ISSN : ISSN: 2471-8416
Journal of Clinical & Experimental Orthopaedics
Shoulder joint infection with negative culture results: clinical characteristics and treatment outcome
European Conference on Orthopedics and Osteoporosis
November 29-30 , 2018 Amsterdam , Netherlands
Mohamed Attia Abdou, Ahreum Jo , Ik-Sun Choi, Chae-Jin Iim, Hyeng-Kyu Park, Hee-Kyun Oh, Sung-Min Kim and Myung-Sun Kim
Chonnam National University, South Korea
Posters & Accepted Abstracts: J Clin Exp Orthop
Abstract
Background: The incidence of septic arthritis of the shoulder joint is increasing as the population ages. The prevalence of the shoulder infection is also increasing due to the growing use of arthroscopy and expansion of procedures in the shoulder. Accurate diagnosis is required to get optimum treatment outcomes. However, cultures do not always identify all microorganisms even in symptomatic infection patients. The incidence of negative culture ranges from 0 to 25%. Few studies have reported the clinical features and treatment outcomes of culture-negative shoulder infections. Consequently, the aim of this study was to compare the clinical characteristics and treatment outcome of shoulder infections patients with negative culture and those with positive culture results. Our hypothesis suggests that culture-negative infections would have less favourable outcome. Methods: We retrospectively reviewed data from 36 patients with shoulder infection between Jun’ 2004 and Mar’ 2015, including 17 culture-negative and 19 culture-positive cases of shoulder infection. The minimum follow-up duration monitoring was 1.2 years (mean, 5±3.8 years; range, 1.2-11 years). We assessed patient’s preoperative demographic characteristics, laboratory markers, imaging and functional scores, in addition to evaluation of both intraoperative and postoperative findings between the two groups. Results: The culture negative patients, were 17 out of 36 (47.2%), showed lower WBC and CRP preoperative levels, and significantly lower number of repeated surgical debridement (culture negative/culture-positive=1.2±0.4/2.4±1.7) (p=0.002) with no osteomyelitis. In multiple logistic regression, the bony destruction on plain radiograph [odds ratio (OR) =9.686, 95% confidence interval (CI): 1.0-91.8] (p=0.04) and the number of surgical debridement (OR=5.3, 95% CI: 1.3-21.6) (p=0.02). There was no significant difference in age, gender, host conditions, initial diagnosis, preoperative symptoms, previous antibiotics treatment, other laboratory data or functional scores between the two groups. Conclusion: Culture-negative infection is less severe with no osteomyelitis and can be controlled better than culture-positive infection. Therefore, culture negativity is not necessarily a negative prognostic factor for shoulder joint infection.
Biography
E-mail:
maabdou84@gmail.com
Google Scholar citation report
Citations : 161
Journal of Clinical & Experimental Orthopaedics received 161 citations as per Google Scholar report
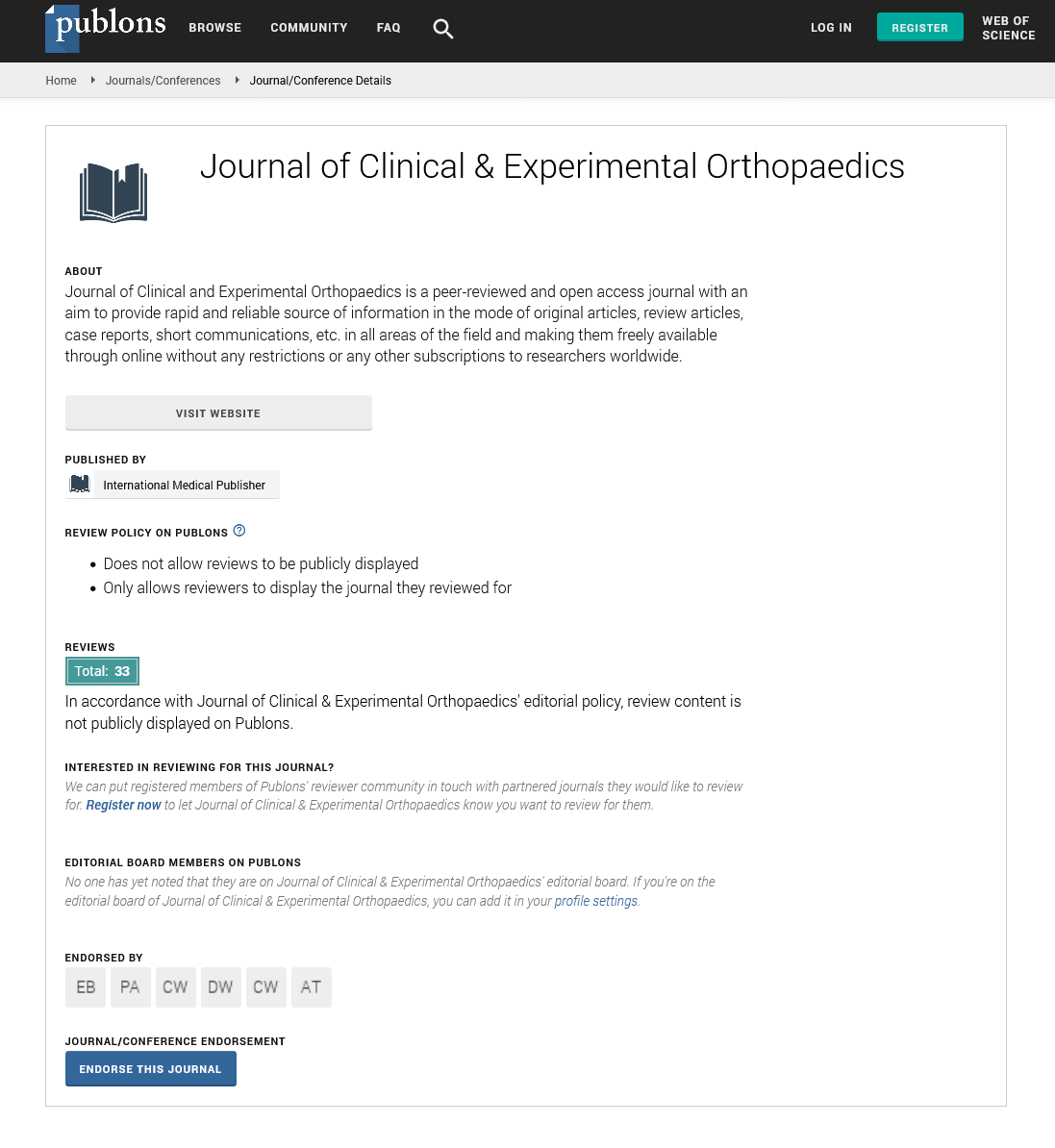
Journal of Clinical & Experimental Orthopaedics peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- China National Knowledge Infrastructure (CNKI)
- Directory of Research Journal Indexing (DRJI)
- WorldCat
- Publons
- Geneva Foundation for Medical Education and Research
- Secret Search Engine Labs
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences