The Dropped Brow Sign in Psychogenic Pseudo-Myasthenic Ptosis
Indiana University School of Medicine, USA
- *Corresponding Author:
- Robert M Pascuzzi
Department of Neurology
Indiana University School of Medicine, USA.
Tel: (317) 963-7415
E-mail: rpascuzz@iupui.edu
Received date: January 31, 2017; Accepted date: February 13, 2017; Published date: February 20, 2017
Citation: Pascuzzi RM, King JL. The Dropped Brow Sign in Psychogenic Pseudo-Myasthenic Ptosis. Ins Ophthal. 2017, 1:1.
Abstract
In patients presenting with eyelid ptosis the clinician considers a differential diagnosis of 3rd nerve palsy, Horner’s syndrome, mitochondrial myopathy, oculopharyngeal muscular dystrophy, levator dehiscence, myotonic dystrophy and myasthenia gravis. The presence of moment to moment fluctuation in severity of ptosis (fatigable ptosis) typically suggests a neuromuscular junction disorder of which myasthenia gravis is the only common form. Patients may also present with symptoms or signs that are psychological in origin. We present a case of ptosis associated with the “dropped brow sign” (initially misdiagnosed as myasthenia gravis). This finding is evidence for psychogenic pseudo-myasthenic ptosis and should direct the clinician towards early exploration of a psychological component to the patient’s symptoms. Evaluation and management options for psychogenic disorders are summarized herein with a focus on recommendations for psychotherapy approaches that include the Creative Arts Therapies treatment and research potentials.
Introduction
The following patient presented with fluctuating upper eyelid ptosis in the setting of longstanding generalized weakness.
Case Report
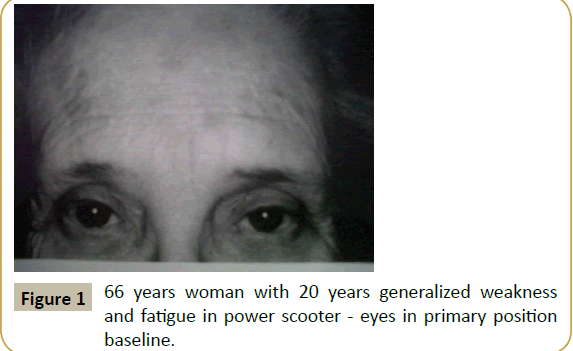
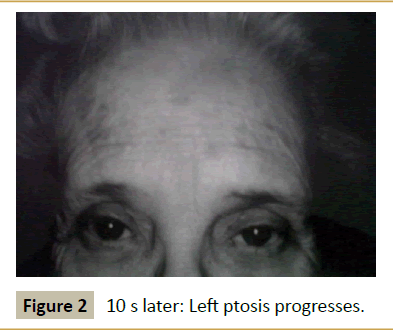
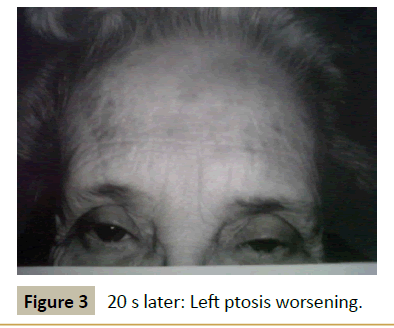
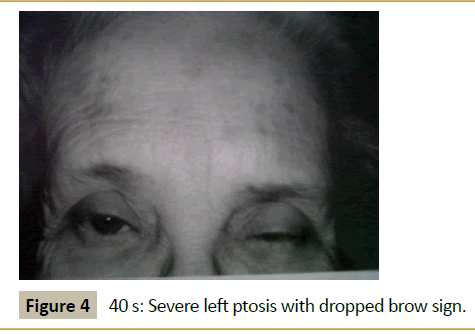
A 66 year old woman presented with a 20 years history of fluctuating droopy eyelids, double vision, impaired chewing and swallowing, weakness of the arms and legs and subjective dyspnea. She had dependency on a power scooter for 10 years. Past medical history was notable for hypertension, hypothyroidism, and hypercholesterolemia all optimally treated. She also had a 20 years history of gastrointestinal symptoms of nausea, indigestion, and loose stools without a clear diagnosis in spite of thorough evaluation. Examination revealed the patient to be tearful and frustrated with the chronic nature of her disabling symptoms and with her perceived lack of help from the physician community. Neurological examination revealed normal mental status screen (no dementia) and normal screening of sensation, cerebellar function, and reflexes. Station and gait was characterized by weakness with standing requiring assistance from the examiner. Cranial nerve testing was notable for asymmetrical ptosis as shown in Figures 1-4. The patient had had full range of motion in testing extraocular motility. She demonstrated shaky giveaway weakness when testing masseter, neck flexor and neck extensor muscles. And there was inconsistent giveaway weakness upon formal testing of proximal and distal limb muscles. Muscle tone and bulk were normal. Her voice was intermittently soft in volume and at times she would whisper but articulation was normal.
During the course of the patient’s history and exam her ptosis would fluctuate from moment to moment as demonstrated in the Figures 1-4.
Based on a 20 years history of fluctuating cranial and limb weakness a diagnosis of myasthenia gravis was pursued. In that regard she was administered an unblended edrophonium test and noted immediate improvement in all symptoms and several minutes of resolution of her ptosis. The patient who was distraught frustrated and tearful was reassured that she had myasthenia gravis and treatment was initiated. Serological testing for acetylcholine receptor antibodies was normal (80% sensitivity). Repetitive stimulation of limb and facial nerves showed no decrement of the corresponding compound muscle action potential (CMAP) and thus was normal. Routine nerve conduction studies and EMG needle exam were normal. She underwent single fiber EMG recording of the right extensor digitorum communis muscle and also the right frontalis muscles and these studies were normal (>95% sensitivity).
Based on the history and examination and benefit from edrophonium a diagnosis of myasthenia gravis was made and the patient was treated with pyridostigmine [1]. She initially improved but still could not ambulate nor perform ADLs independently. Thus she was treated with prednisone initially 60 mg daily with marked improvement in symptoms and function on the 1st day of treatment. Cranial symptoms and function appeared normal, ptosis resolved, and she could walk independently without need for her power scooter. Over the next few weeks her improvement declined and her original symptoms recurred. She was gradually taken off of corticosteroids over several months.
For the next 20 years she has remained in similar clinical status with symptoms of her initial presentation including variable degrees of fluctuating ptosis as in the figure. During that time additional serological testing for MuSK antibodies as well as repeat single fiber EMG have been consistently normal. Over time the physician team concluded that her symptoms and exam represented manifestations of anxiety and conversion. Although she was informed that the diagnosis of myasthenia gravis was incorrect she remained convinced and concerned that this was in face her diagnosis and for many years the office visits would involve further discussion of myasthenia based on her concerns and questions. She refused consultation with psychiatry and never fully accepted the diagnosis of a psychological cause for her symptoms.
Discussion
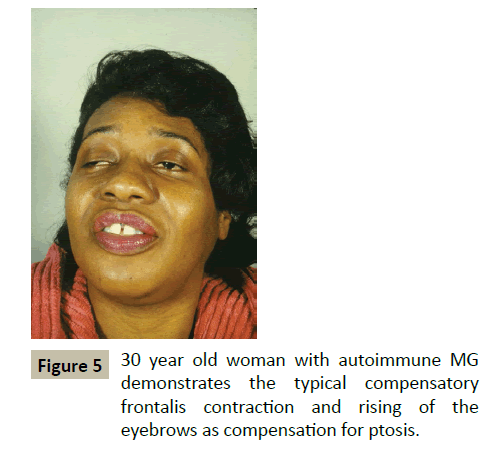
All experienced clinicians recognize the occurrence and challenges of patients in whom it is difficult to distinguish organic from psychological causation. Fullerton reported the presentation of conversion symptoms mimicking myasthenia gravis in 1966 [2]. This patient presented with painless fluctuating cranial and limb weakness including ptosis. While the history suggests myasthenia gravis the patient’s evaluation failed to reveal evidence to validate that diagnosis. The presence of inconsistent giveaway weakness indicates a non-myasthenia etiology to her symptoms. The purpose of this report is to emphasize the features of this patient’s fluctuating ptosis as being more diagnostic for pseudoptosis as opposed to myasthenia gravis. The serial pictures of the patient’s ptosis demonstrate that the left eyebrow drops with increasing upper lid ptosis. This phenomenon of the dropped brow is opposite to the typical behavior and position of the brow in true myasthenic ptosis. More typically the myasthenic patient will contract the frontalis muscle and elevate the brow as compensation for involuntary ptosis (Figure 5). In patients in whom the brow drops with increasing ptosis it behooves the clinician to consider a psychological cause for the patients symptoms. In recognizing this pattern of ptosis it should allow the clinician to be cautious about labeling the patient with a diagnosis myasthenia gravis, the treatment for which can be associated with significant risks and costs (such as from long term prednisone therapy). In patients with the dropped brow sign and fluctuating ptosis a strong consideration for psychological causes is justified. While the current patient appeared to have anxiety and marked life-long stress and appeared to have a conversion of her stresses at an unconscious level thus creating her generalized weakness and inability to function, it is also the case that patents who are malingering may present with a similar examination finding. The presence of a transient favorable response to intravenous edrophonium is insufficient to establish a diagnosis of MG. A control injection with double blinding would improve the use of this test and would have been revealing in this patient [3].
Patients with psychological ocular symptoms include not only those with ptosis but also those with impairment of extraocular motility and associated diplopia. Convergence spasm can mimic myasthenic weakness and serve as a source of potential diagnostic error. Inconsistent eye movement findings, resolution with distraction. Volitional ptosis is often associate with lowing of the upper id and rising of the lower lid. Shaky twitchy movements of the lids are unlikely to be related to myasthenia.
Psychiatric disorders in MG are common, especially depression and anxiety. Ybarra observed 26% of MG patients were diagnosed with a depressive disorder and 46 were diagnosed with anxiety [4].
Management of psychological causes for weakness including those primarily ocular remains challenging as with the spectrum of psychological disorders including, anxiety, depression, conversion, somatization and also those with malingering [5, 6]. Diagnostic criteria, access to healthcare professionals with optimal management skills and programs can be difficult to identify and acquire for such patients. Communication between the physician and patient is central to a favorable outcome. Access to skilled counseling, psychology, psychiatry, and creative arts therapy is instrumental in finding resolution. Formal neuropsychological testing can provide major objective evidence in support of severe depression, anxiety, somatization and states of conversion that allow for a more compelling discussion with the patient as to the need for serious psychological intervention based on an objective test.
There are four distinct groups of patients that the clinician may face in this clinical context. One group has myasthenia gravis which is producing the primary ophthalmological and neurological symptoms and is treated accordingly. The second group has primarily psychologically sourced symptoms and the management must focus on the behavioral and psychological status of the patient. The third group has both - a combination of organic myasthenic symptoms with superimposed psychological weakness ocular or generalized. The author has seen patients with and without underlying myasthenia who have decompensated from a psychological perspective and become hospitalized in the intensive care , intubated, mechanically ventilated, treatment with plasma exchange, IVIg, high dose corticosteroids without objective support for their weakness being myasthenic (these patient have had psychological causes for their decompensation). The fourth group represent patient who have myasthenia gravis. And they have significant stress and psychological conditions that appear to exacerbate their myasthenia. Thus they do not have psychogenic weakness, but they have psychological causes for their myasthenia gravis to worsen. Zou et al. established preoperative anxiety as a risk factor for MG patients developing a post-thymectomy exacerbation of weakness (crisis) [7].
Management is best team oriented with optimal assessment and understanding of the myasthenic component along with specialized professional management from the psychological direction. Communication and collaborative management is needed to assure optimal outcome.
It is difficult for patients to fully grasp why it is that they experience physical and psychological distress. Emotions, memories and perceptions are often stored in less accessible areas of the psyche, especially when associated with traumatic experiences. It is important for the treatment team to recognize this natural human propensity to split off disturbing impulses from direct consciousness and understands more fully how these energies may manifest in psychogenic and stress related symptoms. Contemporary medical practice has a responsibility to approach patients from a holistic perspective and work towards understanding the connections between physical symptoms and underlying psychological stressors, which often requires an approach that moves beyond the linear communication afforded through only words and Cognitive-Behavioral techniques. Nonverbal and symbolic communication afforded through the creative arts therapies helps to facilitate the expression of less conscious experiences that influence the development of physical symptoms.
Psychology, Reflection, Coping and Meaning in the Management of Myasthenia Gravis: There is currently no evidence-based practice for treating people with MG or their caregivers, and no specific psychological method of treatment that addresses coping skills or the consequent development of psychological conditions such as depression and anxiety. While the latter symptomatology may very well be a healthy response to a chronic neuromuscular disorder, adapting a whole person perspective to the illness is essential for optimal treatment. Issues of coping, helplessness and fear of life-threatening weakness likely effect quality of life, impact on the relationships of those involved in care and the capacity to tolerate and process questions of meaning and purpose. And in some cases fear and anxiety may predict a lifethreatening exacerbation of MG [7].
Effective psychotherapy traditionally occurs within the context of the therapeutic relationship, and it is through the expression of the patients that those responsible for treatment can more fully understand the experiences and needs of the people involved. Oftentimes the capacity to verbally express emotions is limited; a natural phenomenon that is exacerbated in times of high stress and traumatic experiences [8]. The use of nonverbal, sensorybased and expressive therapies may provide opportunity to understand more clearly the lived experience of those affected with MG and their caregivers.
Art therapy is a master’s level medical and healthcare profession that uses the creative process, art media, and the resulting products to help patients explore their feelings, develop coping skills, decreases identified symptoms and improve/restore functioning within the context of the therapeutic relationship [9]. Art therapists work with all ages and in a variety of healthcare settings to help patients understand and symbolically express elements of their psychic functioning so that cognitive processing of personal experiences is less threatening, more objective and thus easier to identify and understand.
Art therapy has shown to be effective in stress reduction and anxiety, along with helping caregivers accept the reality of cognitive decline by careful introduction to artwork that quickly shows degeneration through the imagery created [10, 11].
As medical research continues to improve understanding and management of the autoimmune and neuromuscular transmission specifics of MG, more opportunity is afforded to learn about the psychological aspects of the disease and how to treat it. Utilizing psychotherapeutic interventions such as psychology, creative arts therapy, counseling, in combination with other pharmacological interventions has potential to provide relief for patients and their caregivers [12]. Such psychosocial interventions are in need of greater study in the context of neuromuscular disorders including MG [13].
In summary the physician is on the front line of recognizing the patterns of myasthenic and non-myasthenic weakness and using this recognition to develop optimal treatment strategies often in collaboration with a professional in the psychological mechanisms and aspects of chronic illness. The recognition of the “dropped brow sign” as evidence for psychogenic pseudo-myasthenic ptosis allows for early exploration of a psychological component to the patients symptoms and development of optimal evaluation and therapy.
Common eye features of psychogenic myasthenia:
•Subjective non-specific fatigue and weakness
•Lack of objective signs
• Dropped brow sign
•Convergence spasm
•Giveaway
References
- Sieb JP (2014) Myasthenia gravis: An update for the clinician. Clin Exp Immunol 175: 408-418.
- Fullerton DT, Munsat TL (1966) Pseudo-myasthenia gravis: A conversion reaction. J Nerv Ment Dis 142: 78-86.
- Pascuzzi RM (2003) The edrophonium test. Semin Neurol 23: 83-88.
- Ybarra MI, Kummer A, Frota ER (2011) Psychiatric disorders in myasthenia gravis. Arq Neuropsiquiatr 69: 176-179.
- Qiu L, Feng HY, Huang X (2010) Study of incidence and correlation factors of depression, anxiety and insomnia in patients with myasthenia gravis. Zhonghua Yi Xue Za Zhi 90: 3176-3179.
- Lundeen J, Fisher J, Kothari MJ (2004) Frequency of anxiety in myasthenia gravis. J Clin Neuromuscul Dis 6: 9-12.
- Zou J, Su C, Lun X, Liu W, Yang W, et al. (2016) Preoperative anxiety in patients with myasthenia gravis and risk for myasthenic crisis after extended transsternal thymectomy: A consort study. Medicine (Baltimore) 95: e2828.
- van der Kolk BA (2014) The body keeps the score: Brain, mind, and body in the healing of trauma. New York, NY.
- American Art Therapy Association (2015) What is art therapy?
- Walsh S, Martin S, Schmidt L (2004) Testing the efficacy of a creative-arts intervention with family caregivers of patients with cancer. J Nurs Scholarsh 36: 214-219.
- Sezaki S, Bloomgarden J (2000) Home-based art therapy for older adults. Art Therapy 17: 283-290.
- Koopman WJ, LeBlanc N, Fowler S, Nicolle MW, Hulley D (2016) Hope, coping, and quality of life in adults with myasthenia gravis. Can J Neurosci Nurs 38: 56-64.
- Walklet E, Muse K, Meyrick J, Moss T (2016) Do psychosocial interventions improve quality of life and well-being in adults with neuromuscular disorders? A systematic review and narrative synthesis. J Neuromuscul Dis 30: 347-362.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences