ISSN : ISSN: 2576-1455
Journal of Heart and Cardiovascular Research
The Implementation and Cost-Benefit Analysis of a Tertiary Hospital General Rapid Access Cardiology Clinic
Liam Marsden Back*, Praveen Indraratna, Virag Kushwaha
Department of Cardiology, The University of New South Wales, Prince of Wales Hospital, Randwick, Australia
- *Corresponding Author:
- Liam Marsden Back
Department of Cardiology,
The University of New South Wales,
Prince of Wales Hospital, Randwick,
Australia,
E-mail: liammarsdenback@gmail.com
Received date: July 05, 2022, Manuscript No. IPJHCR-22-7188; Editor assigned date: July 07, 2022, PreQC No. IPJHCR-22-7188 (PQ); Reviewed date: July 08, 2022, QC No. IPJHCR-22-7188; Revised date: July 28, 2022, Manuscript No. IPJHCR-22-7188 (R); Published date: Aug 05, 2022, DOI: 10.36648/ipjhcr.6.4.21
Citation: Back LM, Indraratna P, Kushwaha V ( 2022) The Implementation and Cost-Benefit Analysis of a Tertiary Hospital General Rapi d Access Cardiology Clinic. J Heart Cardiovasc Res Vol.6 No.4:21.
Abstract
Background
The Prince of Wales Hospital Rapid Access Cardiology Clinic (RACC) was established in August 2018 in an effort to defer all lower risk cardiology admissions from the Emergency Department (ED) to the outpatient setting. Where similar clinics have limited their focus to chest pain presentations, the scope of the RACC encompassed all general cardiology presentations. Our objective was to evaluate the utilisation, patient profile, clinic outcomes and cost-benefit over the first 12 months of the RACC.
Methods
Details of all patient encounters to the RACC were prospectively collected between August 2018 and July 2019. This included patient demographics, clinical presentation, clinic investigation results and further management initiated from the RACC appointment. A sum of matched Diagnosis-Related Grouping (DRG) coding figures for each individual patient encounter was collated and provided as a conservative cost-savings estimate.
Results
107 patients were reviewed in the RACC. The average age of patients was 52 +/- 1.6 years, 60% of whom were male. The majority of patients (>90%) were reviewed within 10 days of their ED presentation, with a median of 3 days. 99 patients (92.5%) were defined as appropriate referrals to the RACC. The major indication for review was chest pain with 65 patients (61%). 95 of 107 patient encounters (88%) had a resting Transthoracic Echocardiogram (TTE) or exercise stress echocardiogram during review. 53 of 59 (90%) of ESTs were negative for myocardial ischaemia. A number of subsequent specialty cardiology investigations were arranged by the RACC. Conservatively, an estimated total cost saving of $87,857 was derived from the RACC in the 12- month period following its implementation.
Conclusion
The establishment of the RACC provided an efficient and economically beneficial alternative pathway to inpatient investigation for a subset of lower-risk general cardiology presentations, not only chest pain.
The known
Rapid access cardiology clinics provide an efficient, safe, and satisfactory alternative pathway to inpatient investigation of low-risk chest pain from the emergency department.
The New
Extending a rapid access cardiology clinic to service a broader spectrum of lower risk cardiac emergency department presentations appears a feasible, efficient and financially beneficial model of care.
The Implications
Reviewing a subset of lower-risk cardiology patients in a prompt outpatient service appears to impact positively on a hospital budget and promote intangible benefits of increased bed availability for elective procedures, complex patients, and to improve patient flow.
Introduction
Cardiology presentations remain one of the most common reasons for an individual to attend an Australian Emergency Department (ED), and subsequent admissions continue to place a high burden on inpatient services. Six of the twenty most common ED principle diagnoses for patients admitted to Australian hospitals in 2017-18 were cardiac (pain in throat and chest, syncope and collapse, angina pectoris, heart failure, atrial fibrillation and flutter, and acute myocardial infarction). This accounted for 12% (304 443 patients) of all Australian hospital admissions during this period.
Chest pain remains a large contributor to this ED population, and although a high proportion of these patients are admitted to hospital, recent evidence has demonstrated only a small number (11%) are diagnosed with acute coronary syndrome. 1Growing data continues to reinforce a low 30-day event rate in chest pain patients categorised into low and intermediate risk, with 0% and 1.8% respectively.2 This contrasts significantly from those recognised as high-risk chest pain patients with a 30-day event rate of approximately 23%.2 This suggests that a number of these admissions may be avoidable and suitable for an outpatient investigation strategy.
A ‘Rapid Access Clinic’ has become an increasingly utilised tool, both internationally and in Australia, for providing access to timely specialist investigation and management for lower risk patients without necessitating a hospital admission.3-8 Within the cardiology practice, these clinics have predominantly been hospital based, consultant cardiologist-led outpatient clinics providing early access for assessment, investigation and management of chest pain. This model has been adopted widely in the UK as the preferred pathway for assessment of suspected angina pectoris.9 A recent review from published cardiology clinic data, predominantly UK based, has demonstrated that early assessment of chest pain in low-intermediate risk patients is safe, cost effective, reduces hospital admissions, and is a satisfactory pathway for both referring doctors and patients.10 Little data exists on the utility of this model extending beyond chest pain presentations to include other high-volume cardiology presentations to the ED including atrial fibrillation and flutter, syncope and heart failure.
With an increasing demand for inpatient beds in the cardiology service at Prince of Wales Hospital, a Rapid Access Cardiology Clinic (RACC) was established in August 2018 in an effort to defer all low to intermediate risk cardiology admissions, not only chest pain, from the ED to the outpatient setting. Patients referred to the RACC were reviewed by a cardiology registrar with direct consultant supervision, had an Electrocardiograph (ECG) performed and were able to proceed directly to Transthoracic Echocardiogram (TTE) or exercise stress echocardiogram in the same appointment if clinically indicated.
Recearch Ais
The aim of this study was to describe the first year of implementation of the RACC and document its utility, patient profile, clinic outcomes and economic benefit.
Methodological Approach
Approval for this prospective audit was obtained from our local district ethics committee. All patient data was anonymised and stored on a single computer located within hospital grounds in a password protected database, accessible only by the two audit investigators. Patient reviews in the RACC were identified on our appointment database and prospectively detailed for the 12-month period from August 2018 to July 2019.
Data was cross-checked against the original referral letters, the finalised clinic letter authored by the consulting doctor, and the patients’ electronic medical records where recent records were available. Patient demographic data was manually collected and outlined patient age, gender, cardiovascular risk factors and number of prescription medications at the time of clinic review. Each patient’s primary presenting symptom was recorded and classified as chest pain, dyspnoea (undifferentiated), syncope, palpitations, atrial fibrillation/ flutter, or supraventricular tachycardia. Where a single, readily identifiable cardiac symptom was not able to be identified, these patients were classified as ‘other’ for the purpose of this audit. To obtain the data for time until clinic review, the number of days between the receipt of the original referral and the RACC appointment date was recorded. Outcome data was recorded including investigations ordered through the RACC, and results of these investigations if occurring as part of their clinic assessment, for example, an EST. Further outcome data documented included medication changes as a result of the clinic appointment, excluding beta blockade prescribed for CT coronary angiography, and follow up arrangements necessary post clinic assessment, defined as primary care, outpatient cardiology follow up, or direct admission for inpatient management.
An assessment of appropriateness of referral was made by the investigators on review of each patient encounter. A patient was deemed appropriate if they had stable, low to intermediate risk cardiac symptoms requiring further investigation, and who would have otherwise been admitted to our hospital based on current department standards. Requirements to be classified as a low to intermediate risk patient were negative serial troponins, no dynamic ischaemic ECG changes, no oxygen requirement and no haemodynamic instability. Arrhythmia presentations were required to have a heart rate of less than 110 prior to discharge. An appropriate low to intermediate risk syncope presentation was decided on a case by case basis, following assessment from the emergency physician and discussion with the consulting cardiologist. A referral was deemed inappropriate based on pre-specified domains; if a patient reviewed had unstable symptoms or had not had adequate exclusion of other relevant acute pathology in the ED (i.e pulmonary emboli), if the referral was received greater than seven days from a patients’ index ED presentation, or if a patient had already arranged alternative outpatient cardiology follow up within thirty days of their index presentation. All patients categorised as inappropriate referrals were reviewed independently by both audit investigators.
An economic estimate of costs deferred by the RACC was made with assistance from hospital executive and administrative staff. To complete this analysis, a presumption was made that each patient encounter represented a single day inpatient admission to a general cardiology (telemetry) bed. Patient encounters were subsequently stratified by their primary presenting symptom. This data was provided to hospital coders who were able to match each presenting symptom to its corresponding NSW health Diagnosis-Related Grouping (DRG) coding value. The sum total of these individual encounters was calculated and included as our conservative savings estimate. No additional staffing was required to service this clinic.
Results
107 patient encounters were recorded in the RACC between August 2018 and July 2019.
60% of patients reviewed in the RACC were male. The age range of patients was broad at 20 to 87 years, with a median age of 52, and a mean age of 52 +/- 1.6 years. Only 4% of patients were aged 80 and older.
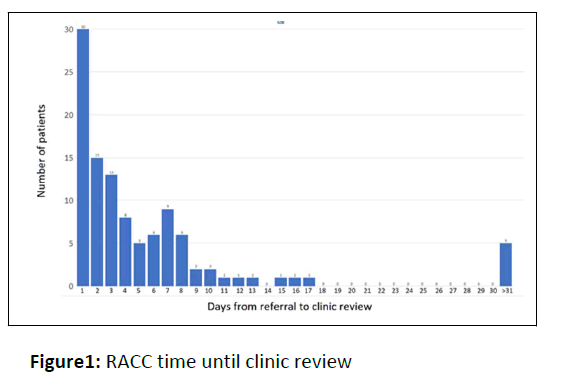
Time until clinic review showed a median of 3 days with a mean of 6.2 +/- 1.1 days. This mean was influenced by a small number of outliers reviewed greater than 3 weeks from original referral (See Figure 1). 75% of patients were reviewed within 1 week of referral, with the majority of patients (>90%) reviewed within 10 days of their index ED presentation. 99 patients (92.5%) were defined as appropriate referrals to the RACC as specified by the investigators predetermined criteria.
Time from receipt of original referral to review in the Rapid Access Cardiology Clinic (RACC) for all 107 patient encounters. The median time to review was 3 days. The mean time for review of 6.2 +/- 1.1 days was influenced significantly by 5 outliers of greater than 31 days. 30 patients (28%) were reviewed within one day of receipt of their referral.
A significant proportion of patients (63%) reviewed had one or more conventional cardiovascular risk factor including smoking (21%), hypertension (48%), dyslipidaemia (48%) and diabetes mellitus (22%). 72% of patients reviewed were on at least one prescription medication, with 18% of patients being on 5 or more, further suggesting a degree of medical complexity in those patients reviewed.
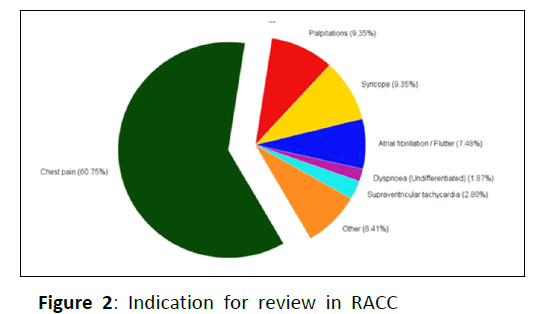
The major indication for review in the RACC was chest pain with 61% (See Figure 2). The other significant indications for referral included palpitations (9%), syncope (9%), atrial fibrillation/flutter (7%), supraventricular tachycardia (3%), undifferentiated dyspnoea (2%) and other (8%).
Proportional breakdown of primary indication for referral and review in the Rapid Access Cardiology Clinic (RACC). The majority of referrals received were for an assessment of chest pain with 65 patients. The remainder of referrals were comprised primarily of arrhythmia, syncope and undifferentiated dyspnea. For the purpose of this study, patients in whom a single, readily identifiable primary complaint was not able to be identified, or those presenting with non-cardiac symptomatology, were categorized as ‘other’.
The predominant investigations facilitated during the RACC appointment were ECG, TTE and EST. 95 of 107 patient encounters (88%) had a TTE or EST. 59 ESTs (56% of referrals) were performed during this 12-month period. 90% of ESTs were negative, with 8.3% equivocal and 1.7% positive.
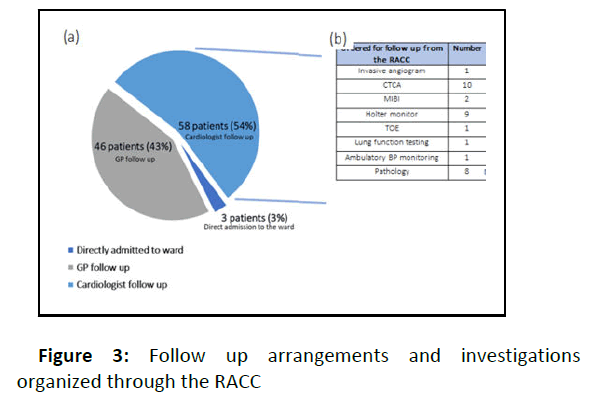
Following review in the RACC, a number of subsequent specialty cardiology investigations were arranged including 2 invasive coronary angiograms, 10 CT coronary angiograms, 2 sestamibi myocardial perfusion scans, 8 Holter monitors and 1 transoesophageal echocardiogram (See Figure 3). 14% of patients were prescribed at least one new prescription medication as a result of the clinic review. This did not include patient’s prescribed B blocker in anticipation of a CT coronary angiogram.
Proportional breakdown of patient disposition following review in the Rapid Access Cardiology Clinic (RACC). 3 patients (3%) were directly admitted to the ward for inpatient management following their clinic assessment. The remainder of patients had follow-up arranged either with their primary care physician (43%), or an appointed cardiologist (54%). (b) Subsequent outpatient specialty investigations organised through the RACC for follow up with either the patients’ primary care physician or appointed cardiologist. The primary cardiac investigations ordered post clinic assessment were CTCA and 24- hour Holter monitoring. Abbreviations: CTCA – Computed tomography coronary angiogram, MIBI – Sestamibi myocardial perfusion scan, TOE – transoesophageal echocardiogram.
53% of patients were referred for ongoing cardiology follow up after review in the RACC. 43% were discharged to their primary care physician without need for ongoing specialist cardiology follow up.Three patients (3%) were directly admitted to the ward following review; indications being inpatient management of pulmonary emboli, inpatient invasive coronary angiogram, and insertion of an implantable loop recorder.
An estimated total cost saving of $87,857 was derived from the RACC in the 12-month period following its implementation. There are likely further increased organisational benefits from the RACC including increasing hospital capacity for more complex acute admissions, elective procedures, and improving patient flow.
Discussion
Results from the RACC demonstrate an efficient and potentially cost-saving alternative to the current inpatient model of care. Encouragingly, the majority of patients (92.5%) were defined as appropriate referrals to the clinic. Patients were generally young with a mean age of 52 +/- 1.6 years, with only a very small proportion greater than 80 years old (4%), and this must be considered when contemplating a wider application of this service.
Mean and median time until clinic appointment was appropriate, with the vast majority of patients (>90%) being reviewed within 10 days of their index ED presentation suggesting a highly efficient service. Our clinic compared favourably with other published Australia data, quoting median time to clinic appointment at 12 days for a rapid assessment clinic and 45 days for cardiology rooms.4 When compared with previously described data reporting a less than 2% event rate in low-intermediate risk chest pain patients in 30 days, this appears an acceptable time period to specialist review. The applicability of this time frame to non-chest pain presentations is unknown however, and must be applied with caution.
A significant proportion of patients (18%) reviewed in the RACC were on 5 or more prescription medications. Furthermore, 63% of patients had a least one or more conventional cardiovascular risk factor. This suggests a degree of patient complexity in those reviewed and supports a hypothesis that not only very-low risk presentations were being referred to the RACC, but also those with reasonable medical complexity and an intermediate degree of suspicion for cardiac disease.
The majority of patients reviewed in the RACC were chest pain presentations, a pattern consistent with other published data. The referrals of palpitations, atrial fibrillation/flutter and supraventricular tachycardias (comprising 19% of patients) suggests another potential cluster of low-risk cardiology presentations that may be able to be safely managed in an outpatient setting. Interestingly, no referrals for heart failure were received by the RACC in the 12-month period. This was likely influenced by the existence of a well-established community heart failure outreach service within our district.
93% of all chest pain referrals underwent EST with an overwhelming majority of those negative. Only 1 of 59 (1.7%) ESTs performed were positive which is reassuring that an appropriate patient population was being referred safely for delayed functional testing. Those with equivocal results were referred on further for sestamibi myocardial perfusion scanning, CT coronary angiography or invasive coronary angiography as appropriate.
Published data from other Australian rapid access cardiology clinics reports similar baseline patient demographics but a significantly higher proportion of positive exercise stress tests (8-16%).4,7 There are several reasons that this observation may be apparent, particularly the larger population of patients undergoing EST, in addition to the significantly longer implementation and observation periods used in their studies. With increased familiarity of the referral process, it could be suspected that a larger number of intermediate risk patients would be referred to the outpatient setting with the understanding that their investigations would be promptly organised.
Liitations Of The Study
This study has several limitations which need to be considered when interpreting its results. Patients referred to the RACC after hours were often requested to contact administrative staff on the next available business day to confirm their appointment details. An accurate record of patients who did not contact or attend the RACC following their index ED presentation was not collected. This raises the possibility of a significant population underrepresented in the defined results.
The majority of patients reviewed in the RACC were middle age male patients with relatively few comorbidities. For this population, it would appear a safe and efficient means of investigating for cardiac pathology in an outpatient setting. There may be difficultly in applying and utilising such clinics for an increasingly geriatric population with multiple comorbidities who present with cardiac symptoms, however, and this must be considered when establishing such a service.
While this data is suggestive of a significant financial benefit from the implementation of the RACC, estimating exact economic effect is challenging. A conservative cost-savings estimate of $87,857 was made on the supposition that all referrals to the RACC were appropriate and would have required only a single inpatient day admission. The presenting complaint of the patient was subsequently matched to NSW health DRG coding to provide an estimate for ‘bed cost’ for this proposed one day admission. No supplementary DRG codes were used in addition to that generated from a patient’s presenting symptom, which may have underestimated costs saved for our hospital.
There are obvious limitations to financial estimates based on this method, including inaccurate coding, underappreciation of patient complexity, and presumption that all clinic patients would have been admitted. Furthermore, although the implementation of the RACC required no additional staffing, patient volume was relatively small and a broader application would require consideration of this factor in financial savings estimates. Additionally, no correction was made for the use and decline in value of investigative tools such as transthoracic echocardiogram equipment and exercise stress hardware. Regardless of these limitations, however, these results provide the impression that an appropriately organised RACC will contribute positively to the hospital health budget. There are also several intangible benefits for hospital administration that are difficult to estimate financially, including improved patient flow and increased bed availability for elective procedures and complex patients.
Conclusion
The implementation of the RACC provided an efficient and economically beneficial alternative pathway to inpatient investigation for a subset of lower-risk general cardiology presentations, not only chest pain.
References
- Cullen L, Greenslade J, Merollini K, Graves N, Hammett CJ, et al. (2015) Cost and outcomes of assessing patients with chest pain in an Australian emergency department. Med J Aust 202: 427–432.
[Crossref], [Googlescholar], [Indexed]
- Cullen L, Greenslade JH, Hawkins T, Hammett C, O’Kane S, et al. (2017) Improved assessment of chest pain trial (IMPACT): assessing patients with possible acute coronary syndromes. Med J Aust 207: 195-200.
[Crossref], [Googlescholar], [Indexed]
- Black JA, Cheng K, Flood JA, Hamilton G, Parker S, et al. (2019) Evaluating the benefits of a rapid access chest pain clinic in Australia. Med J Aust 210: 321-325.
[Crossref], [Googlescholar], [Indexed]
- Klimis H, Khan ME, Thiaglingam A, Bartlett M, Altman M, et al. (2018) Rapid Access Cardiology (RAC) Services Within a Large Tertiary Referral Centre-First Year in Review. Heart Lung Circ 27: 1381-1387.
[Crossref], [Googlescholar], [Indexed]
- Lenderink T, Balkenstein EJ (2019) First time referral reasons, diagnoses and 10-year follow-up of patients seen at a Dutch fast lane outpatient cardiology clinic. Neth Heart J 27: 354-361.
[Crossref], [Googlescholar], [Indexed]
- Yu C, Sheriff J, Ng A, Brazete S, Gullick J, et al. (2018) A Rapid Access Chest Pain Clinic (RACPC): Initial Australian experience. Heart Lung Circ 27: 1376-1380.
[Crossref], [Googlescholar], [Indexed]
- Debney MT, Fox KF (2012) Rapid access cardiology – A nine year review. QJM 105: 231-234.
[Crossref], [Googlescholar], [Indexed]
- Rajpura A, Sethi S, Taylor M (2007) An evaluation of two Rapid Access Chest Pain Clinics in central Lancashire, UK. J Eval Clin Pract 13: 326-336.
[Crossref], [Googlescholar], [Indexed]
- Davie AP (2010) NICE guidance on the investigation of chest pain. Heart 96: p1859.
[Crossref], [Googlescholar], [Indexed]
- Klimi H, Thiagalingam A, Altman M, Atkins E, Figtree G, et al. (2017) A review of rapid access cardiology services – Can these reduce the burden of acute chest pain on Australian and New Zealand health services? Intern Med J 47: 986-991.
[Crossref], [Googlescholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences