Abstract
The Effects of Hepatic Ischemia-Reperfusion Injury on Postoperative Cognitive Function in Elderly Patients
Background: Surgical trauma, such as hepatic ischemiareperfusion (HIR), resulting in the release of peripheral pro-inflammatory cytokines into the brain to affect neurocognitive function, is a prominent risk factor for the development of postoperative cognitive dysfunction (POCD). Methods: Forty patients of partial hepatectomy were divided into two groups: hepatic ischemia-reperfusion group (Group I/R) and control group (Group C). Each group had 20 individuals. Hepatic portal was clamped in the process of partial hepatectomy in the patients of Group I/R, otherwise in the Group C did not block Hepatic portal. Blood sample was collected on the 1th day before surgery and 4th days after surgery respectively, and then the contents of IL-6, TNF-α, S100β protein, AST and ALT were detected by ELISA kit. Neuropsychological tests were performed according Murkin’s standard on the 1th day before surgery and the 4th day, and Z score was counted and used to identify the occurrence of POCD. Result: On the 4th days after surgery, the serum level of IL-6, TNF-α and S100β in the Group I/R patients significantly increased comparing with Group C (P<0.05). Psychological evaluation was performed, and found that Z score was more than 1.96 in 4 patients among Group C, while there were 11 patients in Group I/R. The incidences of POCD in Group I/R were 55%, and obviously higher than 16% in Group C. The incidence of POCD was correlated with serum levels of IL-6, TNF-α and S100β in Group I/R patients. Conclusion: Our results demonstrated that hepatic ischemia-reperfusion in the partial hepatectomy increased the incidence of POCD in elder patients, which was correlated with the elevated levels of IL-6, TNF-α and S100β in peripheral blood.
Author(s): Yiqiao Wang, Lina Hao, Pei Gao, Zhenhua Ren and Yuanhai Li
Abstract | Full-Text | PDF
Share This Article
Google Scholar citation report
Citations : 131
Journal of Surgery and Emergency Medicine received 131 citations as per Google Scholar report
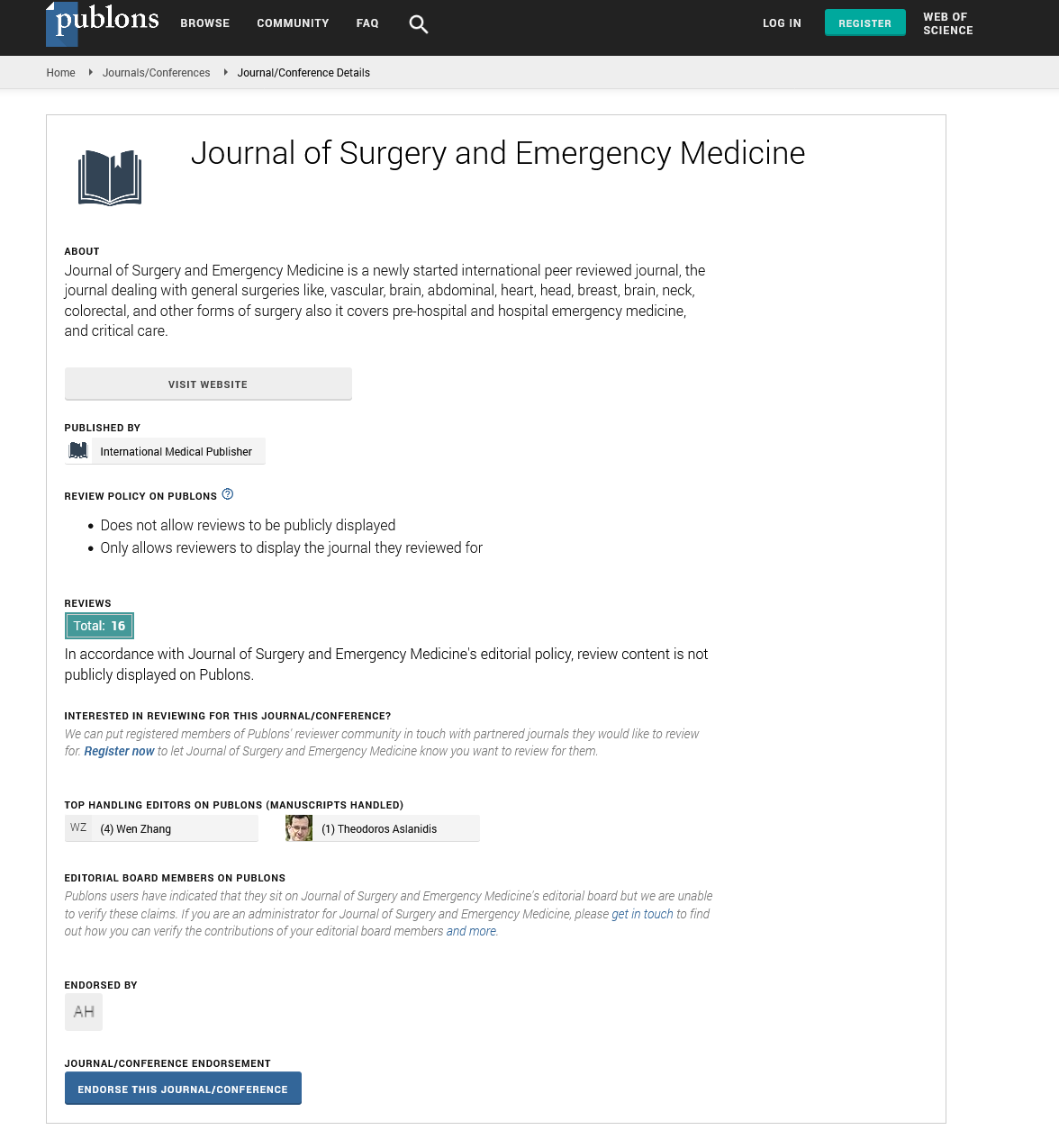
Journal of Surgery and Emergency Medicine peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences