Implementation of Observational Learning via Adjunctive Videos to Improve Physical Assessment Self-Efficacy and Skill
Hyma Gogineni1*, Marie Davies1, Divvjyot Singh1, Marvin Ortiz1, Linda S Garavalia1 and Haarika P Gogineni2
1Department of Pharmacy, Western University of Health Sciences, College of Pharmacy, California, USA
2Department of Pharmacy, University of Irvine, California, USA
- *Corresponding Author:
- Hyma Gogineni
Department of Pharmacy, Assistant Professor of Pharmacy Practice and Administration
Western University of Health Sciences, College of Pharmacy, California, USA
Tel: +909-469-5457
E-mail: hgogineni@westernu.edu
Received date: December 14, 2017; Accepted date: January 01, 2018; Published date: January 04, 2018
Citation: Gogineni H, Davies M, Singh D, Ortiz M, Garavalia LS, et al. (2018) Implementation of Observational Learning via Adjunctive Videos to Improve Physical Assessment Self-Efficacy and Skill. J Pharma Pract Edu Vol 1:8
Copyright: © 2018 Gogineni H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: Physical assessment (PA) skills are crucial for pharmacists to provide comprehensive medication therapy management services. The purpose of this study was to investigate the effectiveness of an observational learning strategy to enhance student pharmacists’ self-efficacy and skills.
Methods: To promote retention of PA skills, seven PA videos were created as adjuncts to didactic instruction. After comprehensive PA practicum and written examinations, students completed a survey assessing utilization of the PA videos and self-efficacy for performing PA skills.
Results: All 112 students completed the survey, and 94.6% watched at least one video. Over 90% of students indicated being confident in performing vitals, ophthalmic exam, and musculoskeletal exams. The majority of students indicated that the videos helped prepare for the practicum, whereas only 54.7% felt the videos prepared them for the written examination.
Conclusions: Observational learning can be an effective instructional strategy for the development of performancebased skills in pharmacy curricula.
Keywords
Curriculum design; Patient assessment; Physical assessment; Physical examination; Self-efficacy; Videos
Introduction
Approximately 125 million Americans (45% of the US population) have one or more chronic conditions, and 61 million (21% of the US population) have multiple chronic conditions. Pharmacists are qualified in the medication management of chronic diseases and are well-positioned to provide this type of care. For 90% of patients with chronic disease, medications are a first-line of treatment. Pharmacists’ involvement in the team-based management of patients with chronic medical conditions has repeatedly been shown to improve patient outcomes and reduce overall healthcare costs [1]. Pharmacists are uniquely situated in community and primary-care settings to meet the needs of patients to improve access and continuity of care through expanded responsibilities in providing collaborative drug therapy management [2]. Part of the expanded roles of pharmacists include patient assessment skills such as performing and interpreting physical assessments (PAs), as well as health screening and interpreting laboratory data. PAs that pharmacists typically perform are currently limited to basic vital signs, mostly blood pressure measurement alone [3]. Pharmacist provided comprehensive PA could improve disease management and drug optimization for patients.Effective January 1, 2014, California pharmacists were recognized as healthcare providers under SB 493, giving pharmacists broader authority to provide health care services in that state. For example, SB 493 adds a license classification for advanced practice pharmacists (APP) who may perform patient assessments [4]. As pharmacists’ scope of practice continues to expand and transition from pharmacotherapy advisors to medication therapy managers, all pharmacists should have training in physical assessment. As a result, pharmacy professional program curricula now include PA skills, but studies are scarce regarding the effectiveness of that training [5-10].
The importance of PA in pharmacy education was recognized in 1993 by the Commission to Implement Change in Pharmaceutical Education. The commission reported that, in order to provide pharmaceutical care, pharmacists must be able to monitor patients’ progress with regard to therapeutic objectives and to detect and prevent adverse drug consequences [10,11]. The Accreditation Council for Pharmacy Education (ACPE) Standards 2016 now includes patient assessment as a required component of the PharmD curriculum. The evaluation of patient function and dysfunction through the performance of tests and assessments leading to objective (e.g., physical assessment, health screening, and lab data interpretation) and subjective (patient interview) data is important to the provision of care [11]. Standard 2: Essentials for Practice and Care indicates that patient care should incorporate performing physical assessments [12]. Similarly, the Joint Commission of Pharmacy Practitioners (JCPP) newly defined Pharmacists’ Patient Care Process (PPCP) indicates that, as part of “collect”, pharmacists should gather and verify patient information from multiple sources, including the physical examination [13]. Therefore, pharmacist training in PA skills to enhance patient-centered care has to be increased in pharmacy education.
In 2007, Spray and Parnapy surveyed multiple US pharmacy programs on the content, extent, and design of PA training in pharmacy curricula. In this study, variability was found in coverage of PA topics, depth of the coverage, types of instruction, and evaluation methods used for PA for each program. Of the 72 programs responding, 96% reported teaching PA skills to some degree. The most commonly taught skills in the PA courses were pulmonary examination, cardiovascular examination, and vital signs. Other PAs such as head, eyes, ears, nose, and throat (HEENT), musculoskeletal, abdomen/gastrointestinal, neuromuscular, and skin, hairs, and nails were taught less frequently ranging from <50% to ~80% of programs teaching these assessments. It is unknown if programs that did not respond to the survey (26% of pharmacy schools) teach PA. Additionally, as noted, many of the PA skills (e.g., HEENT, skin, hair, and nails) were infrequently emphasized [5]. The study did not report instructional design models utilized in teaching PA.
Utilization of evidence-based instructional design models that focus on the development of performance-based skills may be important when teaching PA, which has not been well described in the literature within pharmacy curriculum. Observational learning may be a good instructional design platform for emphasizing retention of the skills requiring demonstration. Bandura’s theory of social learning proposed that “most human behavior is learned by observation through modeling” [14]. Numerous studies support the learning model. For example, a study with medical students compared paired versus individual learning and found that students who were paired with a partner learned PA skills to a greater extent than those who practiced alone [15]. The researchers attributed the difference to the effects of observing a peer in the acquisition of PA skills
Prior to fall 2014, the Western University of Health Sciences (WesternU) College of Pharmacy PA curriculum was limited to measuring blood pressure, pulse, performing diabetic foot examinations, and listening to different lung sounds on a simulated manikin. This limited breadth of coverage was similar to other colleges of pharmacy in the US [5]. To align with the new ACPE standards and guidelines from professional associations, WesternU expanded the curriculum to include PA skills beyond blood pressure, pulse, and blood glucose checks etc. The comprehensive Head-to-Toe PA instruction was implemented in the 2014-2015 academic year. Student feedback indicated a need for additional modeling of the skills. Thus, a series of PA videos were developed by the first class of students and subsequently shared with upcoming classes. The videos with peer models implement an observational learning model that is well-documented as an effective instructional strategy [14,16]. The purpose of this study was to assess student pharmacists’ self-efficacy for physical assessment and to evaluate performance in physical assessment skills with the use of videos to augment didactic instruction.
Methods
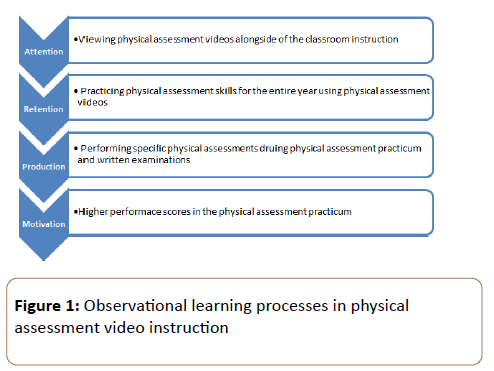
Observational learning involves four processes (see Figure 1). The development of the physical assessment curriculum is described below and the alignment of instructional activities with the observational learning model is outlined in (Figure 1)
Physical assessment curriculum design
Physical assessment was added to the didactic curriculum in the 2014-15 academic year as a year-long curriculum. Due to large class size, the students were divided into two groups (approximately 60 students/group), and each group received PA instruction in four 2-h sessions during fall and spring semesters. Topics taught in the fall were (1) vitals, (2) HEENT examination, (3) pulmonary examination, and (4) abdominal examination, and in the Spring were (1) cardiovascular examination, (2) musculoskeletal examination, (3) neuromuscular examination, and (4) dermatologic examination.
Cardinal techniques such as inspection, palpation, percussion, and auscultation were integrated throughout the PA instruction. Each topic session began with 5-10 min of didactic teaching followed by modeling of the physical assessment by a faculty member. Students participated as mock patients. The faculty member explained the examination findings (normal vs. abnormal). Students then had an opportunity to practice the skill on peers for an additional 15-30 min before moving on to the next skill. The faculty member monitored and provided guidance as necessary during this practice period.
Following completion of the curriculum, students indicated in the course evaluation that these new skills were difficult to transfer to real-life scenarios and that, often times, they forgot how to perform the skills. To improve retention, two pharmacy practice faculty and eight student pharmacists developed seven physical assessment videos (vitals, HEENT, pulmonary, abdominal, cardiovascular, musculoskeletal, and neuromuscular examinations) to augment didactic instruction. The videos emphasized practical PA skills that were likely to be tested in the practicums/objective structured clinical examination (OSCE), utilized in introductory pharmacy practice experiences, and performed in practice after graduation. Total production time for each 3-9 min video was approximately 10 h. Faculty provided guidance throughout production. All videos were recorded using an Apple iPhone camera and edited using iMovie 10.1 program. All videos were made available on Blackboard for the next class of P1s during the following academic year. At the end of each didactic PA session, students were encouraged to watch the videos to reinforce their skills.
Evaluation of students’ physical assessments skills
Students’ PA skills were evaluated at the end of each semester through a cumulative practicum exam. For the timed exam, students were given five minutes to perform three skills (e.g., auscultate lungs anteriorly, percuss the liver span, and palpate point of maximal impulse) on an assigned partner, who played the role of the patient. Partners switched roles, and three separate skills were evaluated. Pharmacy faculty members and residents used an objective structured rubric that included critical steps in each physical assessment to evaluate technique, communication and professionalism. Training on the PA skill and use of the scoring rubric was provided for all graders for each PA skill that he/she would be grading. Graders assigned credit or no credit to each item on the scoring rubric. A minimum score of 70% on the PA practicum exam was required for progression in the program. Students were also required to pass a cumulative PA written exam at the end of the spring semester comprised of 25 multiple choice questions designed to evaluate the ability of the student pharmacists to interpret physical exam findings.
Current research study
This quality-improvement educational study was approved by the WesternU institutional review board. Participants included all WesternU first year student pharmacists in the 2015-16 academic year enrolled in the spring Foundations of Pharmacy Practice/Self-Care Therapeutics II course. In addition to the course written and practicum exams, students voluntarily consented to complete a survey of their use of the videos and confidence in their PA skills. Informed consent was obtained and the survey administered after students completed the written and practicum exams to eliminate the threat of potential grading bias. Survey items asked which physical assessment videos were viewed, number of times each video was viewed, and the helpfulness of the videos for the written and practicum exams. The survey also assessed students' self-efficacy in performing each skill using a 4-point Likert scale (1=strongly disagree, 2=disagree, 3=agree, 4=strongly agree). Each student was assigned a random identification number which linked their survey responses to their performance on both written and practicum exams.
Study objectives were to assess students’ perceptions of the helpfulness of the PA skills videos, evaluate the association between video viewing and performance on examinations, identify predictors for higher performance on the written and practicum examinations, and examine the relationship between self-efficacy and performance. Survey responses and grades were analyzed with descriptive statistics. Predictors were dichotomized as strongly disagree/disagree and strongly agree/ agree vs. above average and below average on the written and practicum examination. Nominal data were analyzed on univariate analysis using a Chi Squared test.
Results
There were 112 students in the class and all completed the PA survey. The class average percent correct on the written examination was 88.3 (5.7) and 81 (10.8) on the practicum. Of the 112 students, 106 students (94.6%) watched at least one video, and, on average, students watched the videos 1.7 (0.7) times. The most commonly viewed video (92.5% of students) was the abdominal exam followed by musculoskeletal (91.5% students) exam (see Table 1).
| Videos | n, (%) |
| Vitals | 80 (75.5) |
| HEENT | 88 (83.0) |
| Neuromuscular | 92 (86.8) |
| Pulmonary | 95 (89.6) |
| Cardiovascular | 96 (90.6) |
| Musculoskeletal | 97 (91.5) |
| Abdominal | 98 (92.5) |
Table 1: Percent of students watching each video at least once
Eighty-four students (79%) felt that they would have not achieved the same result on the written and practicum exams without the physical assessment videos. On the written exam, students performed the lowest on questions regarding the cardiovascular examination-for example, understanding jugular venous distention (JVP), location of the cardiac values, and heart sounds. On the practicum exam, range of motion on the musculoskeletal examination, identification of dermatologic abnormalities, and costovertebral tenderness were also areas of weakness. The most commonly observed errors in the practicum exam are presented in Table 2.
| When performing a lung exam, auscultating above and below the diaphragm (moving into the abdominal area) |
| Forgetting to perform the examination bilaterally |
| Experiencing difficulty differentiating between muscle strength (a neuromuscular parameter) vs. passive range of motion (a musculoskeletal parameter) |
| Being fearful of hurting the patient, not inserting the otoscope in the patients’ ears completely (or failing to properly position the ear canal) |
Table 2: Most commonly observed errors in student’ physical assessment procedures
Students reported high levels of confidence in their PA skills at the end of the semester see (Table 3)
| I felt confident in performing….. | Median | Mean | # of students who SA/A (%) |
|---|---|---|---|
| Inspection | 3 | 3.1 | 90 (84.9) |
| Palpation | 3 | 3 | 85 (80.2) |
| Percussion | 3 | 3 | 81 (76.4) |
| Auscultation | 3 | 3.2 | 94 (88.7) |
| Vitals | 3 | 3.4 | 102 (96.2) |
| Eyes | 3 | 3.2 | 98 (92.5) |
| ENT | 3 | 2.9 | 85 (80.2) |
| Neuromuscular | 3 | 3 | 90 (84.5) |
| Pulmonary | 3 | 3.1 | 91 (84.5) |
| Cardiovascular | 3 | 2.9 | 81 (76.4) |
| Musculoskeletal | 3 | 3.1 | 97 (91.5) |
| Abdominal | 3 | 2.9 | 88 (83) |
| *SA/A=strongly agree/ agree 4-point Likert scale (1=strongly disagree, 2=disagree, 3=agree, 4=strongly agree) | |||
Table 3: Survey perceptions of confidence in physical assessment skills/technique at the end of the course
Over 90% of students agreed or strongly agreed that they were confident performing vitals, an eye exam, and a musculoskeletal exam. Lower confidence, where less than 80% agreed to be confident, was reported for the cardiovascular exam and the cardinal technique of percussion.
The median for each physical exam and cardinal technique was a 3 (Agree) (see Table 2) of the 106 students who viewed the videos, 101 (95.3%) agreed or strongly agreed that the videos helped them prepare for the practicum, whereas only 58 (54.7%) agreed or strongly agreed that the videos helped them prepare for the written examination. Predictors for scoring above average on the written examination included using physical assessment at work or on introductory pharmacy practice experiences (IPPE) and watching the videos at least twice. Associations were statistically significant on Chi Squared test for association (P=0.03 and P=0.005, respectively). No other predictors were statistically significant for the written exam performance. In addition, no significant predictors were found for the practicum examination performance. These predictors are listed in Table 4.
| Criterion | % scoring above average on WE | % scoring above average on PE | ||
|---|---|---|---|---|
| Used PA at work/on IPPE | 51 | 57 | ||
| Not using PA at work/on IPPE | 30 | P=0.03 | 63 | P=0.56 |
| Watched videos once | 43 | 67 | ||
| Watched PA video ≥ 2 times | 63 | P=0.01 | 55 | P=0.23 |
| SA/A that PA videos helped with pulmonary exam | 38 | 60 | ||
| SD/D that PA videos helped with pulmonary exam | 50 | P=0.41 | 63 | P=1.0 |
| SA/A that PA videos helped with neuromuscular exam | 37 | 62 | ||
| SD/D that PA videos helped with neuromuscular exam | 56 | P=0.17 | 50 | P=0.41 |
| SA/A that PA videos helped with cardiovascular exam | 38 | 62 | ||
| SD/D that PA videos helped with cardiovascular exam | 44 | P=0.65 | 56 | P=0.64 |
| SA/A that PA videos helped with musculoskeletal exam | 39 | 60 | ||
| SD/D that PA videos helped with musculoskeletal exam | 37 | P=1.0 | 62 | P=1.0 |
| SA/A that PA videos helped with ENT exam | 41 | 60 | ||
| SD/D that PA videos helped with ENT exam | 33 | P=0.62 | 62 | P=1.0 |
| SA/A that PA videos helped with auscultation | 36 | 62 | ||
| SD/D that PA videos helped with auscultation | 67 | P=0.06 | 50 | P=0.53 |
| SA/A that PA videos helped with inspection | 90 | 62 | ||
| SD/D that PA videos helped with inspection | 15 | P=0.09 | 46 | P=0.27 |
| SA/A that PA videos helped with percussion | 41 | 59 | ||
| SD/D that PA videos helped with percussion | 36 | P=0.82 | 64 | P=0.81 |
| SA/A that PA videos helped with palpation | 38 | 62 | ||
| SD/D that PA videos helped with palpation | 48 | P=0.46 | 52 | P=0.45 |
| *SA/A=Strongly Agree/Agree; SD/D=Strongly Disagree/Disagree; PA=Physical Assessment; ENT=Ears/Nose/Throat; WE=Written Exam; PE=Practicum Exam IPPE=Introductory Pharmacy Practice Experiences | ||||
Table 4: Predictors of scoring above average on the written or practicum exam
Discussions
In this study, we found high mean performance on both the written and practicum examinations for PA after incorporating videos into the courses. Ideally, we would have measured the impact of the videos by comparing this cohort of students to the previous cohort, but the practicum and written exams were different for the previous year class. Another option would have been to compare video watchers to non-watchers, but too few students were non-watchers. Interestingly, we did find that students who watched the videos more than twice had higher scores on the written examination. Counterintuitively, these results were only statistically significant for the written exam and not the practicum. A study in the medical professions reported use of videos in teaching ophthalmic physical examination to chiropractic students. In contrast to our findings, compared to students who did not watch the videos, students who watched videos of the standard physical examination and of common mistakes had higher laboratory scores (P<0.001) but scores on a written exam were not significantly different [15]. Another learning component of our study was the engagement of students from the prior year in developing and producing the videos. Anecdotally, the teaching opportunity strengthened the PA skills of those students. ACPE Standard 3.2 indicates that student learners should “educate all audiences by determining the most effective and enduring ways to impart information and assess learning”. The students who made these videos not only helped the incoming class, but the process of mastering the material reinforced their own PA skills. These students also demonstrated innovation creating this method to enhance the curriculum [11-16]. In terms of common PA errors identified by faculty, the musculoskeletal examination challenged students the most.
This finding is concerning because musculoskeletal injuries are a common reason patients seek pharmacists’ advice in community and ambulatory care settings. Other studies indicate professional students struggle with this PA. For example, Peitzman and Cuddy compared medical student physical examination performance on standardized patients in the United States Medical Licensing Examination (USMLE) Step 2 with history taking and found that, on average, physical examination scores were lower (59.6%) than history taking. Neuromuscular and musculoskeletal mean scores were lower than cardiovascular, respiratory, and gastrointestinal [17]. This particular PA may require even more instructional intervention than other assessments. In the present study, lower performance on the practicum exam was associated with confusion between passive range of motion and muscle strength. To remedy this, we have added a muscle strength examination to the musculoskeletal section, even though it is a neuromuscular examination, so that students might more easily distinguish between the two. Interestingly, 91% of students reported high confidence for the musculoskeletal examination, the third highest confidence rating (following vitals and the eye examination). Students’ self-awareness of PA skills may be an area for future research to explore differences in students’ beliefs about their skills and actual skills. Students also performed lower on the written exam on advanced cardiovascular physical assessments-assessing for JVD and valve location. One potential explanation is that cardiology anatomy and physiology is more complex and challenging because students cannot correlate physical findings as well without the clinical background of specific disease states. In our program, therapeutics is not taught until the P2 year (i.e., applications of heart failure and JVD assessment are not in the first year curriculum).
Students perceived the PA videos to be helpful in developing PA skills. In addition, over 80% of the students agreed or strongly agreed that they were confident in most examinations and cardinal techniques, with cardiovascular and cardinal technique of percussion being the only 2 survey items rated slightly below 80%. Since the majority of the students were confident in skills (i.e., lack of variability in responses), most univariate predictors associated with confidence after watching the videos did not significantly predict written or practicum scores. The majority of students felt well prepared; however, students may have been overconfident in some PA skills. This confidence may be due to a greater willingness of student pharmacists to practice these skills on rotations. Hopefully, this would lead to greater comfort in offering comprehensive medication therapy management services when in practice.
In our study, students who utilized physical assessment at work or on IPPE had significantly higher written examination scores. Students who had the opportunity to apply skill-based curricula to real-life settings may be able to more easily transfer classroom learning to practice. We should encourage students to practice utilizing skills on friends/family and in their community and ambulatory care practice sites (work or IPPE/APPE). Future research should explore how these additional opportunities impact skill retention.
An issue we observed in using skills on rotations was that many pharmacy preceptors were not comfortable with this practice and, therefore, would not allow students to perform such skills. Pharmacy education needs to continue to emphasize the practice of physical assessment in therapeutic courses as a means for triage in the community and ambulatory care settings so that students value and feel confident in using these skills. Collection and assessment of subjective and objective information as part of the PPCP includes physical assessment and, therefore, continued reinforcement, training, repetition, and advocacy of pharmacists performing these skills is necessary. Several limitations should be noted for the study. First, we expected the videos to enhance performance on the practicum exam, but no baseline measures were available for comparison. We did, however, find some significant predictors for performance on the written exam. A second limitation was the lack of variability in grades for the practicum examinations.
Third, although training was provided on use of the scoring rubrics, variability in faculty subjectivity could have impacted scoring. Furthermore, students were assigned only three different practicum physical exams, and they may have been less/more confident in those particular skills. Also, half the class was assigned three different skills and those may have been perceived as more difficult. Lastly, this study includes only one class at a single institution.
Future directions for continuous quality improvement of the skills training include incorporating physical assessments into therapeutic courses and reassessing performance and self-efficacy of these skills prior to graduation. We also plan to quantify utilization of the videos throughout course work (P2-P4 years). This will allow us to determine if the videos are serving as a tool for students in later years and if more reinforcement of skills is desired. In addition, students suggested that we create videos demonstrating incorrect performance of the techniques (i.e., common errors) followed by correct demonstrations. Also, our findings indicate that adding more physical assessment to IPPEs and APPEs may be beneficial for retention. We may also require students to watch the videos prior to didactic instruction to increase utilization of the videos, which predicted higher performance on the written exam in this study.
Summary
Physical assessment skills are essential for pharmacists to provide comprehensive medication therapy management services to optimize patient-centered care. Even though accrediting bodies emphasize the importance of training student pharmacists in physical assessment skills for advanced pharmacy practice, the best method for teaching these skills has not been established. To our knowledge, this is the first pharmacy education study utilizing physical assessment videos to train students. Students perceived these videos as beneficial and to have assisted them in preparing for the practicum, more so than for the written examination. Students who watched the videos two or more times and those applying these skills at IPPE/work had higher written examination performance.
References
- Accreditation Council for Pharmaceutical Education (2016) Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Standards 2016.
- American Society of Health-System Pharmacists (1999) ASHP statement on the pharmacist’s role in primary care. Am J Health-Syst Pharm 56: 1665-1667.
- Manolakis PG, Skeleton JB (2010) Pharmacists’ contributions to primary care in the United States collaborating to address unmet patient care needs: The emerging role for pharmacists to address the shortage of primary care providers. Am J Pharm Educ 74: 7.
- Pharmacy Practice Act (2013) Cal SB 493.
- Spray JW, Parnapy SA (2007) Teaching patient assessment skills to doctor of pharmacy students: The TOPAS study. Am J Pharm Educ 71: 64.
- Bolesta S, Trombetta DP, Longyhore DS (2011) Pharmacist instruction of physical assessment for pharmacy students. Am J Pharm Educ 75: 29.
- Sherman JJ, Riche DM, Stover KR (2011) Physical assessment experience in a problem-based learning course. Am J Pharm Educ 75: 156.
- Grice GR, Wenger P, Brooks N, Berry TM (2013). Comparison of patient simulation methods used in a physical assessment course. Am J Pharm Educ 77: 77.
- Commission to Implement Change in Pharmaceutical Education (1993) Background paper II: Entry-level curricular outcomes, curricular content and educational process. Am J Pharm Educ 57: 377-385.
- Accreditation Council for Pharmaceutical Education (2016) Accreditation standards and key elements for the professional program in pharmacy leading to the doctor of pharmacy degree. Standards 2016.
- American Association of College of Pharmacy (2013) Center for the Advancement of Pharmacy Education (CAPE) 2013 educational outcomes.
- Joint Commission of Pharmacy Practitioners (2014) Pharmacists’ patient care process.
- Bandura A (1986) Social foundations of thought & action: A social cognitive theory. Englewood Cliffs, NJ: Prentice-Hall, Inc.
- Zhang N, Chawla S (2012) Effect of implementing instructional videos in a physical examination course: An alternative paradigm for chiropractic physical examination teaching. J Chiropr Educ 26: 40-46.
- Martineau B, Mamede S, St-Onge C, Rikers R, Schmidt HG (2013) To observe or not to observe peers when learning physical examination skills; that is the question. BMC Med Educ 13: 55.
- Albano CB, Brown W (2012) Integration of physical assessment within a pathophysiology course for pharmacy. Am J Pharm Educ 76: 14.
- Peitzman SJ, Cuddy MM (2015) Performance in physical examination on the USMLE Step 2 Clinical Skills examination. Academic Medicine 90: 209-213.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences