Anatomopathological Profile of Primary Focal and Segmental Glomerulosclerosis in Children in Dakar: A Case Report of 61 Cases
Kéita Y1, Dial CM4, Sylla A1, Sow A1*, Ly F5, Faye M2, Nzambaza JD2, Ndongo AA3, Ka El HF2, Diouf B3 and Sall MG1
1Service de Pédiatrie Du CHU A. Le Dantec, Dakar, Sénégal
2Service de Néphrologie Du CHU A. Le Dantec, Dakar, Université Cheikh AntaDiop, Sénégal
3Service de Pédiatrie De L’Hôpital D’Enfants, Albert Royer CHU Fann, Dakar, Sénégal
4Service d’Anatomopathologie De L’Hôpital Grand Yoff, Dakar, Sénégal
5Service de Pédiatrie De L’hôpital De Pikine, Dakar, Sénégal
- *Corresponding Author:
- Sow Amadou
Interne des hopitaux De dakar, Hôpital
Aristide Le Dantec, Université Cheikh
AntaDiop, Sénégal
Tel: 00221772690111
E-mail: amadousoow@hotmail.com
Received Date: Sep 13, 2017 Accepted Date: Nov 17, 2017 Published Date: Nov 20, 2017
Citation: Kéita Y, Dial CM, Sylla A, SowA, Ly F, et al. (2017) Anatomopathological Profile of Primary Focal and Segmental Glomerulosclerosis in Children in Dakar: A Case Report of 61 Cases. Jour Ren Med. Vol.1 No.3: 13.
Abstract
Introduction: Focal and Segmental Glomerulosclerosis (FSGS) associates three types of glomerular lesions: Cellular alterations which are initially on podocytes; hyaline deposits and sclerosis. Our objective was to classify focal and segmental glomerulosclerosis (FSGS) lesions found in children in Dakar.
Patients and methods: This was a retrospective and descriptive study during the period starting from the 1st of January 1994 to 31st December 2014. Were included in the study patients aged 0 to 15 years and presenting at least one FSGS typical glomerular lesion according to the Columbia 2004 classification.
Results: Of the 150 renal biopsies performed on the children, 40.7% (n=61) presented typical FSGS lesions. The average age of children was 11.07 ± 3.81 years. The sexratio was 1.34. Nephrotic syndrome was found in 93.4% (n=57) of the children, and renal biopsy was performed for steroid resistance in 54.4% (n=31) of them. Optical microscopy (OM) was used in 100% of the cases and immunofluorescence (IF) performed in 52.5% (n=32) of them. IF was positive in 56.30% (n=18). FSGS classic form of represented 67.2% (n=41) of the cases, cellular FSGS 14.7% and collapsing FSGS 10% of them. Etiological research was negative in all of our patients. The Progression was précised in only 26.22% (n=16) of cases with half of them 50% (n=8) already on end stage renal disease.
Conclusion: FSGS revealed itself through steroid resistance in 54.4% in our series. Renal biopsy showed a higher occurrence of the classic form.
Keywords
Children; Nephrotic syndrome; Senegal; Steroid resistance
Introduction
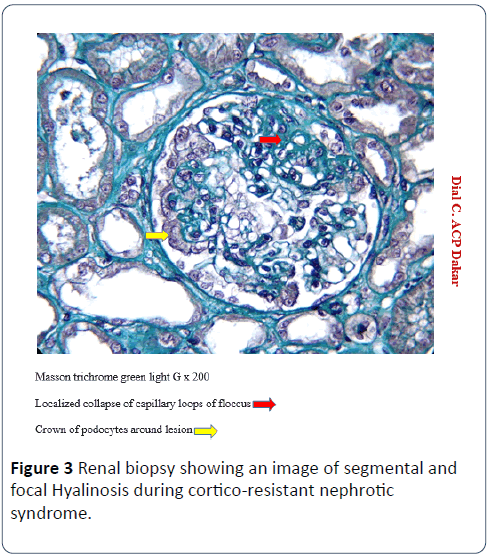
Segmental and Focal Hyalinosis (SFH) associates three types of glomerular lesions: initially podocytic cell alterations, hyaline deposits and sclerosis [1,2]. These lesions are called segmental when they partially involve the glomerulus or focal areas when all the glomeruli are not affected [3,4]. For a standardized approach, the classification of Columbia 2004 proposes five morphological subgroups of SFH: the classical (non-specific) form, the perihelial form (vascular pole), the cellular form (endocapillary hypercellularity), the collapsing (destructive) form and The SFH of the tubular pole ("Tiplesion") [5,6]. In most cases, SFH is found in children with steroid-resistant nephrotic syndrome (NS) and progresses to chronic renal failure (CKD) in 20-30% of patients [1-4]. Data on SFH in children in Senegal are non-existent to our knowledge. Our objective in this study was to classify histologically the lesions of SFH found in children in Dakar.
Materials and Methods
This study was conducted in the Department of Pediatrics, Adult Nephrology and Anatomy Pathology of the Aristide Le Dantec Hospital (HALD) and in the Department of Pathology of the General Hospital of Grand Yoff (HOGGY). This was a descriptive retrospective study during the period from 1 January 1994 to 31 December 2014 (21 years). Renal biopsies were performed by nephrologists and/or pediatricians initially with Silverman 16G and 18G needles and then with the automatic pistol from 2013. For each child, two (02) fragments of kidney were taken of which One fixed in the mixture comprising Alcohol, Formol and Acid (AFA) for reading by optical microscopy (MO) and the other fixed in Michel's liquid for reading with immunofluorescence (IF). Between 1994 and 2009, the fragments were read in France in the university hospitals of Necker and Saint Louis. As of 2010, the presence of a renal histopathologist, trained in Necker, in Senegal, allowed reading of the kidney fragments on site. Patients aged 0-15 years and presenting at least one FSGS typical glomerular lesion according to the Columbia 2004 classification were included in this study (1:2). Patients without HSF lesions were excluded from the study. The diagnosis of primary SFH was retained in the absence of signs of systemic or general disease, either clinically, biologically or histologically. Nephrotic syndrome (SN) was defined as proteinuria >50 mg/kg/24 h associated with hypo-protidemia <60 g/L and hypo-albumin <30 g/L. Corticoresistance was defined as the persistence of SN after 4 weeks of oral prednisone at 2 mg/kg/day and three perfusions of methylprednisolone at 1 g/1.73 m2 body surface area. The data were obtained from the patient record, the biopsy application form, the biopsy register and the histopathological report. We studied the age, sex, geographic origin of patients, indications of renal biopsy and we classified primary lesions of SFH found according to the classification of Columbia 2004. The descriptive study was carried out by the calculation of Frequencies for the qualitative variables and the calculation of the means with their standard deviation for the quantitative variables using the SPSS 18.0 software. This study received approval n° 0223/2016/CER/UCAD of the research ethics committee of Cheikh Anta Diop, University in Dakar, Senegal.
Results
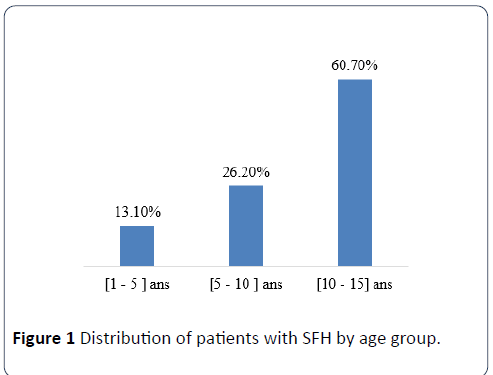
Of 150 kidney biopsies performed in children, 40.7% (n=61) had typical lesions of SFH. Children were of Senegalese nationality in 88.5% (n=54) of the cases and originating from neighboring countries of Senegal in 11.5% (n=7). The mean age was 11.07 ± 3.81 years, and those aged 10-15 accounted for 60.6% (n=37) of the cases (Figure 1). The sex ratio was 1.34. Nephrotic syndrome (NS) was present in 93.5% (n=57) of children. Renal biopsy puncture (PBR) was performed for isolated renal insufficiency without nephrotic syndrome in 6.5% (n=4) patients.
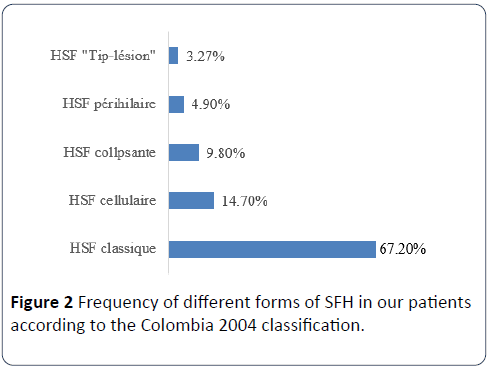
In patients with NS, PBR was performed for impurity criteria in 28.1% (n=16) patients, over age 12 years in 17.5% (n=10) and for corticosteroid in 54, 4% (n=31). Hematuria and renal insufficiency were found in 50% (n=18) of the children with impurity criteria and 37.5% (n=6) of the patients. OM was performed in 100% of cases and IF in 52.5% (n=32) of the cases. The IF was positive in 56.30% (n=18) with IgM deposits (90%), Complement C3 (85%), IgA (75%), albumin (65%), IgG (40%), C1q (20%) and fibrin (10%). Using the 2004 Columbia classification, the classical form of SFH accounted for 67.20% (n=41) of the cases, cellular SFH 14.7% (n=09), and collapsing SFH in 10% (n=06) of children (Figures 2 and 3). Etiological research was negative in all of our patients, particularly the search for HIV, diabetes and sickle cell anemia.
Nephroprotective therapy was initiated in all cases associated with low-dose corticosteroid therapy. Only 26.22% (n=16) of the cases could be specified. Half of them (50%) (n=8) had progressed to chronic terminal renal insufficiency (CRFI). Chronic hemodialysis was performed in 62.5% (n=5) of cases of HCFI by HSF.
Discussion
HSF accounted for 40.7% of lesions found during renal biopsy in children in Dakar. In Morocco, Bourquia et al. noted a frequency of 25% in a population of 88 children in whom a renal biopsy was performed [7]. In Congo Brazzaville, Mabiala- Babela et al. [8] described, on 26 biopsies performed in the adolescent, 38.4% of isolated or associated HSF lesions. Studies show the high frequency of HSF when renal biopsy is indicated in children.
The average age of our patients at the time of diagnosis was 11 years. Different studies have shown that the mean age at diagnosis of SFH varies between 6 and 7 years [9]. This difference in age with our study is due to the delayed realization of the renal biopsy due to the deficiency of nephrologists and histopathologists in sub-Saharan Africa. In our study, the primary indication for PBR was idiopathic nephrotic syndrome cortico-resistant (50.8%).
Nephrotic syndrome in particular cortico-resistant is the most frequent indication of renal biopsy in children and is often associated with SFH lesions [10-12]. This corticoresistance of SFH during renal biopsy in children is described in Morocco (83%) and Congo Brazzaville (23%). Other indications of renal biopsy revealing lesions of SFH were less frequent in our study compared to cortico-resistance. We found impure nephrotic syndrome in 26.2% (n=16), unexplained acute renal failure in 6.5% (n=4). According to the 2004 Columbia classification, the classical form accounted for 67.2% of the SFH lesions. The predominance of this form is estimated by Das et al. [13] to 44.6% in India and Swarnalatha et al. [14] to 62.2%. The frequency of cellular and collapsing forms varied between 4.6% in the Das study and 14.7% in our series. These studies show that the prevalence of SFH subtypes is different in these populations and that conventional SFH is the most frequently found.
In addition, the clinically, biochemically and histologically significant differences [13] reaffirm the usefulness of Columbia's classification in routine kidney biopsy reports. Especially since the degree of renal survival is different between the histological variants [9]. After renal transplantation, SFH recurrence affects up to 40% of patients after first transplantation and reaches 80% of patients for subsequent transplantation after a first episode of recurrence [9,13,15].
Conclusion
The prevalence of SFH subtypes is different in our study population. Conventional SFH was the most frequently described lesion in our series. The Columbia classification is useful in kidney biopsy reports. For our population, it is necessary to improve the reading of the kidney biopsies, especially since renal transplantation is authorized in Senegal since 2015.
References
- Binaut R, Maisonneuve N, Vanhille P (2004) Néphropathies glomérulaires. Orientation diagnostique et évolution. EMC 1: 110-120.
- Gubler MC (2010) Classification des néphropathies glomérulaires primitives. EMC: 1-6.
- Colombat M, Deleuze S, Callard P (2006) Lésions élémessntaires des glomérules chez l’adulte. EMC, Néphrologie 18: A-10.
- Niaudet P (2005) Syndromes Néphrotiques congénitaux et infantiles. Nephrol Ther 1: 63-70.
- Nochy D, Lefaucheur C, Bariety J (2009) Biopsie rénale: Les différentes techniques. Nephrol Ther 5: 314-330.
- D’agati VD, Fogo AB, Bruijn JA (2004) Pathologic classification of focal segmental glomerulosclerosis: A working proposal. Am J Kidney Dis 43: 368-432.
- Bourquia A, Louahlia S (1997) Le syndrome néphrotique chez l’enfant. MAG 65: 31-35.
- Mabiala-Babela JR, Pecko JF (2006) Le syndrome néphrotique chez l'adolescent congolais: Aspects cliniques et histologiques. Arch Pédiatr 13: 88-89.
- Tizki S, Lasry F, Khalifa HH (2013) Hyalinose segmentaire et focale primitive de l’enfant: Épidémiologie et facteurs pronostiques Nephrol Ther 9: 433-437.
- Printza N, Bosdou J, Pantzaki A (2011) Percutaneous ultrasound-guided renal biopsy in children: A single centre experience. Hippokratia 15: 258-261.
- Obiagwu PN, Aliyu A, Atanda AT (2014) Nephrotic syndrome among children in Kano: A clinicopathological study. Niger J Clin Pract 17: 370-374.
- Mubarak M, Lanewala A, Kazi JI (2009) Histopathological spectrum of childhood nephrotic syndrome in Pakistan. Clin Exp Nephrol 13: 589-593.
- Das P, Sharma A, Gupta R (2012) Histomorphological classification of focal segmental glomerulosclerosis: A critical evaluation of clinical, histologic and morphometric features. Saudi J Kidney Dis Transpl 23: 1008-1016.
- Swarnalatha G, Ram R, Ismal KM (2015) Focal and segmental glomerulosclerosis: Does prognosis vary with the variants? Saudi J Kidney Dis Transpl 26: 173-181.
- Delville M, Sigdel T, Li L (2012) Une signature IgG prédictive de la récidive de hyalinose segmentaire et focale après la transplantation. Nephrol Ther 8: 259-277.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences