Scleral Buckling Procedure with Chandelier Illumination
Toshiyuki Yokoyama*
Department of Ophthalmology, Juntendo University Nerima Hospital, Tokyo, Japan
- Corresponding Author:
- Toshiyuki Yokoyama
Department of Ophthalmology
Juntendo University, Nerima Hospital
3-1-10 Takanodai, Nerima-ku, Tokyo 177-8521, Japan
Tel: +81 3 5923 3111
Fax: +81 3 5923 3217
E-mail: yokoyama@juntendo-nerima.jp
Received date: June 13, 2017; Accepted date: July 20, 2017; Published date: July 27, 2017
Citation: Yokoyama T (2017) Scleral Buckling Procedure with Chandelier Illumination. Ins Ophthal. Vol. 1 No. 3:11
Abstract
Scleral buckling is still a useful and effective technique to repair rhegmatogenous retinal detachment (RRD), especially in phakic eyes, but many retinal surgeons have recently preferred to perform pars plana vitrectomy (PPV). Scleral buckling has some disadvantages compared to PPV, such as the requirement for expertise in using the indirect ophthalmoscope in a particular position and the obscured view of the indirect ophthalmoscope in eyes with opaque media or small pupil. Retinal breaks are difficult to identify and treat in eyes with opaque media, small pupil or small retinal holes. However, RRD in young patients without posterior vitreous detachment should be treated by scleral buckling. To minimize these problems, we applied advanced instruments, chandelier illumination and the wide-angle viewing system. Scleral buckling with chandelier illumination could resolve some of the problems. This technique has some advantages and possible disadvantages, but allows scleral buckling surgery with reduced risk of cataract induced by PPV in phakic RRD.
Keywords
Rhegmatogenous retinal detachment; Wide-angle viewing system; Ophthalmoscope; Fundus view
Introduction
Two main procedures are generally selected for the repair of rhegmatogenous retinal detachment (RRD), scleral buckling and pars plana vitrectomy (PPV), based on the severity of the retinal detachment, more specifically the degree of proliferative vitreoretinopathy, location of the break, lens status, presence of vitreous hemorrhage, patient’s age and surgeon’s experience or technique.
The Preferences and Trends (PAT) Survey of retina specialists found that recent advances in vitrectomy systems have encouraged the adoption of primary PPV, which allows completion of all steps of surgery under the operating microscope with excellent visibility [1]. Moreover, all staff in the operating room can observe the surgery using the recording and monitoring system of the microscope. In contrast, conventional scleral buckling requires repeated positioning of the indirect ophthalmoscope, which gives only an unshared inverted fundus view, and considerable surgical skill, especially in eyes with opaque media or small pupil. However, scleral buckling is still preferred in some cases, especially in phakic younger patients with breaks in lattice degeneration without posterior vitreous detachment [2]. Chandelier illumination together with the recently developed wide-angle viewing system (WAVS) may solve some of these problems.
Scleral Buckling with Chandelier Illumination and Non-contact WAVS
Microsurgery for retinal detachment repair was described in 1987 using microscopy with slit lamp illumination attached to the microscope to identify the retinal breaks and the 3 mirror contact lens without chandelier or other intraocular illumination [3]. The reported success rate was excellent, but the procedure is thought to be complicated and requires more time. The surgical view can be shared and magnified, but may be inverted and restricted to only a small area.
Scleral buckling surgery with chandelier illumination was reported in 2012 using a non-contact WAVS in 16 patients with RRD [4]. A 25 gauge Torpedo light (Alcon Laboratories, Inc., Fort Worth, TX, USA) was inserted through the sclerotomy with a 27 gauge needle as chandelier illumination and BIOM (Oculus Optikgeräte GmbH, Wetzlar, Germany). Retinal reattachment was achieved in 13 eyes (81.3%). During surgery, scleral perforation occurred in one eye due to excessive indentation. No complication was caused by the chandelier illumination. Since then, several reports using this system have been published [5-13].
Surgical Technique
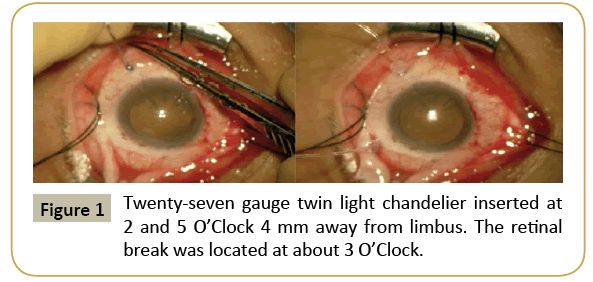
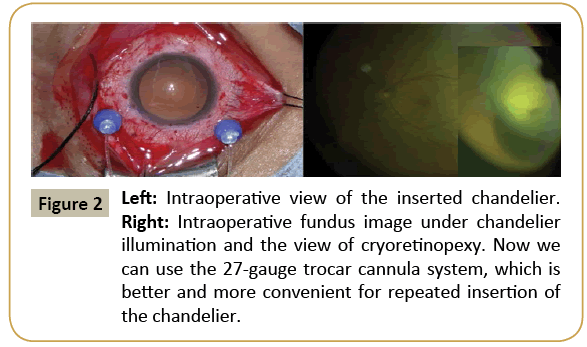
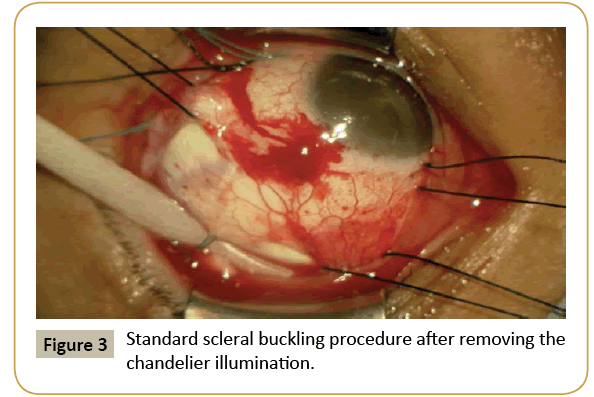
The standard procedure uses WAVS under chandelier illumination inserted into the vitreous through the sclera at about 3-4 mm from the limbus with or without microcannula (Figure 1). Retinal breaks are identified and cryoretinopexy is performed using the surgical view of the WAVS under chandelier illumination (Figure 2). The chandelier is then removed and the buckling procedure with or without subretinal fluid drainage is performed (Figure 3). The chandelier is then inserted again to observe the fundus view. A 25 gauge single port chandelier is mainly used, but we used a 27 gauge twin light chandelier [6] and a 29 gauge twin light chandelier was used in one case [13]. The chandelier is mainly placed in the quadrant next to or opposite from the retinal breaks. A retinal break under or very close to the chandelier is difficult to identify because of light glare.
An interesting modification of this procedure was used for sub retinal fluid drainage [14]. After cryopexy and scleral buckling by the conventional method, a 25 gauge chandelier was placed and the WAVS was activated. Under direct visualization, a 25 gauge needle mounted on a tuberculin syringe with plunger removed was inserted into the subretinal space in an area of retinal detachment away from the large retinal break and subretinal fluid was drained. This technique allowed more controlled sub retinal fluid removal with excellent visualization without complications. The chandelier was not used to identify and treat the retinal break because of the risk of complications caused by repeated removal and reinsertion of the chandelier.
Primary Reattachment Rate
Cases with difficult presentations such as undetected retinal breaks were all reattached. Reported initial reattachment rates are mostly over 90%, ranging from 81.3% to 94.27% [4,8,9,11- 13]. In our 49 patients, initial reattachment was achieved in 47 of 49 eyes (95.9%) (Unpublished data). Comparisons to the conventional method have shown that the primary success rate was almost equal [8,9,11].
Advantages of the Present Technique
This technique has some advantages compared with the conventional method. The most important feature allows direct observation under the surgical microscope so that the fundus view can be magnified and monitored. Therefore, even small breaks, which can be hard to find by the conventional method, can be detected. Several authors including us have reported retinal breaks identified intraoperatively which were not found by careful preoperative examination [5,6,10]. The risk of intraoperative corneal epithelial disorder is also reduced because the good surgical view decreases the need to peel the corneal epithelium even in the presence of corneal opacity caused by the WAVS [7]. The shared surgical view is very useful for instruction and education of staff, especially inexperienced fellows or residents [9].
Use of the WAVS together with chandelier illumination allows wide-angle fundus view of the surgical area even if the eye has a small pupil or mild opaque media. In addition, the surgeon does not have to wear an indirect ophthalmoscope or adopt a specific position. This advantage reduces the chance of infection and may shorten surgical time. Surgical duration is reportedly shorter compared with the conventional method [8,9,11]. However, our unpublished data suggest that the surgical duration was longer compared with the conventional method, possibly due to selection bias, because many of our patients had undetected or hardly visible breaks. The risk of neck or back injury due to the position required may be reduced compared to the conventional method because the present technique enables surgeons to maintain a comfortable posture [8].
Disadvantages and Possible Complications of the Present Technique
Only one severe complication has so far been reported, scleral perforation in one eye due to excessive indentation during cryopexy [4], which was not related to either chandelier illumination or the WAVS. Only a few complications related to the chandelier system were reported. However, the main feature of this technique, insertion of the chandelier illumination, may cause some complications including intraocular injury such as lens touching, retina or ciliary injury, and vitreous hemorrhage. Such complications occurred in 7 of 79 eyes in 79 patients and included limited choroidal hemorrhage in 5 eyes, retinal break in one eye thought to be related to the cannula-based chandelier illumination, and lens touching during cryoretinopexy in one eye, which fortunately did not induce cataract progression [12]. Light toxicity is another possible complication, but is unlikely because phototoxicity occurs only after close exposure of the retina to high intensity light for a long period [15].
Insertion of the chandelier illumination requires sclerotomy. After removal of the chandelier illumination, vitreous leakage or wicking may occur which could induce retinal traction or postoperative intraocular infection. Vitreous leakage likely occurs after large sclerotomy and without use of the trocar cannula system. Angle incision performed with a trocar cannula could reduce the risk of vitreous leakage [7]. Scleral suture to correct vitreous leakage was not required in any of the 12 patients treated using a 25 gauge chandelier inserted as above. We use the 27 gauge twin light chandelier inserted through angle incision with or without use of the trocar cannula system, but vitreous leakage occurs especially under high intraocular pressure after scleral buckling suture. Sometimes we need to treat vitreous wicking and we think that complete covering of the sclerotomy by the conjunctiva is important to prevent postoperative intraocular infection.
The chandelier system hinders rotation of the eye ball and scleral buckling. Contamination may result from touching the microscope or chandelier illumination bend and then touching the lens or retina. Therefore, the chandelier illumination should be removed during the buckling procedure.
Another disadvantage of this technique is the requirements for expensive specialized equipment such as chandelier illumination, chandelier light source and the WAVS or contact lens. Most previous reports used the WAVS and we also prefer the WAVS to contact lens because of the excellent wide angle fundus view.
Future Prospects
Recently, many surgeons have preferred vitrectomy for the repair of retinal detachment, possibly due to the recent introduction of advanced micro incision vitrectomy surgery with sophisticated instrumentation and the WAVS. In contrast, the scleral buckling procedure needs some experience and skill, especially to examine the fundus using the indirect ophthalmoscope and requires the surgeon to wear the indirect ophthalmoscope in a particular position. Conventional scleral buckling is also difficult to study for fellows or residents because the fundus view cannot be shared, so only the surgeon can identify and treat retinal breaks. Some of these disadvantages can be resolved by using chandelier illumination together with the WAVS. This technique may be suitable for the inexperienced retinal surgeon under instruction from a skilled surgeon. The WAVS and chandelier system have been introduced widely with the prevalence of advanced vitrectomy surgery. Many surgeons have developed experience with this procedure, and advances in the systems are likely. Brighter light sources and smaller chandelier illumination will make this technique easier and safer.
Scleral buckling with the chandelier illumination technique may encourage the use of scleral buckling surgery and may reduce the risk of cataract progression due to vitrectomy in phakic patients.
References
- Williams PD, Hariprasad SM (2014) Evolving trends in primary retinal detachment repair: microincisional votrectomy and the role of OCT. Ophthalmic Surg Lasers Imaging Reina 45: 268-272.
- Heimann H, Bartz-Schmidt KU, Bornfeld N, Weiss C, Hilgers RD, et al. (2007) Scleral buckling versus primary vitrectomy in rhegmatogenous retinal detachment. A prospective randomized clinical study. Ophthalmology 114: 2142-2154.
- Bonnet M (1987) Microsurgery for retinal detachment repair. Dev Ophthalmol 14: 5-10.
- Aras C, Ucar D, Koytak A, Yetik H (2012) Scleral buckling with a non-contact wide-angle viewing system. Ophthalmologica 227: 107-110.
- Kita M, Fujii Y, Kawagoe N, Hama S (2013) Scleral buckling with a noncontact wide-angle viewing system in the management of retinal detachment with undetected retinal break: A case report. Clin Ophthalmol 7: 587-589.
- Yokoyama T, Kanbayashi K, Yamaguchi T (2015) Scleral buckling procedure with chandelier illumination for pediatric rhegmatogenous retinal detachment. Clin Ophthalmol 9: 169-173.
- Nam KY, Kim WJ, Jo YJ, Kim JY (2013) Scleral buckling technique using 25 gauge chandelier endoilluminator. Retina 33: 880-882.
- Tomita Y, Kurihara T, Uchida A, Nagai N, Shinoda H, et al. (2015) Wide-angle viewing system versus conventional indirect ophthalmoscopy for scleral buckling. Sci Rep 5: 13256.
- Narayanan R, Tyagi M, Hussein A, Chhblani J, Apte RS (2016) Scleral buckling with wide-angled endoillumination as a surgical educational tool. Retina 36: 830-833.
- Temkar S, Takkar B, Azad SV, Vankatesh P (2016) Endoillumination (chandelier) assisted scleral buckling for a complex case of retinal detachment. Indian J Ophthalmol 64: 845-846.
- Li XJ, Yang XP, Lyu XB (2016) Comparison of scleral buckling using wide-angle viewing systems and indirect ophthalmoscope for rhegmatogenous retinal detachment. Int J Ophthalmol 9: 1310-1314.
- Imai H, Tagami M, Azumi A (2015) Scleral buckling for primary rhegmatogenous retinal detachment using noncontact wide-angle viewing system with a cannula-based 25 G chandelier endoilluminator. Clin Ophthalmol 9: 2103-2107.
- Seider MI, Nomides RE, Hahn P, Mruthyunjava P, Mahmoud TH (2016) Scleral buckling with chandelier illumination. J Ophthalmic Vis Res 11: 304-309.
- Haug SJ, Jumper JM, Johnson RN, McDonald HR, Fu AD (2016) Chandelier-assisted external sub retinal fluid drainage in primary scleral buckling for treatment of rhegmatogenous retinal detachment. Retina 36: 203-205.
- Vander JF, Eagle RC Jr, Brown GC, Arbizo V, Shakin EP, et al. (1991) Retinal tolerance of an implantable light source for use during vitrectomy surgery. Ophthalmic Surg 22: 735-739.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences