Treatment of Calciphylaxis Induced Lower Extremity Ulcers using Sodium Thiosulfate
1Research Scholar, the Toronto Institute of Plastic Surgery, Toronto, Canada
2Department of Surgery, University of Toronto and Consultant Plastic Surgeon, The Scarborough Hospital and the Toronto Institute of Plastic Surgery, Toronto, Canada
- *Corresponding Author:
- Mohammed M Elahi
Department of Surgery, University of Toronto and Consultant Plastic Surgeon, The Scarborough Hospital and the Toronto Institute of Plastic Surgery, Toronto, Canada
E-mail: mmelahi93@hotmail.com
Received date: September 04, 2018; Accepted date: September 21, 2018; Published date: September 27, 2018
Citation: Waheed AS, Khan A, Elahi H, Elahi MM (2018) Treatment of Calciphylaxis Induced Lower Extremity Ulcers using Sodium Thiosulfate. Int J Case Rep Vol 2:10
Copyright:© 2018 Waheed AS, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Calciphylaxis is a rare complication often seen in patients with End Stage Renal Disease (ESRD). We report a case of a female patient with chronic kidney disease who developed calciphylaxis with secondary hyperparathyroidism. The patient failed standard medical treatment and did not want to proceed with surgery. Sodium Thiosulfate (STS) was used to treat bilateral lower extremity ulcers on a regimen of three times per week over 9 weeks. The ulcers improved significantly and were completely healed at the end of the treatment cycle. There has been no recurrence of ulcers in the past 18 months since treatment. We present this case to highlight the importance of STS treatment for calciphylaxis induced lower extremity ulcers which may prevent the need to proceed with more invasive techniques such as surgery, wound debridements and skin grafting or flaps.
Keywords
Calciphylaxis; Ulcer; Skin grafting; Tumoral calcinosis
Introduction
Calciphylaxis, also known as calcific uremic arteriopathy, is a rare and life threatening condition which is classified as a tumoral calcinosis [1-6]. It is caused by calcification of micro vessels in the dermis and subcutaneous adipose tissue [1-6]. Calciphylaxis has a high morbidity rate from 46% to 80%, and an average of 50% in patients without uremia [2,4,7]. This disease is more susceptible in white females who are obese and suffer from End-Stage Renal Disease (ESRD). However, it may still occur in patients with normal renal functioning or earlier stages of chronic kidney disease [3,4,6]. This condition is characterized by painful skin lesions due to ischemia, which may lead to ulceration and necrosis, and is similar in uremic and non-uremic patients [3,4,6]. Treatment options include Hyper-Baric Oxygen Treatment (HBOT) and maggot therapy followed by oral pentoxyfilin [8,9]. The mainstay of treatment for these ulcers, however, is surgical debridement and soft tissue coverage with skin grafts and/or flaps which is quite invasive and associated with significant morbidity and even mortality. Recent reports, however, have highlighted the use of sodium Thiosulfate (STS) injections to effectively manage this condition as a non-invasive, non-operative option [8,9].
Case Report
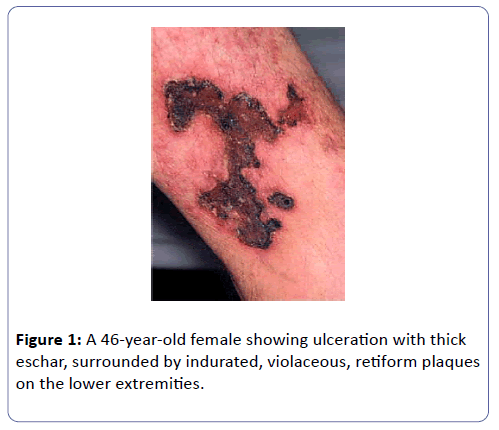
We present the case of a 46-year-old female who developed severe bilateral lower extremity ulcers. She was obese with a Body Mass Index (BMI) of 35, blood pressure of 90/36 and a pulse of 90 with regular heart beats. The patient suffered from small vessel vasculitis involving Central Nervous System (CNS) vasculitis and renal arteritis which was treated using drug therapy. She was diagnosed with ESRD which was treated by the creation of a left radio cephalic arteriovenous fistula for dialysis. She was also diagnosed with calciphylaxis and suffered from wounds on her bilateral thighs and legs (Figure 1).
Initially HBOT was administered but no significant improvement was documented. The necrotic and devitalized tissue was debrided with plans to proceed with surgical reconstruction. Literature search suggested that STS was a viable option to consider as the patient was reluctant to undergo surgery, especially given her multiple co-morbidities. Sodium Thiosulfate (STS) was administered, three times per week over a 9 weeks period after which no complications were noticed and the bilateral thighs and leg ulcers healed over. No further treatment has been required.
Discussion
Calciphylaxis is a rare condition which typically develops in patients with improper kidney functioning as a result of ESRD and is experiencing the symptoms of hyperparathyroidism [3,5]. The parathyroid gland maintains calcium-phosphorous homeostasis, so an irregularity would cause an imbalance in calcium and phosphate levels [10]. Calciphylaxis usually occurs in patients with improper calcium metabolism, which may lead to the formation of blood clots in micro vessels [7]. This buildup of calcium may lead to thrombosis, endovascular fibrosis and mural proliferation [2,7]. While the pathogenesis of calciphylaxis is poorly understood, it is theorized to be a two-stage process. The first stage involves vascular injury in the form of mural calcification, intimal hyperplasia, and endovascular fibrosis. This vessel damage sensitizes the supplied tissue areas to ischemia. In the second stage, additional vascular damage is triggered by clinical events, such as local trauma, hypotension, or thrombosis and leads to the development of an ischemic infarct, dystrophic calcification, or ulceration. Tissues and skin cells do not receive sufficient nutrients or oxygen which may lead to painful necrotic skin ulcers [7].
While there are numerous known ways to care for a patient suffering from calciphylaxis such as surgical wound treatment or managing factors that delay healing, managing the condition with STS injections is an effective and non-invasive treatment [1,2]. STS has a long history of medical use [11]. It is a vasodilator and an antioxidant [2-4]. Standard treatment of calciphylaxis using STS consists of 12.5-25 g intravenous doses administered thrice a week for 2 months [2]. Continuous administration of STS is necessary as 20% to 50% of STS is excreted before it reacts with calcium [7]. STS decreases the likelihood of calcium precipitate formation by isolating calcium ions from phosphate ions [1,2,5,7]. Highly soluble calcium thiosulfate complexes are formed, rather than less soluble calcium phosphate compounds [1,2,5,7]. To our knowledge, the first study to review the use of STS to treat calciphylaxis was by Peng et al. [12] which showed promising results. The study included 358 patients from which 70% responded successfully to STS treatment while 37.6% died despite administration of STS [12]. Some complications that arise from STS treatment are pain during administration and induced metabolic acidosis [7].
At present, there is no standard treatment of calciphylaxis due to limited clinical studies and cases. Treatment for calciphylaxis patients requires a multidisciplinary approach. Intravenous sodium thiosulfate and removing potential triggers are the main medical treatment for calciphylaxis. The treatment for calciphylaxis for our patient was commenced after the failure of HBOT. Significant improvement was noted after the patient was treated using STS by week 4, followed by complete resolution by week 9. There were no major complications during her treatment and the lesions or ulcers have not recurred. Her bilateral thighs and legs have completely healed on STS injection treatment without the need for adjuvant wound care or dressings. We believe that STS treatment is a viable treatment option in patients suffering from lower extremity ulcers from calciphylaxis.
References
- Goossens J, Courbebaisse M, Caudron E, Bahans C, Vacquerie V, et al. (2017) Efficacy of intralesional sodium thiosulfate injections for disabling tumoral calcinosis: Two cases. Semin Arthritis Rheum 47: 451-455.
- Isoherranen K, Bouchard L, Kluger N (2017) Benefits of intralesional injections of sodium thiosulfate in the treatment of calciphylaxis. Int Wound J 14: 955-959.
- Nigwekar SU, Thadhani R, Brandenburg VM (2018) Calciphylaxis. N Engl J Med 378: 1704-1714.
- Ng AT, Peng DH (2011) Calciphylaxis. Dermatol Ther 24: 256-262.
- Smith VM, Oliphant T, Shareef M, Merchant W, Wilkinson SM (2012) Calciphylaxis with normal renal function: treated with intravenous sodium thiosulfate. Clin Exp Dermatol 37: 874-878.
- Ahmed S, O'Neill KD, Hood AF, Evan AP, Moe SM (2001) Calciphylaxis is associated with hyperphosphatemia and increased osteopontin expression by vascular smooth muscle cells. Am J Kidney Dis 37: 1267-1276.
- Schlieper G, Brandenburg V, Ketteler M, Floege J (2009) Sodium thiosulfate in the treatment of calcific uremic arteriolopathy. Nat Rev Nephrol 5: 539-543.
- Podymow T, Wherrett C, Burns KD (2001) Hyperbaric oxygen in the treatment of calciphylaxis: a case series. Nephrol Dial Transplant 16: 2176-2180.
- Tittelbach J, Graefe T, Wollina U (2001) Painful ulcers in calciphylaxis - combined treatment with maggot therapy and oral pentoxyfillin. J Dermatolog Treat 12: 211-214.
- Mackenzie-Feder J, Sirrs S, Anderson D, Sharif J, Khan A (2011) Primary hyperparathyroidism: an overview. Int J Endocrinol 2011: 1-8.
- Asplin JR, Donahue SE, Lindeman C, Michalenka A, Strutz KL, et al. (2009) Thiosulfate reduces calcium phosphate nephrolithiasis. J Am Soc Nephrol 20: 1246-1253.
- Peng T, Zhuo L, Wang Y, Jun M, Li G, et al. (2017) A systematic review of sodium thiosulfate in treating calciphylaxis in chronic kidney disease patients. Nephrol 23: 669-675.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences