisley A, Syed A (2012) Pituitary apoplexy masquerading as bacterial meningitis. Canadian Medical Association J 184: 1812-1812.
- Tu M, Lu Q, Zhu P, Zheng W (2016) Surgical versus non-surgical treatment for pituitary apoplexy: A systematic review and meta-analysis. J the Neurological Sciences 370: 258-262.
- Fraser L, Lee D, Cooper P, Van Uum S (2009) Remission of Acromegaly After Pituitary Apoplexy: Case Report and Review of Literature. Endocrine Practice 15: 725-731.
- Chentli F (2012). Cure of Acromegaly and Diabetes Mellitus After Pituitary Apoplexy. Acta Endocrinologica (Bucharest) 8: 113-118.
- Qurttom M, Seshadri M (1995) Spontaneous Remission of Acromegaly After Pituitary Apoplexy. Annals of Saudi Medicine 15: 191-192.
- Sibal L, Ball S, Connolly V, James R, Kane P, et al. (2004) Pituitary Apoplexy: A Review of Clinical Presentation, Management and Outcome in 45 Cases. Pituitary 7: 157-163.
- Baruah M, Ranabir S (2011) Pituitary apoplexy. Indian J Endocrinology and Metabolism 15: 188.
- Vidal E (1992) Twelve cases of pituitary apoplexy. Archives of Internal Medicine 152: 1893-1899.
- Santos A, França M, Hirosawa R, Marivo M, Zanini M, et al. (2011) Conservative management of pituitary tumor apoplexy. Arquivos Brasileiros de Endocrinologia & Metabologia 55: 345-348.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences