Guided Surgery-Predictable and Safer Implantology of the Future
Surina U M.Sc., DMD*
Department of Oral Surgery and Implantology, Poliklinika Smile, Croatia
- *Corresponding Author:
- Uros Surina M.Sc., DMD
Department of Oral Surgery and Implantology
Poliklinika Smile, Croatia
Tel: +385917828683
E-mail: stom65@gmail.com
Received Date: September 12, 2018; Accepted Date: October 22, 2018; Published Date: October 29, 2018
Citation: Surina U (2018) Guided Surgery-Predictable and Safer Implantology of the Future. J Clin Med Ther.3:15.
Abstract
Today more and more patient are unhappy with their dental status, constant pain or inadequate/old prosthetic solution and as result of that they are seeking for better treatment options. Also because of growing implant market nowadays every patient wants and deserves fixed or semi-fixed prosthetic solutions. Alongside with implants also implementation of CAD-CAM technology in nearly every aspect of dentistry had happened. Named technology and possibility of computer assisted planning is giving the dentist/oral surgeon wide treatment possibility, safe and precise performance with predictable results.
Keywords
Implant; Dentistry; Implantology; Guided surgery; CAD-CAM
Clinical Case
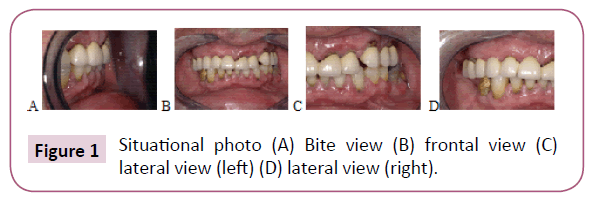
A male patient age 60 comes to the office to resolve the issue of upper and lower jaw pain due to the inadequate and decrepit prosthetic solutions as well as the visible lack of esthetics. Clinical evaluation shows that, apart from the decrepit prosthetics, there is also an old two-part dental bridge in the upper jaw between 16 and 22 and between 23 and 25. The bridges are mobile and create discomfort to the patient. In the lower jaw there is a visible crown on 44 and exceptional mobility in 36. Other teeth are also mobile except for 33, 34 and 43. Patient's oral hygiene is adequate (Figure 1).
However, it is agreed that the therapy is going to include the improvement of methods and ways of maintaining it.
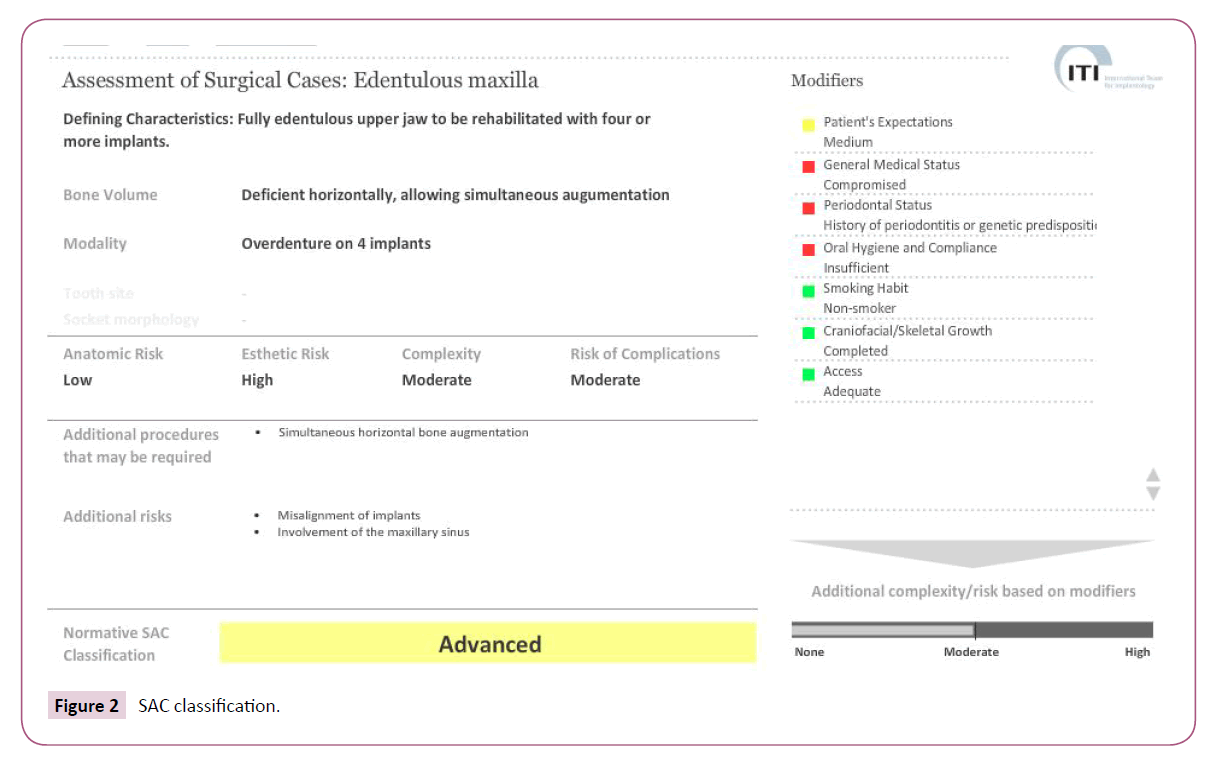
It is revealed in the conversation that the patient's expectations concerning esthetics are medium-level. He expects new, goodlooking teeth, to finally be able to smile without hiding his mouth and to chew food. Unfortunately, the patient has financial limitations and requests the work to be done within his budget. Based on the conversation with the patient, the treatment complexity evaluation is made using SAC classification [1] and the expected outcome is presented to him (Figure 2).
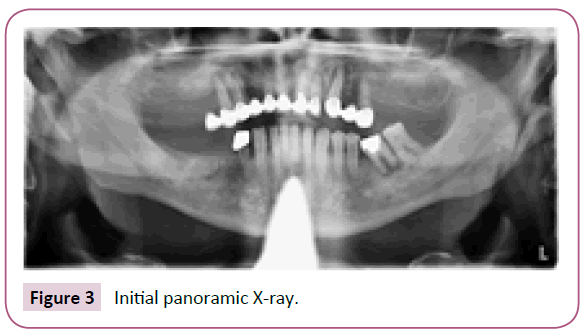
Next the panoramic dental X-ray is made and the patient completes the anamnestic questionnaire.
The panoramic X-ray reveals bone loss around the following teeth: 15, 14, 12, 21, 22, 23, 25 and 36, as well as bone retraction (periodontitis) (Figure 3).
Following inspection of oral cavity; periodontal pockets and cavities under the existing bridges in upper jaw are also evident.
In the lower jaw teeth 44, 42, 41, 31, 32, 35, 36 and 37 have also noticable movement and create discomfort for the patient when chewing.
Patient history reveals high blood pressure, heart disease (heart murmur) and previous heart surgery with the risk for endocarditis. Because he takes blood thinners every procedure on our part is done in consultation with the patient's physician and cardiologist.
In agreement with the patient and in accordance with his requests and wishes therapy is recommended and solutions are suggested that will meet both the patient's expectations and the professional criteria. Subsequently, the patient decides on a semifixed implant denture (the bar). Potential risks and complications during and after the procedure are explained to the patient and, taking into consideration his mild fear, medical history and wishes, it is decided that the procedure is going to be performed using computer assisted technology (CAD-CAM)-Guided surgery.
The first step in the therapy is elimination of inflammation processes and extraction of all teeth in upper and lower jaw. The removal procedure is only done after the confirmation of the patient's physician that he is able to have his teeth extracted and that he had stopped taking blood thinners. Extraction wounds are treated, excochleated and disinfected with povidone-iodine. The same day temporary prosthetics are made from cold, self - curing , dental base acrylic resin [2]; occluded/aligned and a new jaw alignment is created because previous procedures had left the patient's jaw bite misaligned and uneven on both sides. The patient is scheduled a follow-up appointment in a few days and a potential prosthetics alignment within 2 to 3 weeks.
After 3 months the patient returns and the next step in the therapy is agreed-operation and implant provision. The procedure is done using guided surgery and local anesthesia (articain hydrochloride/ adrenaline (tartarate) [3]. After the procedure is explained to him, the patient signs the required consent forms and diagnostic procedure begins, including impressions and X-rays of both jaws.
First, the prosthetics are lined to improve adherence to the gums. Next, a complete CT is done to inspect the condition of the solid structures-bones, to verify post extraction wound healing and bone to epithelia ratio (gingiva thickness). It is visible that the bone has not yet healed in some locations, but only position 23 has an unhealed bone defect that is to be avoided during the preoperational planning of implant position (Figure 4).
Next steps are collection of impressions of the upper and lower jaw using putty and making of the models which are then scanned by extraoral scanner. Prosthetics are also scanned with CT.
Jaw impressions may also be taken digitally, with an intraoral scanner, but in the case of toothless patients classic impressions have been proven more precise through experience. If only a few teeth are replaced with implants, then the intraoral scanner is used.
The data collected (CT, jaw impressions and prosthetics scans) is filed and input into digital planning program. The patient is released until the next day when the operation is scheduled and surgical templates are made.
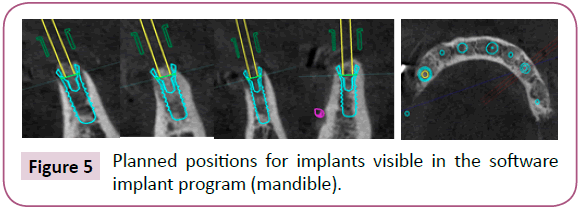
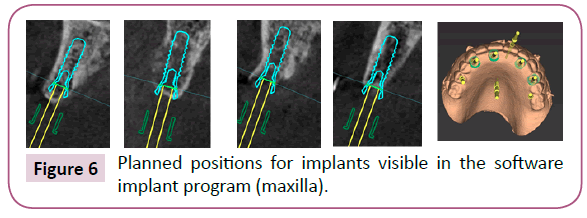
Upon inspecting the virtual image it is evident that the placement of the implant to the desired position is possible. The optimal position within the bone and the relation between the implant and the prosthetics are then planned (Figures 5 and 6).
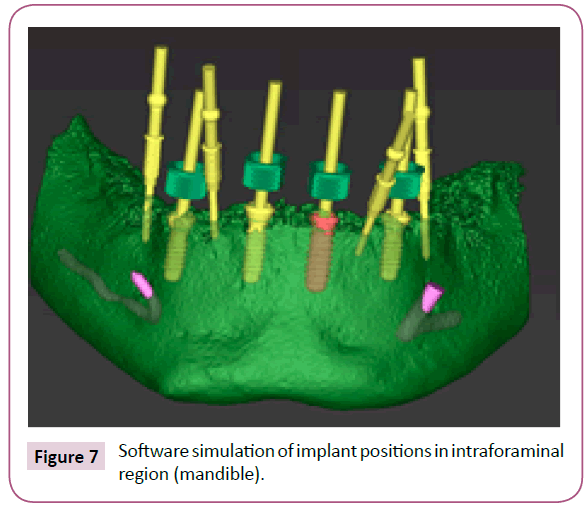
Within this procedure it is planned to place 4 implants in the lower and 4 in the upper jaw to serve as basis for the semi-fixed prosthesis (bar), so the implants are placed in the 'intraforaminal region' in both jaws, namely between 14 and 24 or 34 and 44 (Figure 7).
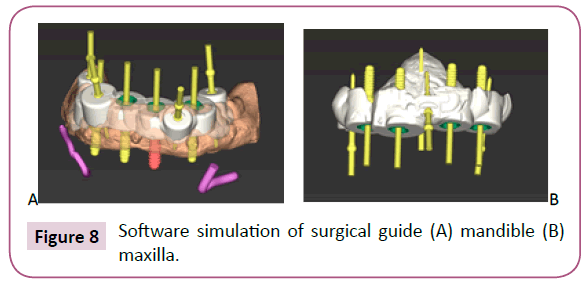
After a detailed plan and virtual implant placement, a surgical template is created and the locations and methods for its assembly are planned, as well as implant guidance systems (Figure 8).
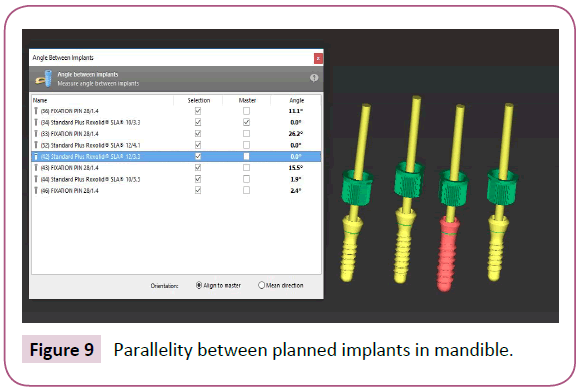
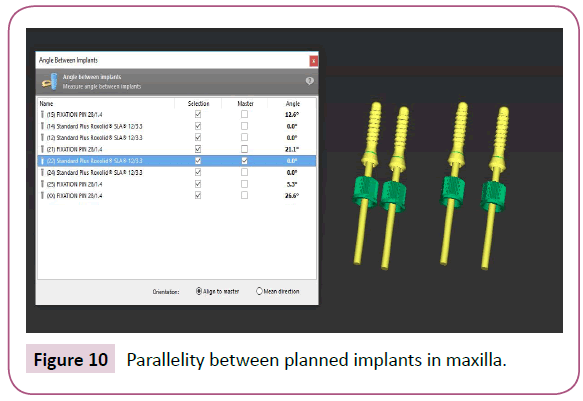
Everything is once again inspected and simulated by software (Figures 9 and 10) and the complete file is sent to the laboratory for the surgical template to be made by 3D printing and for the implant guidance systems to be installed for the planned procedure the next day.
On the day of the procedure the patient arrives and first has drugs and antibiotics administered and his oral cavity disinfected (chlorhexidine digluconate solution) [4]. Next, anesthesia is administered [3] and the patient is prepared for the procedure and covered with sterile dressing pad. Surgical template is sterilized in advance – surgical guides were first submerged into 70% ethanol solution for 20-25 min [5] and afterwars rinsed within chlorhexidine solution [4] and left in physiological solution until the beginning of the procedure.
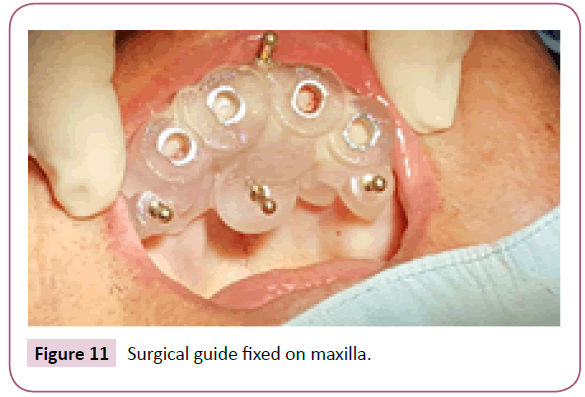
Surgical template is placed on the jaw and fixed with fixation screws (pins) so as not to move during the procedure (Figure 11).
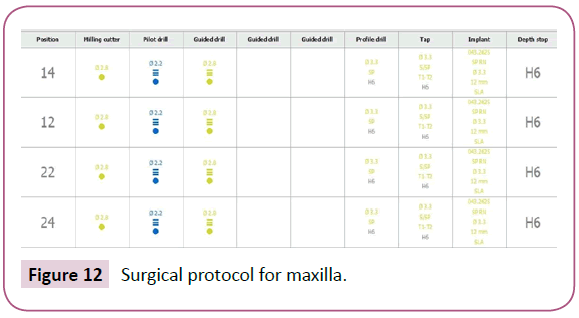
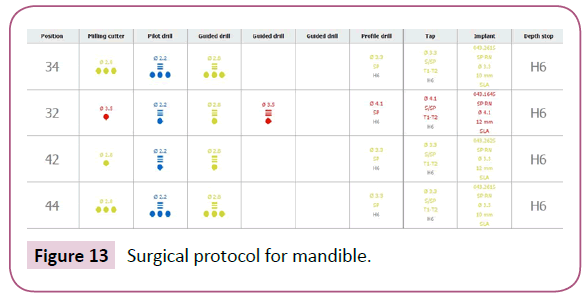
The operation continues as was planned virtually (Figures 12 and 13) and finally implants are placed on the depth specified in advance by the 3D bone position model.
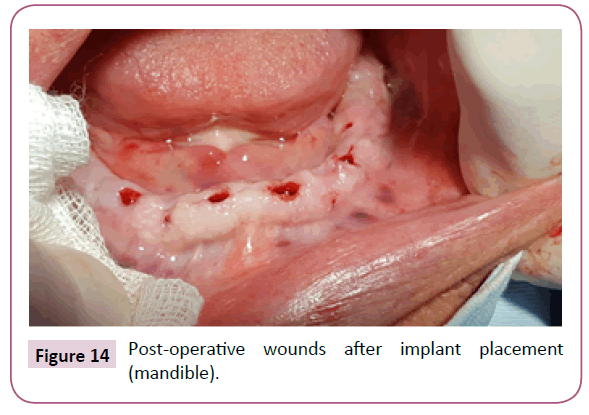
After the implants are placed, primary screws are positioned and then the surgical template can be removed from the jaw. As evident, due to flapless surgery and only gingiva punch opening through holes on surgical guide (Figure 14), postoperative wounds are minimal, which contributes to a more positive prognosis of the wound (implant) healing.
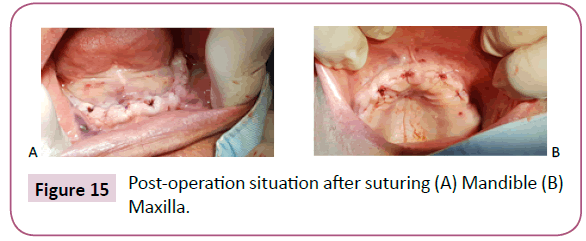
In such procedures it is possible for the removed part of the gum (gingiva punch) to be reattached to the same position above the implant, given that every step is planned in advance. In this case it is decided that the wounds are treated with PRF membrane, sutured closed and left to heal (Figure 15).
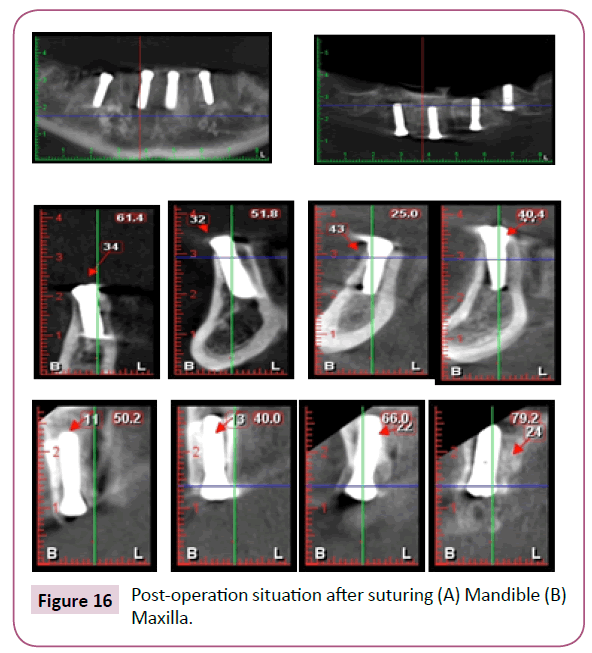
After the surgery the patient is referred to have a control X-ray to make sure the position of the implant in the bone corresponds the planned positions (Figure 16).
He is also informed about the importance of control examination and following the postoperative care instructions. Implant uncovering is scheduled in 4 to 5 months.
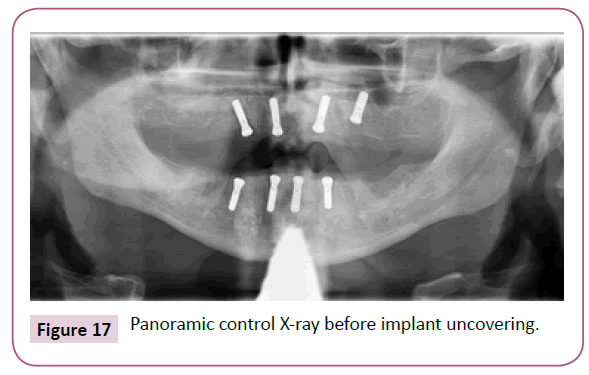
After the osseointegration period is completed, the patient comes in for the implant uncovering. Control image is done and it is evident that the situation and implant position is identical to the image done postoperatively. (Figure 17).
Gingiva formers are installed, prosthesis is once again lined so the patient can continue to use the temporary prosthetics. The patient is referred to have implant impression made and to continue therapy with his primary care physician.
Discussion
This article showed to us the demands from both the clinicians and the patients. They all want safer, quickier, painless implant placement with predictable results. Guided surgery is for sure one of methods how to fulfill the needs from profession and to satisfy patients. In the literature there are many articles and authors who disovered the concept of guided surgery superior to the conventional implant placement. They all agree that there are advantages from which the following can be highlighted: Precision, safety, less invasive for patient, lesser swelling after implant placement, fewer number of visits and operations, easier treatment option for patients with strong anxiety of surgery and better prosthetic implant position in the bone [6-20]. In the other hand some authors did not found guided surgery as improvement in comparison with conventional implant placement but gives advantage in favor of guided surgery and flapless procedure only on the part of post-operative swelling [21-23].
Advantage of guided surgery can be pointed also in possibility of modifying the plan of the operational procedure depending on the existing situation in the mouth i.e., to remaining number of teeth , remaining quantity of the bone or to the teethless situations. As it is already known-we can differentiate 3 types of surgical guide support-tooth, tissue/mucosa and bone support [24]. That gives us range of possibility to adjust the surgical guide and the concept of guided surgery to our needs and to plan the implants knowing that the guide can be fixated in all three named situations or in combination of two of them. Here the situation is discutable because some authors defend the tooth supported guide surgery as superior while the others found combinations of tooth/mucosa or tooth/bone fixation to be superior [7,25]. When there is a word about guides there has to be noticeable disadvantage that if the oral situation after taking impression or taking a CT scan is changed on teeth (tooth extractions, fillings, newly done provisional or definitive prosthetic works) or on tissue (swelling, losing of keratinised part of gums) that will surely lead to alter fit of surgical guide and inaccuracies in placing implants [24].
We can go further and differentiate tooth supported guides on guides with full-lenght sleeves and the ones with sleeve lenght reduction. In the situations where we are dealing with hard bone at future implant position one of the complications could be overheating of bone to which follows necrosis and implant rejection [26]. Every modern implant system has water cooling during bone drilling but when we are drilling in situations like this the overall experience of operater is more important to deal with situation more than implant system alone. With guided implant placement situation is even more complicated because of the sleeves and surgery guide which additionally obstruct water cooling at the drilling hole causing higher temperatures at that place. Here the advantage goes to sleeve lenght reduction with opened space for the coolant at the cost of lower stability and risk for guide movement during drilling especially with mucosa or bone supported guides [7,10]. In procedures like this there has to be highlighted in operation plan that there is a need for gradual drilling along with abundant cooling.
In our case we were dealing with patient with compromised medical anamnesis, previous hearth surgery, normal bone quality and with potential risk for bacteriemia. Also for this patient the plan was to decrease the number of operations especially tooth extractions to minimalise the need for his medical therapy change. Respect that and knowing that the possibility for bacteriemia in flapless procedures is 3X lower in comparison with conventional flap opening [8]. We performed the operation with full lenght sleeve surgical guide and with tissue/mucosa support fixated with the pins to eliminate the risk of movement. Normally in other cases with clear medical anamnesis, when we have few solid teeth in the jaw and they do not interfere with future implant position, certainly we would choose combination of tooth and mucosa fixation for surgical guide [7,25].
Although the guided surgery is predictable procedure and step in advance in precision we at the moment still can not perfectly transfer the virtually planned implant position from software to the bone but that differences and deviations can be statistically significant or not depending on author [27,11,9,10,6,13]. The reason for that can be found in small percentual deviations when transferring the oral situation to software, taking an impression, scanning , printing models and surgical guides or in material contractions [27,28]. We can not also completly exclude technical problems of CT scans and pairing with virtual model, mistakes made in software according to plan because of longer learning curve [19] or level of operators experience in working with surgical guides which later affects to deviation in result [29]. Stability of guide on jaw before fixing with pins or drill movement in sleeve are also facts that will change the desired outcome. In the end if patient has limited mouth opening that is situation when operator has to switch on conventional way of implant placement due to lack of space to positionate surgical guide and afterwards enter with drill and proceed with drilling sequence.
Conclusion
As presented in this clinical case, today , using guided surgery and surgical guides in dentistry or implantology is a step forward in reaching more accurate safer and better performed oral operation and implant placement with predictable results. For patient this also means less pain and better post-operational recovery with doubtless satisfaction after finishing the procedure. But; because every patient is different and has his own personal and anamnestic records or desires it is hard to have identical treatment options for every patient or to measure success in every procedure. With guided surgery we are going in right direction to fulfill our defined goals but there is surely a lot of space to improve every aspect of named procedure. In the future the concept of guided surgery will be improved even more but this technique can be nowdays suggested to all clinicians ranged from inexperienced to well experienced.
References
- https://www.iti.org/SAC-Assessment-Tool
- https://www.ivoclarvivadent.com/en/p/all/products/removable-denture-prosthetics/materials-for-dentures/probase-cold
- https://www.ema.europa.eu/en/medicines/human/referrals/septanest-associated-names
- https://cdc.net.au/pdf/curasept-instructions.pdf
- Smith PN, Palenik CJ, Blanchard SB (2011) Microbial contamination and the sterilization/disinfection of surgical guides used in the placement of endosteal implants. Int J Oral Maxillofacial Implants 26: 274-281.
- Yatzkair G, Cheng A, Brodie S, Raviv E, Boyan BD, et al. (2015) Accuracy of computer-guided implantation in a human cadaver model. Clin Oral Implants Res 26: 1143-1149.
- Geng W, Liu C, Su Y, Li J, Zhou Y (2014) Stemness & niche sans frontiers - the cancer stem cell myth. J Stem Cells Regen Med 10: 1.
- Arisan V, Bölükbaşi N, Öksüz L (2013) Computer-assisted flapless implant placement reduces the incidence of surgery-related bacteremia. Clin Oral Investig 17: 1985-1993.
- Stübinger S, Buitrago-Tellez C, Cantelmi G (2014) Deviations between placed and planned implant positions: an accuracy pilot study of skeletally supported stereolithographic surgical templates. Clin Implant Dent Relat Res 16: 540-551.
- Zhao XZ, Xu WH, Tang ZH, Wu MJ, Zhu J CS (2014) Accuracy of computer-guided implant surgery by a CAD/CAM and laser scanning technique. Chin J Dent Res 17: 31-36.
- Fürhauser R, Mailath-Pokorny G, Haas R, Busenlechner D, Watzek G, et al. (2015) Esthetics of flapless single-tooth implants in the anterior maxilla using guided surgery: association of three-dimensional accuracy and pink esthetic score. Clin Implant Dent Relat Res 17: e427-e433.
- Youk SY, Lee JH, Park JM, Heo SJ, Roh HK, et al. (2014) A survey of the satisfaction of patients who have undergone implant surgery with and without employing a computer-guided implant surgical template. J Adv Prosthodont. 6: 395.
- Moon SY, Lee KR, Kim SG, Son MK (2016) Clinical problems of computer-guided implant surgery. Maxillofac Plast Reconstr Surg. 38: 15.
- Arcuri L, Lorenzi C, Cecchetti F, Germano F, Spuntarelli M, et al. (2016) Full digital workflow for implant-prosthetic rehabilitations: A case report. Oral Implantol 8: 114-121.
- De Vico G, Ferraris F, Arcuri L, Guzzo F, Spinelli D (2016) A novel workflow for computer guided implant surgery matching digital dental casts and CBCT scan. Oral Implantol 9: 33-48.
- Ciabattoni G, Acocella A, Sacco R (2017) Immediately restored full arch-fixed prosthesis on implants placed in both healed and fresh extraction sockets after computer-planned flapless guided surgery. A 3-year follow-up study. Clin Implant Dent Relat Res 19: 997-1008.
- Bencharit S, Staffen A, Yeung M, Whitley D, Laskin DM, et al. (2018) In vivo tooth-supported implant surgical guides fabricated with desktop stereolithographic printers: Fully guided surgery is more accurate than partially guided surgery. J Oral Maxillofac Surg 76: 1431-1439.
- Ravidà A, Barootchi S, Tattan MA, Saleh MHA, Gargallo-Albiol J, et al. (2018) Clinical outcomes and cost effectiveness of computer-guided versus conventional implant-retained hybrid prostheses: A long-term retrospective analysis of treatment protocols. J Periodontol 89: 1015-1024.
- Pinto A, Raffone C (2017) Postextraction computer-guided implant surgery in partially edentate patients with metal restorations: A case report. Oral Implantol 10: 71-77.
- Younes F, Cosyn J, De Bruyckere T, Cleymaet R, Bouckaert E, et al. (2018) A randomized controlled study on the accuracy of free-handed, pilot-drill guided and fully guided implant surgery in partially edentulous patients. J Clin Periodontol 45: 721-732.
- Pozzi A, Tallarico M, Marchetti M, Scarfò B, Esposito M (2014) Computer-guided versus free-hand placement of immediately loaded dental implants: 1-year post-loading results of a multicentre randomised controlled trial. Eur J Oral Implantol 7: 229-242.
- Marlière DAA, Demétrio MS, Picinini LS, De Oliveira RG, Netto HDDMC (2018) Accuracy of computer-guided surgery for dental implant placement in fully edentulous patients: A systematic review. Eur J Dent 12: 153.
- Colombo M, Mangano C, Mijiritsky E, Krebs M, Hauschild U, et al. (2017) Clinical applications and effectiveness of guided implant surgery: A critical review based on randomized controlled trials. BMC Oral Health 17: 1-9.
- Umapathy T, Anila B, Ashwini C, Jayam C (2015) Overview of surgical guides for implant therapy. J Dent Implant 5: 48.
- Pozzi A, Polizzi G, Moy PK (2016) Guided surgery with tooth-supported templates for single missing teeth: A critical review. Eur J Oral Implantol 9: 135-153.
- Trisi P, Berardini M, Falco A, Podaliri Vulpiani M, Perfetti G (2014) Insufficient irrigation induces peri-implant bone resorption: An in vivo histologic analysis in sheep. Clin Oral Implants Res 25: 696-701.
- Schneider D, Schober F, Grohmann P, Hammerle CH, Jung RE (2015) In-vitro evaluation of the tolerance of surgical instruments in templates for computer-assisted guided implantology produced by 3-D printing. Clin Oral Implants Res 26: 320-325.
- Flügge T, Derksen W, Te Poel J, Hassan B, Nelson K, et al. (2017) Registration of cone beam computed tomography data and intraoral surface scans-A prerequisite for guided implant surgery with CAD/CAM drilling guides. Clin Oral Implants Res 28: 1113-1118.
- Rupaimoole R, Lee J, Haemmerle M, Ling H, Previs RA, et al. (2015) Long noncoding RNA ceruloplasmin promotes cancer growth by altering glycolysis. Cell Reports 13: 2395-2402.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences