Treatment Response among Asthmatics With & Without Reversible Airflow Limitation
Abdulgadir Attiah*
Department of Physics, Nabanji Medical Centre, Abha, Saudi Arabia
*Corresponding author: Abdulgadir Attiah, Department of Physics, Nabanji Medical Centre, Abha, Saudi Arabia, Tel No: 966598181581; E-mail: Atyaa291@ksau-hs.edu.sa
Received date: December 13, 2020; Accepted date: August 16, 2021; Published date: August 26, 2021
Citation: Attiah A (2021) Treatment Response among Asthmatics With & Without Reversible Airflow Limitation J Lung Vol: 2 No: 3.
Abstract
Background: Asthma is a chronic airway disorder associated with variable airflow limitation that is triggered by different stimuli. We aim to determine the treatment outcomes (improvement of FEV1 and number of asthma exacerbations) associated with the presence of airflow reversibility.
Methods: We conducted a retrospective cohort study, which included all adults diagnosed with asthma and performed a Pulmonary Function Test (PFT) at a tertiary care center in Saudi Arabia from January 2015 to December 2018. Smokers and patients with comorbidities that might affect the PFT were excluded. Exacerbations were defined as the need to use oral corticosteroids. A comparative analysis was done using the chi-square test.
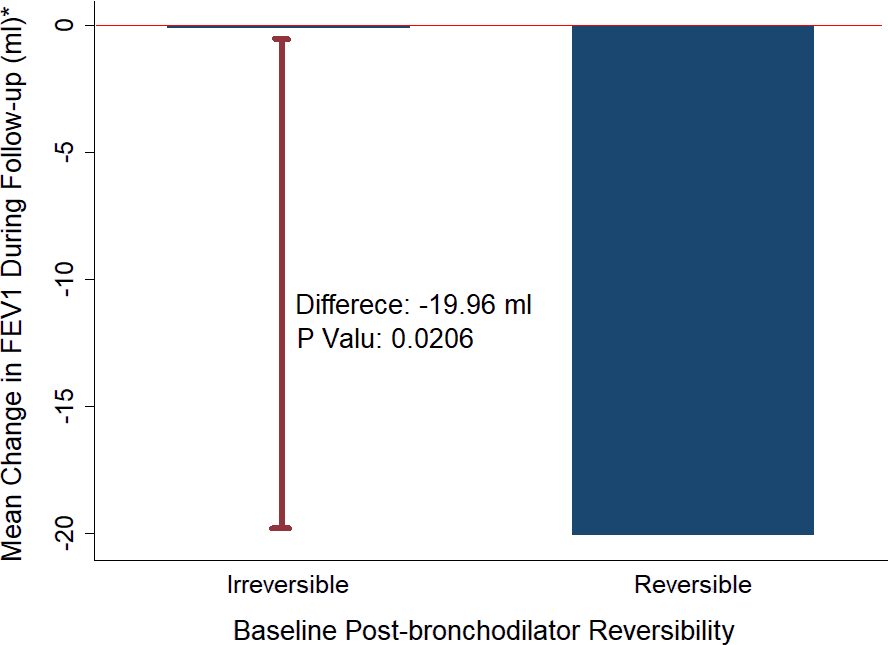
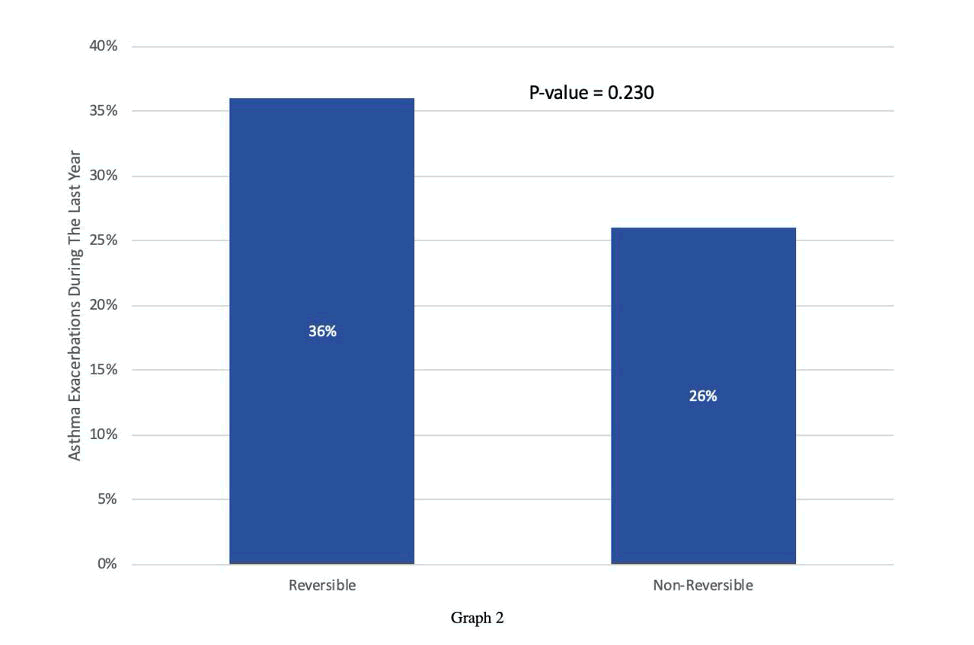
Results: 154 subjects were included, of which 42 subjects had reversibility and 112 did not. Asthmatics with baseline reversible airflow limitations had significant worsening of FEV1 during follow-up, compared to those with no reversibility, with a mean difference of 19.96mL (P-value = 0.0206). There was no significant association between having reversibility and experiencing an asthma exacerbation (P-value 0.23).
Conclusion: Reversibility of airflow was associated with significant worsening of FEV1, without significant effect on exacerbations, during follow-up of asthmatic patients.
Keywords: Asthma; Reversibility; Forced Expiratory volume 1; Exacerbations; Pulmonary Function Test.
Introduction
Asthma can be defined as a chronic respiratory disorder characterized by recurrent episodes of wheezing, shortness of breath, chest tightness, and/or cough along with expiratory airflow limitation that vary over time and in intensity (1–3). Although these classical symptoms are usually associated with asthma, they are still not definitive (1,2,4). Therefore, a thorough history accompanied by accurate diagnostic approaches such as peak expiratory flow, flow-volume relationships, and bronchodilator responses, which can be measured through spirometry, can result in a definitive diagnosis of asthma (1–5). Moreover, the clinical evaluation alone is not sufficient to establish the diagnosis, since it can also lead to the use of unrecognized terms to describe asthma such as reactive airway disease (6,7). This term may be appropriate for use in the pediatric population since it refers to transient cough and wheeze; however, in adults, it is considered unreliable and should be replaced with the term asthma (2,6,7). The use of spirometry is important to measure the reversibility of airflow limitation, which is the response of patients to bronchodilator medication and improvement in airflow (2,4).
WHO estimates that 235 million people currently suffer from asthma, and it is considered the most common non-communicable disease among children (5). Asthma is a public health problem in all countries regardless of the level of development (5). According to the Center for Disease Control and Prevention, asthma affects 25.7 million people in the United States (8). The Saudi Ministry of Health reports that the prevalence of asthma among the Saudi population is approximately 15-25%, including adults and children (9). A 2013 national study among adults in Saudi Arabia, determined that the prevalence of diagnosed asthma is 4.05% (95% Confidence Interval: 3.54-4.62%), a relatively low prevalence (10).
For centuries, clinicians have been trying to classify asthma into different phenotypes, as some phenotypes have a better response to treatment than others (11). Apart from allergic asthma, aspirin-exacerbated asthma, nonallergic asthma, infection-related asthma, and childhood pre-asthma phenotype, according to a review article, other phenotypes in the literature are categorized into “biomarker-based phenotypes”, “symptom-based phenotypes”, and “trigger-induced phenotypes” (11). Variability in airflow limitation post-bronchodilator use can be utilized to identify a phenotype of asthma with a particular response to certain medications. After conducting a review of the literature and to the best of our knowledge, no such studies have been conducted relating those two factors.
Materials and Methods
Population
All patients diagnosed with asthma and performed full Pulmonary Function Test (PFT) at King Abdulaziz Medical City, Jeddah between January 1st, 2014 to May 31st, 2019 were evaluated. Patients at least 18 years of age and followed-up for at least 6 months were included. Patients were diagnosed as asthmatics when having typical clinical feature and improving with bronchodilator and/or inhaled steroid treatments. We dichotomized our patients into two groups based on reversibility. Patients were labeled to have reversible airflow limitation when they had shown an increase in the FEV1 results by 12% and 200 mL spontaneously or after using a bronchodilator. Patients who did not meet these criteria were labeled to be without reversible airflow limitation. Moreover, Two PFT results were collected, a baseline and a follow-up which are at least 12 months apart to assess changes in the variables.
Patients who are smokers, diagnosed with lung diseases that affect respiratory function, chest wall deformities, neuromuscular disorders affecting the chest wall, pulmonary congestion, cardiovascular diseases, and significant anemia (Hb<10mg/dL) were all excluded. Finally, ex-smokers who quit smoking in the past 10 years on the baseline PFT were excluded.
Study Design and Evaluation
Retrospective cohort study in which subjects were included using a consecutive sampling technique. Collected variables included demographic data such as age, gender and Body Mass Index (BMI). Moreover, baseline pre- and post-bronchodilator results of the following values, FEV1, FVC, FEV1/FVC ratio, percent change in FEV1, and percent change in FVC were collected and compared to follow up PFT which is at least 12 months apart. Following a standardized procedure, bronchodilator used is salbutamol (200mg). Other collected data include the presence of cardinal symptoms of asthma (cough, wheeze, and dyspnea), the frequency of exacerbations per year, defined by the use of oral or inhaled corticosteroids due to worsening symptoms of asthma, the frequency of emergency department visits due to asthma or asthma symptoms, and the treatment regimen prescribed.
Statistical Analysis
All analyses were performed using SPSS. The proportion and means for continuous variables were measured to describe subjects' characteristics. Outcomes were compared between subjects with and without reversible airflow limitation using chi-square test, Student's t-test and logistic regression analysis. Statistical significance will be determined using a 95% confidence interval and a P-value of 0.05. Results are expressed.
Ethical Considerations
Ethical approval was obtained from King Abdullah International Medical Research Center's (KAIMRC) ethical committee. Confidentiality was ensured during data collection and processing.
Declaration of Interest
The authors declare no conflict of interest. Moreover, the authors report no conflict of interest concerning the methods or materials used in this study or the findings specified in this paper.
Results
154 subjects were included, of which 42 had reversibility and 112 did not. The mean age for asthmatics with and without reversibility were 48.57 and 52.2 respectively. Other baseline demographic and PFT characteristics are shown in (Table 1).
| Characteristics | Reversibility (n=42) | No Reversibility (n=112) |
|---|---|---|
| Mean age (years) | 48.57 [43.86-53.28] | 52.27 [49.33-55.2] |
| Male (%) | 12 (28.57%) [15.72% - 44.58%] | 14 (12.50%) [7.01% -20.01%] |
| Body Mass Index (kg/m2) | 31.71 [29.71-33.66] | 32.35 [31.10-33.60] |
| Diabetes Mellitus | 16 (38.10%) | 38 (33.93%) |
| Hypertension | 16 (38.10%) | 34 (30.36) |
| Renal Disease | 2 (4.76%) | 7 (6.25%) |
| Baseline Pre FVC | 2.54 [2.29-2.79] | 2.38 [2.24-2.53] |
| Baseline Post FVC | 2.79 [2.54-3.04] | 2.40 [2.25-2.54] |
| Baseline Pre FEV1 | 1.78 [1.59-1.97] | 1.90 [1.77-2.03] |
| Baseline Post FEV1 | 2.13 [1.91-2.34] | 1.96 [1.83-2.09] |
| Baseline Pre FEV1% | 62.90% [58.48% - 67.33%] | 75.17% [71.16% - 78.72%] |
| Baseline Post FEV1% | 75.71% [71.02% - 80.41%] | 76.72% [73.04% - 80.41%] |
| FEV1/FVC ratio (Pre) | 0.7 | 0.79 |
| Baseline Pre FVC | 2.54 [2.29-2.79] | 2.38 [2.24-2.53] |
Table 1: Baseline characteristics of subjects (demographic and PFT)
The presenting symptoms and treatment regimens among asthmatics with and without reversibility are illustrated in Table 2 and Table 3.
| Symptoms | Reversibility (n=42) | No Reversibility (n=112) |
|---|---|---|
| Cough | 24 (57.14%) [0.42-0.73] | 66 (58.93%) [0.54-0.73] |
| SOB | 23 (54.76%) [0.39-0.71] | 54 (48.21%) [0.42-0.62] |
| Wheeze | 21 (50.00%) [0.35-0.67] | 37 (33.04%) [0.26-0.45] |
Table 2: Presenting symptoms of asthmatics with and without reversibility.
| Medications | Reversibility (n=42) | No Reversibility (n=112) |
|---|---|---|
| SABA | 33 (78.57%) | 90 (80.36%) |
| LABA | 30 (71.43%) | 77 (68.75%) |
| LAMA | 11 (26.19) | 16 (14.29) |
| ICS | 39 (92.86%) | 104 (67.53%) |
| Low Dose ICS | 9 (21.43%) | 34 (30.36%) |
| Moderate Dose ICS | 21 (50.00%) | 40 (35.71%) |
| High Dose ICS | 9 (21.43%) | 30 (26.79%) |
Table 3: Treatment regimens used among asthmatics with and without reversibility.
Patients with reversibility had more significant worsening of FEV1 than those without reversibility (20 ± 17.69 mL versus 0.11 ± 8.13 mL, p= 0.02) during follow-up (Figure 1).
Patients with reversible airflow limitation experienced more frequent exacerbations than patients without reversibility (74% versus 36%. p= 0.23), however the difference did not reach statistical significance (Figure 2).
Discussion
Our study findings indicate that asthmatics with reversibility have more worsening of their lung function during follow up, as compared to asthmatics without reversibility. A possible explanation is that these dynamic changes may indicate more airway inflammation that predispose to airway remodeling. In contrast to our findings, however, Boskabady et al. reported a significant correlation between reversibility of FEV1 (defined as an increase in FEV1 10 minutes post-bronchodilator) and improvement in FEV1 after a three months course of treatment (12). Furthermore, Boulet LP et al. found mean baseline FEV1 for those without reversibility to be significantly lower than that of patients with reversibility (13).
Our study also demonstrated no difference in the rates of exacerbation between asthmatics with and without reversibility. On the contrary, Denlinger et al. found that there is a linear relationship between the degree of reversibility and risk of exacerbations only in populations that have one or two exacerbations per year (14). It has been hypothesized that patients with Exacerbation prone asthma (EPA), defined as three or more exacerbations per year, have a distinguished phenotype in comparison to other subjects with similar FEV results because they could possibly demonstrate increased capacity of airway closure due to remodeling such as hypertrophy of smooth muscle and thickening of the basement membrane (14). Furthermore, Matsunaga K et al. found that the exacerbation rate was significantly correlated with the decline in FEV1 (15).
We also did not find any relation between reversibility and asthma related ER-visits. This is in contrast to studies that have been conducted on children and adolescents which demonstrated that the greater the degree of reversibility the higher the likelihood of having asthma-related ER visits and the highest risk for developing exacerbations in the future (16). Another study assessing dose-responsiveness to bronchodilation among children and adolescents found that those with poor bronchodilator response had a 2-fold increase in ER visits as well as a 2-fold increased odds of a subsequent ER visit compared to those who had better responsiveness to bronchodilators (17).
Limitations of the study include the small sample size due to the fact that many patients did not have a follow-up PFT at our center. Moreover, it is only a single-center study and retrospective in design.
Conclusion
Asthmatics with reversibility had a greater decline of FEV1 during follow-up compared to those without reversibility. However, the presence of reversibility did not influence the risk of exacerbation in our population.
Declaration of Interest
The authors declare no conflict of interest. Moreover, the authors report no conflict of interest concerning the methods or materials used in this study or the findings specified in this paper.
Acknowledgment
We would like to acknowledge the research unit at King Saud bin Abdul-Aziz University for Health Sciences College of Medicine, Jeddah (KSAUHS, COM-J) for their support. Also we would like to acknowledge the medical records department at King Abdul-Aziz Medical City (KAMC) for their cooperation during the study period.
References
- GINA-2020-report_20_06_04-1-wms.pdf [Internet]. [cited 2020 Aug 30]. Available from:https://ginasthma.org/wp-content/uploads/2020/06/GINA-2020-report_20_06_04-1-wms.pdf
- Expert Panel Report 3 (2017) Guidelines for the Diagnosis and Management of Asthma.440.
- Overview | Asthma: diagnosis, monitoring and chronic asthma management | Guidance | NICE[Internet].NICE. Available from: https://www.nice.org.uk/guidance/ng80
- Smith HR, Iroin CG, Cherniack RM (1992) The Utility of Spirometry in the Diagnosis of Reversible Airways Obstruction. Chest. 101:1577â??81.
- Asthma [Internet]. [cited 2020 Aug 30]. Available from: https://www.who.int/en/news-room/fact-sheets/detail/asthma
- Fahy JV (2001) Oâ??Byrne PM. â??Reactive Airways Diseaseâ?: A Lazy Term of Uncertain Meaning That Should Be Abandoned. Am J Respir Crit Care Med. 163: 822â??823.
- Pratter MR, Hingston DM, Irwin RS (1983) Diagnosis of Bronchial Asthma by Clinical Evaluation. Chest.84:42â??7.
- Asthmaâ??s effect on the nation. [Internet]. Centers for Disease Control and Prevention. 2020 [cited 2020 Aug 30]. Available from: https://www.cdc.gov/asthma/asthmadata.htm
- Health Days 2018 - World Asthma Day [Internet]. [cited 2020 Aug 30]. Available from: https://www.moh.gov.sa/en/HealthAwareness/healthDay/2018/Pages/HealthDay-2018-05-02.aspx
- Moradi-Lakeh M, El Bcheraoui C, Daoud F, Tuffaha M, Kravitz H, Al Saeedi M, et al. Prevalence of asthma in Saudi adults: findings from a national household survey, 2013. BMC Pulm Med. 2015 Dec;15:77.
- Hekking P-PW, Bel EH (2014) Developing and Emerging Clinical Asthma Phenotypes. J Allergy Clin Immunol Pract.2: 671â??680.
- Boskabady MH, Fasihfar M, Maemoori G (2003) Correlation between symptom score, wheeze, reversibility of pulmonary function tests and treatment response in asthma. Iran J Allergy Asthma Immunol. 2:61â??7.
- Boulet L-P, Turcotte H, Turcot O, Chakir J. Airway inflammation in asthma with incomplete reversibility of airflow obstruction. Respir Med. 2003 Jun;97(6):739â??44.
- Denlinger LC, Phillips BR, Ramratnam S, Ross K, Bhakta NR, Cardet JC, et al. Inflammatory and Comorbid Features of Patients with Severe Asthma and Frequent Exacerbations. Am J Respir Crit Care Med. 2017 Feb;195(3):302â??13.
- Matsunaga K, Hirano T, Oka A, Tanaka A, Kanai K, et al. (2015) Progression of Irreversible Airflow Limitation in Asthma: Correlation with Severe Exacerbations. J Allergy Clin Immunol Pract. 3:759-764.e1.
- Howrylak JA, Fuhlbrigge AL, Strunk RC, Zeiger RS, Weiss ST, (2014) Raby BA, et al. Classification of childhood asthma phenotypes and long-term clinical responses to inhaled anti-inflammatory medications. J Allergy Clin Immunol. 133:1289â??300, 1300.e1-12.
- Grunwell JR, Nguyen KM, Bruce AC, Fitzpatrick AM, et al. (2020) Bronchodilator Dose Responsiveness in Children and Adolescents: Clinical Features and Association with Future Asthma Exacerbations. J Allergy Clin Immunol Pract. 8: 953â??64.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences