Correlated Diabetes Mellitus and Tuberculosis: The Challenge Continues
Ankita Pandey, Shivangi and Laxman S. Meena*
CSIR-Institute of Genomics and Integrative Biology, India
- *Corresponding Author:
- Laxman S. Meena
CSIR-Institute of Genomics and Integrative Biology, India.
Tel: 011-27002200
Fax: 011-27667471
E-mail: laxmansm72@yahoo.com
Received Date: August 09, 2018; Accepted Date: August 14, 2018; Published Date: August 20, 2018
Citation: Pandey A, Shivangi P, Meena LS (2018) Correlated Diabetes Mellitus and Tuberculosis: The Challenge Continues. J Mol Cell Biochem Vol.2 No.1:7
Abstract
Co-relation between diabetes and tuberculosis (TB) creates dual burden of this disease worldwide. This bi directional association necessitates special attention and thus detailed study on human immune system regarding this is necessary. It is very important to develop some good strategies for prevention of diabetes in patients who are exposed to Mycobacterium tuberculosis (M. tuberculosis). Both these diseases are negatively affecting each other as individual with tuberculosis may frequently attain hyperglycaemic condition in diabetic patients and on the other side anti diabetic drugs may also interact with anti tuberculosis drugs in many ways to decreases their efficacy. This review provides recent estimates of TB and diabetes incidence and mortality in the world. In this review, we summarize the current clinical and immunological studies on co-relation between diabetes and TB and what can be done for prevention of these diseases, and spread awareness of this unfavourable co-relation between communicable and non communicable disease which can cause serious threat to public health.
Keywords
Mycobacterium tuberculosis; Alveolar macrophages; Pathogenesis; Diabetes mellitus; Phagolysosome
Abbreviations
TB: Tuberculosis; M. tuberculosis: Mycobacterium tuberculosis; DM: Diabetes Mellitus WHO: World Health Organization; IFN-γ: Interferon γ; IL: Interleukin; TNF-α: Tumour Necrosis Factor-α
Introduction
Tuberculosis (TB) caused by Mycobacterium tuberculosis H 37Rv (M. tuberculosis ) is one of the oldest known human disease whose risk increases day by day and become fatal [1,2]. Ability of M. tuberculosis to utilize macrophages for its replication enables it to survive and further cause disease [3]. There were 53 million cases of TB reported by WHO in all over world during 2000- 2016. TB is the 9th cause of death worldwide and 1st in case of infectious disease [4]. Controlling TB is a global health issue which becomes more challenging because of its association with social and economic conditions [5]. M. tuberculosis has co-evolved with humans for years. TB detected in a fossil of Pleistocene bison is the oldest evidence of presence of M. tuberculosis. Robert Koch received a Nobel Prize in 1905 for the discovery of bacillus causing TB, M. tuberculosis [6]. The double burden of TB and diabetes has attracted much attention in the past decade. The co-relation between these two diseases is a serious threat to public health. Type 2 diabetic patients have a weak immune response and hence are prone to catch infections including TB. Almost one-third of the total population in the world is infected with M. tuberculosis. This bacterium remains inactive in some individual in the initial stage and in later stage of life it could become active and cause disease especially in people who suffers from diabetes [7,8]. Response of diabetic patients to initial phase of anti TB treatment is slow and almost 8-10% of tuberculosis cases are linked to diabetes all over the world. 2-3 fold culture positive TB is shown in some studies after 3 months of treatment [9,10]. Diabetes is co-related with failure of treatment in TB as well as deterioration of health after improvement. Disease control program will need to expand their efforts to cure patients with diabetes mellitus (DM) and TB [11,12]. This co- relation between DM and TB is one of the major concerns for immunologists and clinicians [13].
Literature Review
Factors associated with Diabetes Mellitus (DM) and Tuberculosis (TB)
Age- The data available regarding this factor is not enough to conclude the extent of its contribution in diabetic TB patients. However, a case study in California and Mexico has shown decrease in association between DM and TB with increase in age [14,15]. Association of TB with DM is more dominant in younger population. DM patients who are using insulin are at higher risk of tuberculosis [16].
Sex- It is found that in some cases men have strong association but other suggests that there is higher risk in women. Relationship with sex varies by age and it is observed that higher proportion were women in older age and men in younger age. Although the association with sex is not very clear [14,17,18].
Prevalence
In the Middle East, prevalence of DM and TB is estimated to be 15.2 million people with positive diagnosis. It is expected that, this will be increasing around 42.6 million by 2030. Global report noted that every one person in three is infected [19]. In one of the study it has been found that, tuberculosis rate vary in diabetic patients between 1.6 and 2.8 millions. Tuberculosis is ten times more common in diabetic patients in comparison to non diabetic patients [20]. Prevalence of TB in DM patients is higher in countries of Asia although the global prevalence is low. Former studies show higher prevalence of TB among diabetic patients in low and middle income countries [21,22]. Also it is reported that screening of TB among DM patients were detected with high rate of prevalent TB. According to a research it is clearly shown that the large population affected with TB are those in which TB is relapsed after having DM [23].
Poverty
Low income countries are more prone in catching infection of communicable disease. Though, the burden of non communicable disease found to be 47% in year 1990 and is predicted to be increased by 69% by year 2020 in low income countries [9]. Increasing rates of industrialization and urbanisation directs higher rates of obesity and diabetes. The number of people with diabetes, which was 171 million in 2000, is expected to grow to 366 million–440 million by 2030, with three-quarters of patients with diabetes living in low-income countries [24].
Non functional immunity to M. tuberculosis in DM patients
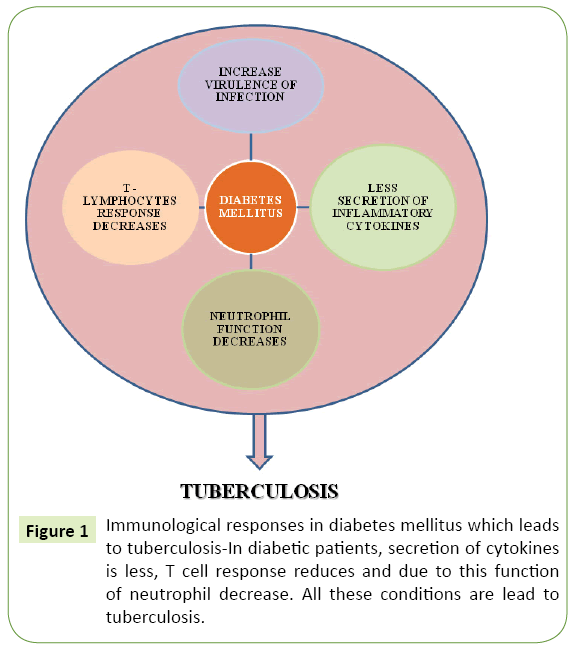
Macrophage activation by T cell inhibits M. tuberculosis replication and restricts this disease for life time in infected humans [25]. Conversion of active disease from inactive infection is higher with T-cell deficiency or loss of cytokine function (IFN-γ, IL-12, TNF-α). Immune cells and cytokines increase in circulation of diabetic patients co infected with tuberculosis [26]. Granulomatous sores are seen in various areas of the head and neck and a troublesome symptomatic test for the radiologist. Infective granulomas might be because of bacterial or parasitic operators. Noninfective granulomas are Wegener's granulomatosis, sarcoidosis, amyloidosis, compound granuloma and reparative goliath cell granuloma [27-29]. Current research suggests reduction in the association of monocytes with M. tuberculosis in diabetic patients which ultimately results in decreased opsonin and C3 component of the compliment system which play an important role in phagocytosis of the pathogen [30,31]. Cell mediated immune response is activated by efficient phagocytosis of M. tuberculosis which restrict its initial growth but this phagocytosis dramatically decreases in chronic diabetic patients and this delay subsequently plays an important role in increasing the risk of tuberculosis infection and persistence shown in Figure 1 [32].
Figure 1: Immunological responses in diabetes mellitus which leads to tuberculosis-In diabetic patients, secretion of cytokines is less, T cell response reduces and due to this function of neutrophil decrease. All these conditions are lead to tuberculosis.
Discussion
Impact of diabetes on TB treatment
DM is often associated with M. tuberculosis clearance which is delayed during treatment in diabetic patients and sometimes treatment failure, relapse or death has also been reported [33]. The anti-TB drug therapy involves wide range of drugs, which can develop adverse drug reaction in patients. If we use anti DM medication, it can be interact with anti tubercular drugs. It is necessary to eliminate the factors which are associated with adverse reaction of anti TB medication which might leads therapy success [34]. DM has been associated with all mortality cases in patients having TB and mostly death is reported in case of pulmonary TB [35,36]. Drug toxicity, mainly in hepatocytes will increase due to diabetes therefore; death chances will be 6 times higher in diabetic TB patients [16].
Comparative study of TB patients with and without diabetes
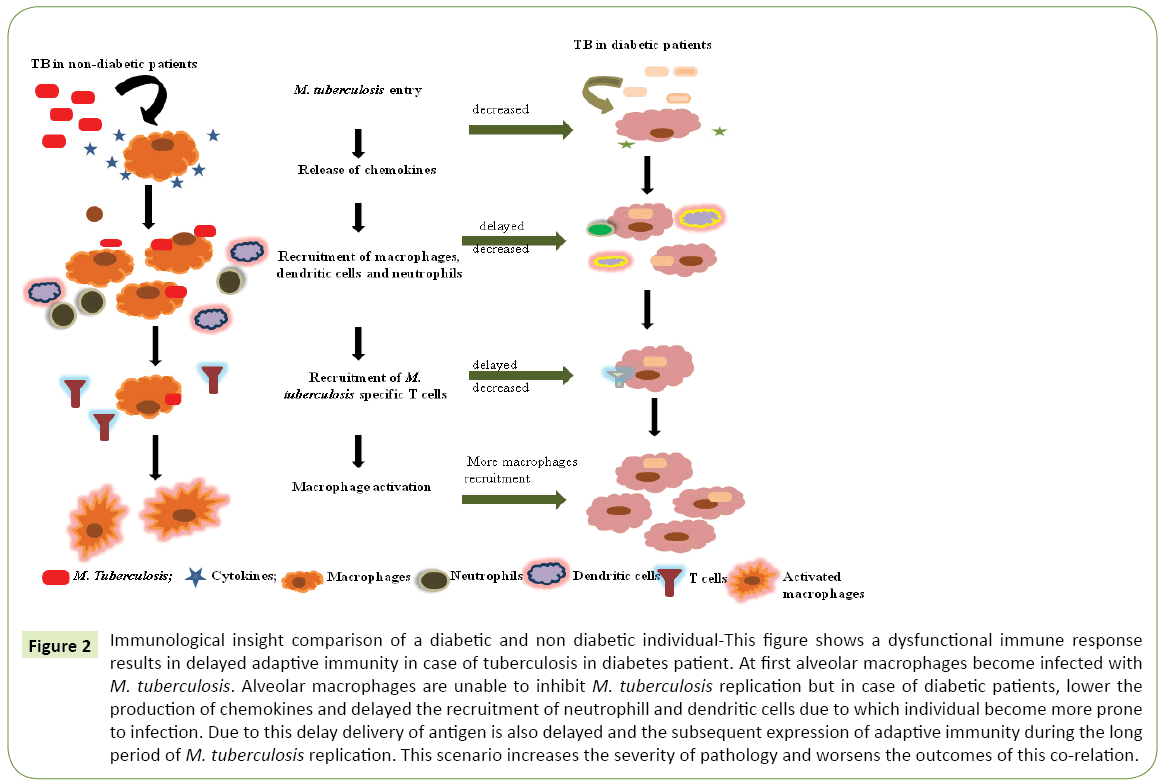
If we compare diabetic individual with non diabetic, then we can see the dominance of re infection or relapse. We can conclude that anti tuberculosis drugs will fail to treat infection. Some evidences suggest that T cell response in diabetic patients is greater quantitatively but functionally it is less effective than the non diabetic patient’s response as shown in Table 1 [26]. Common symptoms are almost same including cough, fever and weight loss. According to several studies, in diabetic patients prevalence of haemoptysis is higher and prevalence of dyspnea and loss of appetite is higher in non diabetic patients [19]. Large number of smear positive results in TB patients with DM in comparison with patients of TB without DM was observed. According to a study also risk of relapse in TB patients with DM shows increase of four fold versus TB without DM [30]. Former study on TB patients of southern Texas and northern Mexico shows that in diabetic patients, production of IFN-γ, IL-2, TNF-α, and GM-CSF is higher than non diabetic TB patients as shown in Figure 2 [25].
| S. No. | Criteria | TB in diabetic patients | TB in non-diabetic patients | References |
|---|---|---|---|---|
| 1. | T-cell response | Quantitatively -greater | Quantitatively-lesser | [26] |
| Functionally - less effective | ||||
| Functionally- more effective | ||||
| 2. | Common symptoms | Cough | Cough | [19] |
| Fever | Fever | |||
| Loss of appetite | Weight loss | |||
| 3. | Risk relapse | 4-fold increase | Lesser chance | [30] |
Table 1: T-cell response in TB patients with diabetes and without diabetes.
Figure 2: Immunological insight comparison of a diabetic and non diabetic individual-This figure shows a dysfunctional immune response results in delayed adaptive immunity in case of tuberculosis in diabetes patient. At first alveolar macrophages become infected with M. tuberculosis . Alveolar macrophages are unable to inhibit M. tuberculosis replication but in case of diabetic patients, lower the production of chemokines and delayed the recruitment of neutrophill and dendritic cells due to which individual become more prone to infection. Due to this delay delivery of antigen is also delayed and the subsequent expression of adaptive immunity during the long period of M. tuberculosis replication. This scenario increases the severity of pathology and worsens the outcomes of this co-relation.
Can we reduce tuberculosis by targeting diabetes?
DM can hamper the treatment of TB. We can decrease the mortality rate of TB by preventing diabetes. If diabetes continues to increase at current rate, it will tedious to prevent TB. We can say if we target diabetes as one of the associated factors of TB, it will optimize treatment response of TB [22]. According to journal of Diabetes and metabolism, it is discovered that if beta cells are treated with vitamin D or derivative of vitamin D (eg. LCA propionate) it can protect the function of beta cells by enhancing the expression of genes which encodes insulin [37]. Thus we can conclude that it will prevent or cure diabetes and through this mechanism, we can indirectly reduce TB because vitamin D deficiency is also one of the associated factors with higher risk of TB. Individuals, who are vitamin D deficient, also have susceptibility to develop TB and also disease progression get worsen in these individual if infected with TB. Anti mycobacterial activity is also promoted by vitamin D supplement [38]. Vitamin D treatment inhibits mycobacterial entry and also restricts its survival within macrophage. Therefore it could predict that, the burden of this co infection of TB and DM could be managed simultaneously through supplement of vitamin D [39,40].
Conclusion
Rare co relation between communicable and non communicable diseases such as the one seen in Tuberculosis and diabetes has created problems in treating both simultaneously. This association is the next challenge for controlling global burden of tuberculosis. Some Novel therapeutic approaches should be designed which can target the hindrance created by diabetes in the treatment of TB, as immune cell in diabetic individual show less efficiency to kill M. tuberculosis. Hence, designing new drug pipelines that can target TB and diabetes simultaneously is vital so that we can enhance the interaction between macrophages and M. tuberculosis. If it is possible to deal with immune compromise stage of diabetes then we can cure or prevent TB lead by diabetes. Cross-sectional imaging methods, for example, CT and MR imaging, depend on morphologic criteria for the evaluation of pneumonic and mediastinal tumors [41-43]. Addressing co-relation between DM and M. tuberculosis transmission is crucial to achieve control of these diseases in high burden cities. Repeated surveys measuring tuberculosis infection in diabetic patients in the same community involving young individuals can give us an estimate of tuberculosis transmission. This strategy can be used in high burden urban areas to calculate transmission of tuberculosis and develop strategies to reduce its progression. Priority should be given to the development of health assessments to eradicate diabetes from population to achieve support in TB prevention stratagem.
Acknowledgements
The authors acknowledge financial support from the Department of Science and Technology-SERB, Council of Scientific and Industrial Research-Institute of Genomics and Integrative Biology under the research project GAP0145.
References
- Harries AD, Dye C (2006) Tuberculosis. Ann Trop Med Parasitol 100: 415-431.
- Smith I (2003) Mycobacterium tuberculosis pathogenesis and molecular determinants of virulence. Clin Microbiol Rev 16: 463-496.
- Chopra P, Meena LS, Singh Y (2003) New drug targets for Mycobacterium tuberculosis. Indian J Med Res 117: 1-9.
- (https://www.who.int/tb/publications/global_report/gtbr15_main_text.pdf)
- Raviglione M, Sulis G (2016) Tuberculosis in 2015: Burden, challenges and strategy for control and elimination. Infect Dis Rep 24: 6570.
- Sandhu GK (2011) Tuberculosis: Current situation, challenges and overview of its control programs in India. J Glob Infect Dis 3: 143-150.
- Sullivan T, Amor YB (2012) The co-management of tuberculosis and diabetes: Challenges and opportunities in the developing countries. PLoS Med 9: e1001269.
- Agarwal AK, Gupta G, Gupta P, Dwivedi S, Swamai P (2006) The association between diabetes and tuberculosis may be the next challenge for global tuberculosis control worldwide. Indian J Endocrinol Metab 20: 732-733.
- Jeon CY, Murray MB, Baker MA (2012) Managing tuberculosis in patients with diabetes mellitus. Expert Rev Anti Infect Ther 10: 836-868.
- Restrepo BI (2007) Convergence of the tuberculosis and diabetes epidemics: Renewal of old acquaintances. Clinical Infectious Diseases 45: 436-438.
- Reis-Santos B, Gomes T, Locatelli R, De Oliveira ER, Sanchez MN, et al. (2014) Treatment outcomes in tuberculosis patients with diabetes: A polytomous analysis using Brazilian Surveillance System. PLoS One 9: e100082.
- García-Elorriaga, Rey-Pineda D (2014) Type 2 diabetes mellitus as a risk factor for tuberculosis. J Mycobac Dis 4: 144.
- Yorke E, Atiase Y, Akpalu J, Sarfo-Kantanka A, Boima V, et al. (2017) The bidirectional relationship between tuberculosis and diabetes. Tuberc Res Treat 20: 1701-2578.
- Stevenson CR, Critchley JA, Forouhi NG, Roglic G, Williams BG, et al. (2007) Diabetes and the risk of tuberculosis: A neglected threat to public health?. Chronic Illn 3: 228-245.
- Casqueiro J, Casqueiro J, Alves C (2012) Infections in patients with diabetes mellitus: A review of pathogenesis. Indian J Endocrinol Metab 16: S27-36.
- Baghaei P, Marjani M, Javanmard P, Tabarsi P, Masjedi MR (2013) Diabetes mellitus and tuberculosis facts and controversies. J Diabetes Metab Disord 20: 58.
- Dyck RF, Klomp H, Marciniuk DD, Tan L, Stang MR, et al. (2007) The relationship between diabetes and tuberculosis in Saskatchewan people. Can J Public Health 98: 55-59.
- Pérez-Guzmán C, Vargas MH, Torres-Cruz A, Pe´rez-Padilla JR, Furuya MEY, et al. (2003) Diabetes modifies the male: female ratio in pulmonary tuberculosis. Int J Tuberc Lung Dis 7: 354-358.
- Baghaei P, Tabarsi P, Abrishami Z, Mirsaeidi M, Faghani YA, et al. (2010) Comparison of pulmonary TB patients with and without diabetes mellitus type II. Tanaffos 9: 13-20.
- Mugusi F, Swai ABM, Alberti KGMM, Mclarty DG (1990) Increased prevalence of diabetes mellitus in patients with pulmonary tuberculosis in Tanzania. Tubercle 71: 271-276.
- Workneh MH, Bjune GA, Yimer SA (2017) Prevalence and associated factors of tuberculosis and diabetes mellitus comorbidity: A systematic review. PLoS One 12: e0175925.
- Harries AD, Kumar AM, Satyanarayana S, Lin Y, Zachariah R, et al. (2016) Addressing diabetes mellitus as part of the strategy for ending TB. Trans R Soc Trop Med Hyg 110: 173-179.
- Mave V, Nimkar S, Prasad H, Kadam D, Meshram S, et al. (2017) Tuberculosis screening among persons with diabetes mellitus in Pune, India. BMC Infect Dis 17: 388.
- Boutayeb A (2006) The double burden of communicable and non-communicable diseases in developing countries. Trans R Soc Trop Med Hyg 100: 191–199.
- Horsburgh RC Jr (2004) Priorities for the treatment of latent tuberculosis infection in the United States. N Engl J Med 13: 2060-2070.
- Martinez N, Kornfeld H (2014) Diabetes and immunity to tuberculosis. Eur J Immunol 44: 617-626.
- Razek AA, Castillo M (2010) Imaging appearance of granulomatous lesions of head and neck. Eur J Radiol 76: 52-60.
- Abdel Razek AA (2016) Imaging of connective tissue diseases of the head and neck. Neuroradiol J 29: 222-230.
- Abdel Razek A, Al-Adlany M, Alhadidy A, Atwa M, Abdou N (2017) Diffusion tensor imaging of the renal cortex in diabetic patients: Correlation with urinary and serum biomarkers. Abdominal Radiol 42: 1493-1500.
- Gomez DI, Twahirwa M, Schlesinger LS, Restrepo BI (2013) Reduced Mycobacterium tuberculosis association with monocytes from diabetes patients that have poor glucose control. Tuberculosis 93: 192-197.
- Restrepoa BI, Schlesinger LS (2014) Impact of diabetes on the natural history of tuberculosis. Diabetes Res Clin Pract 106: 191-199.
- Vallerskog T, Martens GW, Kornfeld H (2010) Diabetic mice display a delayed adaptive immune response to Mycobacterium tuberculosis. J Immunol 1: 6275-6282.
- Root HF (1934) The association of diabetes and tuberculosis. N Engl J Med 210: 1-13.
- Siddiqui AN, Khayyam KU, Sharma M (2016) Effect of diabetes mellitus on tuberculosis treatment outcome and adverse reactions in patients receiving directly observed treatment strategy in India: A Prospective study. Biomed Res Int 2016: 7273935.
- Baker MA, Harries AD, Jeon CY, Hart JE, Kapur A, et al. (2011) The impact of diabetes on tuberculosis treatment outcomes: a systematic review. BMC Med 1: 81.
- Dooley KE, Tang T, Golub JE, Dorman SE, Cronin W (2009) Impact of diabetes mellitus on treatment outcome of patients with active tuberculosis. Am J Trop Med Hyg 80: 634-639.
- Rajni, Meena LS (2011) Unique characteristic features of Mycobacterium tuberculosis in relation to Immune system. Am J Immunol 7: 1-8.
- https://www.medicalnewstoday.com/articles/319719.php
- Kearns MD, Tangpricha V (2014) The role of vitamin D in tuberculosis. J Clin Transl Endocrinol 1: 167-169.
- Meena LS, Rajni P (2010) Survival mechanism of pathogenic Mycobacterium tuberculosis H37Rv. FEBS J 277: 2416-2427.
- Razek AA (2012) Diffusion magnetic resonance imaging of chest tumors. Cancer Imaging 12: 452-463.
- Sepahdari AR, Politi LS, Aakalu VK, Kim HJ, Razek AA (2014) Diffusion-weighted imaging of orbital masses: multi-institutional data support a 2-ADC threshold model to categorize lesions as benign, malignant, or indeterminate. AJNR Am J Neuroradiol 35: 170-175.
- Abdel Razek AA, Gaballa G, Denewer A, Tawakol I (2010) Diffusion weighted MR imaging of the breast. Acad Radiol 17: 382-386.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences