Vertebroplasty: Review of the Procedure in Relation to Patients with Fracture of Osteoporotic Origin
Department of Neurosurgery, Hospital General Universitario de Valencia, Valencia, Spain
- *Corresponding Author:
- Inaki Arrotegui,
Department of Neurosurgery
Hospital General Universitario de Valencia
Valencia, Spain
Tel: 034627492961
E-mail: athbio@yahoo.es
Received date: Jul 26, 2018; Accepted date: Jul 30, 2018; Published date: Aug 07, 2018
Citation: Arrotegui I (2018) Vertebroplasty: Review of the Procedure in Relation to Patients with Fracture of Osteoporotic Origin. J Surgery Emerg Med 2: 555.
Copyright: © 2018 Arrotegui I. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Vertebroplasty was initially described by Gallibert and cols. in 1987 to treat symptomatic hemangiomas of the vertebral body. Percutaneous vertebroplasty (PV) is a minimally invasive technique used to reinforce pathological vertebral bodies. It is indicated in symptomatic hemangiomas, vertebral fractures due to osteoporosis and vertebral involvement due to metastasis or multiple myeloma with bone destruction and risk of spinal and/or root involvement. The efficacy of VP is based on its analgesic effect, in addition to preventing vertebral fractures and, in the event of a vertebral fracture already existing, the VP prevents its progression. The technique involves the injection of methyl-methacrylate cement (M-M) into the pathological vertebra, in a semiliquid or pasty state so that in a very short time it polymerizes to a solid state, giving a good support to the vertebral body
Keywords
Vertebroplasty; Osteoporosis; Myasthenia gravis; Fluoroscopy
Introduction
Vertebroplasty was initially described by Gallibert and cols. in 1987 to treat symptomatic hemangiomas of the vertebral body [1]. Percutaneous vertebroplasty (PV) is a minimally invasive technique used to reinforce pathological vertebral bodies. It is indicated in symptomatic hemangiomas, vertebral fractures due to osteoporosis and vertebral involvement due to metastasis or multiple myeloma with bone destruction and risk of spinal and/or root involvement. The efficacy of VP is based on its analgesic effect, in addition to preventing vertebral fractures and, in the event of a vertebral fracture already existing, the VP prevents its progression. The technique involves the injection of methyl-methacrylate cement (M-M) into the pathological vertebra, in a semiliquid or pasty state so that in a very short time it polymerizes to a solid state, giving a good support to the vertebral body. When hardened within the cancellous bone of the pathological vertebra, the M-M cement increases the resistance of the vertebral body, which prevents the progression of the fracture thereof and produces an analgesic effect [2]. In addition to the mechanical effect produced by cement, it also performs two other actions: the first is the thermal effect, due to the polymerization process that releases a large amount of heat, destroying the tumor cells in the event of neoplastic infiltration. The second action is the cytotoxic effect of M-M on cells in direct contact with cement, described in previous investigations.
The cement was used for the first time in 1960 in hip surgery [3], whereas in 1984 Galibert first described vertebroplasty by direct injection. In 1985 Galibert and Deramond described the VP and since then the use of cement M-M in medicine has been increased and the indications of VP have expanded. Initially VP was used for the treatment of aggressive vertebral hemangiomas with pain, expansion and bone destruction. Currently, its application has been extended to tumor pathology such as metastasis and multiple myeloma as palliative and adjuvant treatment with radiotherapy, chemotherapy and surgery. Another main indication of the technique is fracture due to osteoporosis that does not respond to the usual conservative treatment.
Pathology
Osteoporosis
The functional disability of patients with osteoporosis is due to vertebral and hip fractures. Patients with fractures of one vertebra may be asymptomatic, but in the case of multiple vertebral fractures or hip fractures, their functional capacity may be severely diminished. Some authors have compared older female patients with osteoporosis, and with two or more vertebral fractures with loss of height greater than 25%, with women in similar conditions without fractures. Patients with fractures had functional abilities well below the control group. Functional limitations due to vertebral fractures affected all aspects of everyday life, such as housework, walking, playing sports or driving a car. These limitations appear to increase as the number of fractures increased. Pain in patients with osteoporosis can be acute and is usually due to recent fracture, although there are vertebral fractures without acute pain. The painful symptoms of vertebral fractures usually disappear at 4-6 weeks if there is no medullar or radicular involvement. The usual treatment of acute pain due to vertebral fracture consists of bed rest, local analgesia with cold and heat, massage, nerve root block and physiotherapy, as well as non-steroidal analgesics, myorelaxants. Prolonged bed rest can also aggravate osteoporosis.
Chronic back pain and low back pain in patients with osteoporosis are usually of muscular origin due to contractures due to skeletal deformities. This pain should be treated with physical exercises to strengthen the lumbar muscles and in case of exacerbation with rest, cold-heat, analgesics, muscle relaxants and physiotherapy.
Percutaneous Vertebroplasty
In addition to the invasive surgical techniques, for the repair and stabilization of the injured vertebrae, with the consequent anesthetic and surgical risk and the high cost of the procedure, a new percutaneous technique has been introduced that is much less invasive, less expensive and with very good results positive.
The cement
The cement we use in percutaneous vertebroplasty is MM. There are several brands with the same product and some contain antibiotics. The cement has the following constituents: a) powdered components: gentamicin sulfate, polymethyl methacrylate, benzoyl peroxide, barium sulfate; b) Liquid components: methyl methacrylate, N,N-dimethyl-ptoluidine, hydroquinone. Bone cements do not have adhesive properties [4]. They harden quickly within the bone and when distributed in the cancellous bone they allow to reinforce it and to distribute the weight and other tensions in a regular way [5].
Percutaneous Vertebroplasty Technique
The technique used in VP is the following:
• Positioning of the patient: In cervical lesions, the patient is placed in the supine position, in dorsal lesions in the prone position, while in the lumbar lesions he is placed in the prone or lateral decubitus position.
• Analgesia: The most used in neuroleptoanalgesia, plus local anesthesia. Some authors use general anesthesia.
• Analgesia: The most used in neuroleptoanalgesia, plus local anesthesia. Some authors use general anesthesia.
• Access is usually bilateral, although in some procedures a unilateral puncture is sufficient.
• Injection control: with fluoroscopy.
• Contrast used: tungsten or tantalum in quantity corresponding to 0.5-1 g for each vertebral body. Some authors use barium [6].
Vertebroplasty with transpedicular approach
The patient is placed in the prone position when the lesion is dorsal or lumbar. A peripheral line is taken and the patient is monitored. We proceed to neuroleptoanalgesia. The area of the puncture is localized with the help of fluoroscopy and cleaned with betadine. The patient is covered with sterile drapes leaving the puncture area open. Local anesthesia is performed with novocaine. A small cut is made in the skin with a scalpel blade to facilitate the introduction of the VP needle [7].
Under a fluoroscopic control in anteroposterior projection the pedicle of the affected vertebra is located where the needle is inserted. Then the fluoroscopy is placed on a lateral projection to advance the needle until it reaches the anterior third of the vertebral body. A vertebrography is performed to assess the filling of the vertebra and the possible escape routes of the cement. The cement is prepared. The M-M is first mixed in powder form with the contrast (tungsten or tantalum) and then the methyl-methacrylate is added as a liquid to obtain a paste mixture. The cement is quickly injected into the vertebral body before it solidifies [8].
Some authors use a combination of CT with fluoroscopy to perform the intervention. CT is used to place the needle into the vertebral body and fluoroscopy to control the injection of cement [9].
Contraindications of use
The use of cement is contraindicated in patients with allergy to any of its components. Cements with gentamicin should not be used in the presence of myasthenia gravis or hypersensitivity to gentamicin [10].
Limitations of Vertebroplasty
Vertebroplasty is contraindicated in generalized and localized infections where the procedure has to be performed, in severe alterations of coagulation and cardio-respiratory pathology [11].
Cases - The two patients with symptomatic vertebral fracture have severe back pain after a traumatism or a bad gesture. The pain worsened with the erect position and presented a kyphotic postural attitude in standing (Figure 1).
Figure 1: Osteoporosis Fractures in Theatre.
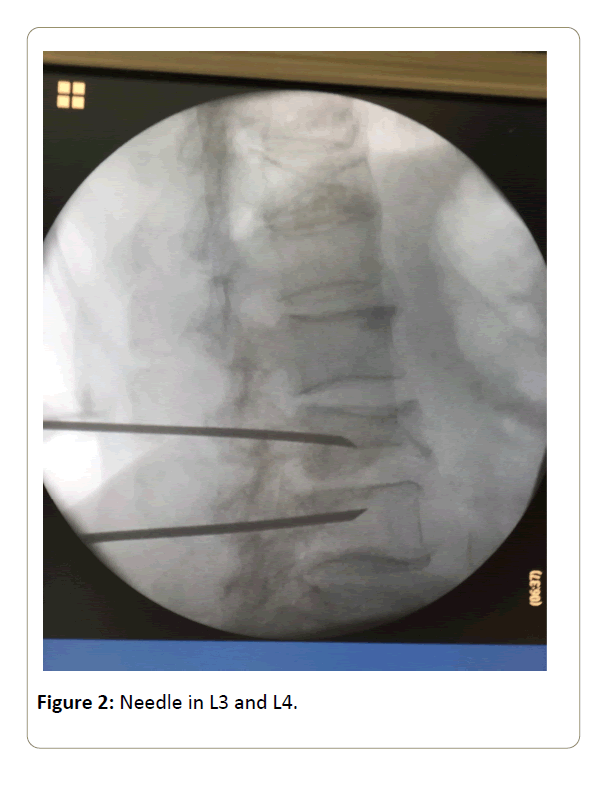
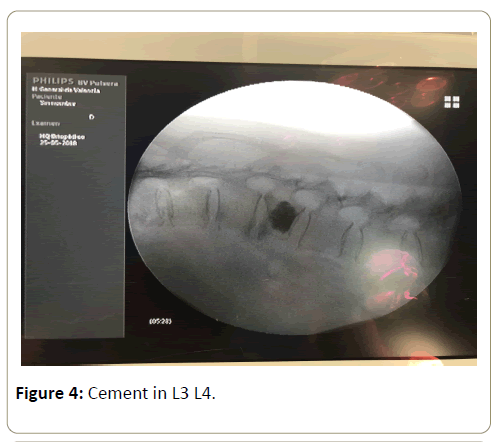
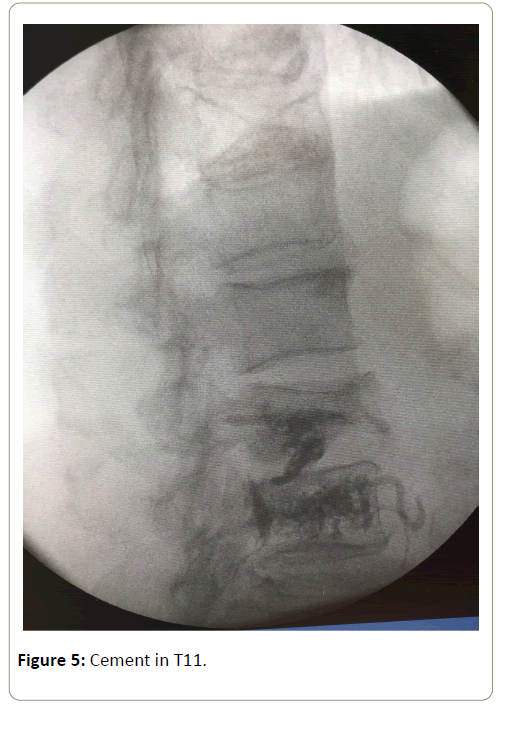
Figures 2 and 3, shows the location of the osteoporotic fractures in T11 (Figure 3) and L3 and L4 (Figure 2), the cementation system of both cases (Figures 4 and 5). After resting for 30 minutes with neurological assessment and monitoring, and when there were no problems, the patients were discharged
References
- Galibert P, Deramond H (1990) La vertébroplastie percutanée comme traitement des angiomes vertébraux et des affections dolorigènes et fragilisantes du rachis. Chirurgie, J Neuroradiol 116: 326-335.
- Onimus M, Schraub S, Bertin D, Bosset JF, Guidet M (1985) Le traitement du cancer secondaire du rachis. Rev Chir Orthop 71: 473-482.
- Benxted JP, Doren CV (1965) Histological changes in the rat bone after varying doses of X rays with particular reference to bone tumour production. Brit J Radiol 38: 261-270.
- Chiras J, Gaston A, Gaveau T, Sellier N, Marsault C, et al. (1979) A study of irradiated bone: histopathologic and physiologic chances. J Nucl Med 20: 142-149.
- Esses, Stephen I (2010) The Treatment of Symptomatic Osteoporotic Spinal Compression Fractures: Guideline and Evidence Report, American Academy of Orthopaedic Surgeons.
- Review of interim funded service: Vertebroplasty and New review of Kyphoplasty (2011) Medical Services Advisory Committee.
- Percutaneous vertebroplasty and percutaneous balloon kyphoplasty for treating osteoporotic vertebral compression fractures (2013) NICE The National Institute for Health and Care Excelence. Health Technol Assess.
- Nicole B, Paul L, Tory MJ (2008) Vertebroplasty and Kyphoplasty.
- Bliemel C, Oberkircher L, Buecking B, Timmesfeld N, Ruchholtz S, et al. (2012) Higher incidence of new vertebral fractures following percutaneous vertebroplasty and kyphoplasty-fact or fiction? Acta orthopaedica Belgica 78: 220-229.
- Wang LJ, Yang HL, Shi YX, Jiang WM, Chen L (2012) Pulmonary cement embolism associated with percutaneous vertebroplasty or kyphoplasty: a systematic review. Orthopaedic Surgery 4: 182-189.
- Wardlaw D, Meirhaeghe VJ (2012) Balloon kyphoplasty in patients with osteoporotic vertebral compression fractures, Expert Review of Medical Devices 9: 423-436.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences