Abstract
BET protein inhibition prolongs cardiac transplant survival via enhanced myocardiac autophagy
Graft rejection remains a major barrier to long-term engraftment after transplantation. Autophagy plays an important role in cardiac ischemia reperfusion and cardiac injury pathogenesis. The bromodomain and extraterminal protein inhibitor JQ1 inhibits inflammatory responses. However, the beneficial effect of JQ1 on transplant tolerance and the potential role of autophagy in the protective effect of graft survival have yet to be investigated. Our study revealed that JQ1 treatment evidently prolonged cardiac allograft survival, but LKB1 deficiency among donors eliminated the tolerogenic effect of JQ1. JQ1 increased the expression levels of LKB1, ATG5, and LC3-II and potentiated the phosphorylation of AMP-activated protein kinase (AMPK), ULK1, and ATG14 in the allografts. A conditional ATG5 deletion donor was utilized to abrogate transplant tolerance induced by JQ1. The combined use of JQ1 with Bafilomycin A1 partially reversed the tolerogenic effect of JQ1, suggesting that autophagy is involved in the signaling pathway in graft survival. JQ1 decreased the frequencies of Th1, Th2, Th17, and regulatory T cells in vitro and downregulated the expression of inflammatory cytokines, such as IL-2, IL-6, IL-1β, TNF-α, IFN-γ, and IL-17, but JQ1 could not prevent CD4+ and CD8+ T cell activation in vivo. Thus, JQ1 prolonged cardiac allograft survival by potentiating myocardiac autophagy through the LKB1-AMPK-ULK1 signaling pathway and inhibiting the subsequent release of inflammatory cytokines. This result might provide novel insights into transplant tolerance induction.
Author(s): Weihua Gong
Abstract | PDF
Share This Article
Google Scholar citation report
Citations : 131
Journal of Surgery and Emergency Medicine received 131 citations as per Google Scholar report
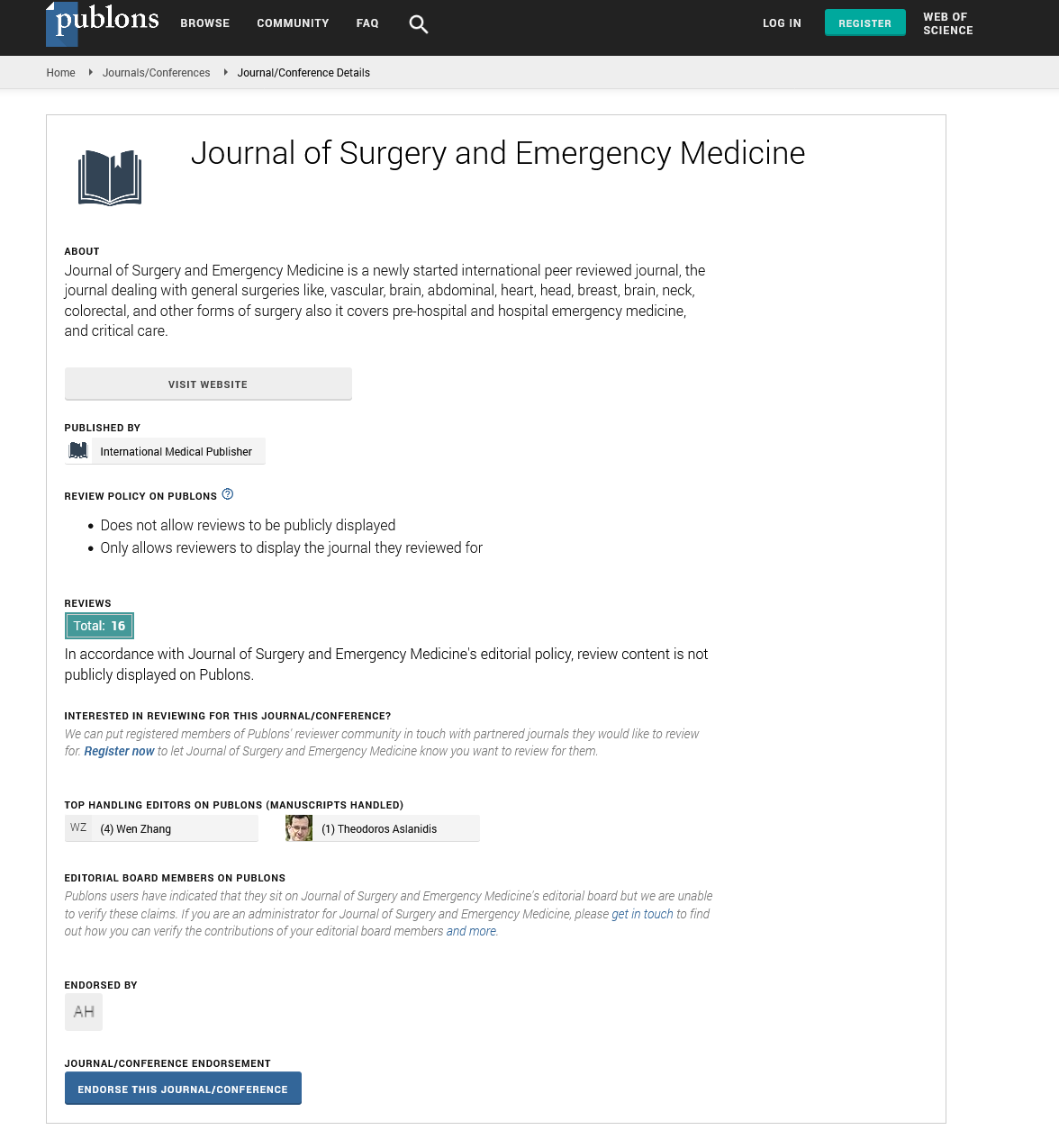
Journal of Surgery and Emergency Medicine peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences