Superior Gluteal and Inferior Gluteal Artery Pseudoaneurysms Following Blunt Traumatic Pelvic Ring Disruption
Hu DK1*, Watkins JR1, Mani US2, Slonim SM3,Amos JD1 and Dunn EL1
1Department of Surgery, Methodist Dallas Medical Center, Dallas, Texas, USA
2Department of Orthopedics, Methodist Dallas Medical Center, Dallas, Texas, USA
3Department of Radiology, Methodist Dallas Medical Center, Dallas, Texas, USA
- *Corresponding Author:
- Hu DK
Department of Surgery, Methodist Dallas
Medical Center, Dallas, Texas, USA
Tel: +1 214-947-8181
E-mail: David.Hu@bcm.edu
Received date: February 27, 2018; Accepted date: March 14, 2018; Published date: March 29, 2018
Citation: Hu DK, Watkins JR, Mani US, Slonim SM, Amos JD, et al. (2018) Superior Gluteal and Inferior Gluteal Artery Pseudoaneurysms Following Blunt Traumatic Pelvic Ring Disruption. J Emerg Trauma Care. Vol.3 No.1:2.
Abstract
We present a case of a previously healthy man arriving at our emergency department complaining of pelvic and lower extremity pain after being crushed by a fork lift at work. A computed tomography (CT) revealed significant pelvic ring disruption with 100% disassociation of the sacroiliac (SI) joint, along with a transverse posterior wall fracture pattern and displacement hip protrusion. The patient underwent staged open reduction and internal fixation of his injuries. Twenty two days after the initial injury, he developed hemodynamic instability, CT revealed active extravasation of contrast in the pelvis. Angiography subsequently revealed unique pseudoaneurysms of the superior and inferior gluteal arteries. Embolization of the pseudoaneurysms was complicated with subsequent gluteal muscle necrosis.
Keywords
Pseudoaneurysms; Traumatic; Pelvic; Blunt
Introduction
Pelvic trauma can be categorized into blunt and penetrating injury, of which blunt trauma is more common. Pelvic trauma has a high incidence of vascular injury, with hemorrhage as the highest cause of mortality in this patient group [1].
Pseudoaneurysm of the superior or inferior gluteal artery is uncommon and overwhelmingly related to penetrating trauma. There are few case reports of isolated gluteal artery pseudoaneurysm after blunt trauma. Pseudoaneurysms of the superior gluteal artery are more common than those of the inferior gluteal artery. A review of the literature shows only 10 cases of inferior gluteal artery pseudoaneurysms described in the last 30 years [2].
Even rarer are concomitant superior and inferior gluteal pseudoaneurysms, none of which have been discussed in the existing literature. The preferred treatment is trans-arterial embolization (TAE). Trans arterial embolization has been well established as an option for management of hemorrhage and vascular injury in pelvic trauma. However, pelvic TAE does include its own set of complications, including muscle, bladder, femoral head and skin necrosis and even paresis, impotence and surgical wound complications [3].
Unfortunately, gluteal muscle necrosis may be a significant and fatal complication of this procedure. Gluteal muscle necrosis can cause sepsis and disseminated intravascular coagulation [3]. High suspicion and early detection of complications related to TAE are vital.
We present a case of pseudoaneurysms of both the superior and inferior gluteal arteries after blunt trauma with subsequent gluteal necrosis after TAE.
Case Presentation
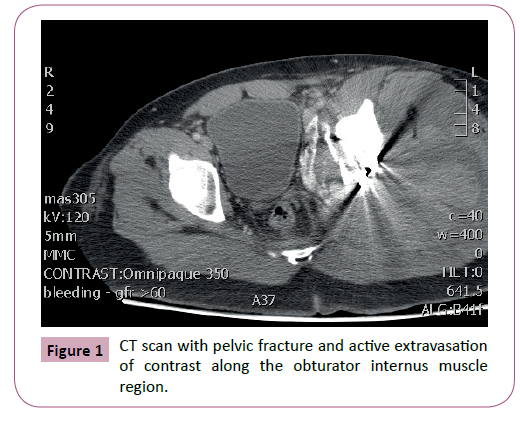
A 30-year-old man presented to our emergency department after sustaining a severe crush injury to the pelvis. The patient was hemodynamically normal and all laboratory values were within normal limits. The patient had a Glasgow Coma Scale of 15 and was neurovascularly intact in all extremities. Focused assessment with sonography (FAST) was negative for fluid and the patient was subsequently taken to CT for further evaluation (Figure 1).
Imaging revealed an acetabular fracture with significant protrusion and pelvic ring disruption. The patient had no intraperitoneal, intracranial, or spinal injuries. He was admitted to the Surgical Trauma Intensive Care Unit for close monitoring of his injuries. Orthopedic surgery consultation was obtained. Staged open reduction and internal fixation was undertaken without any intraoperative complication. The patient underwent three operations to stabilize his pelvic injuries over the course of two weeks.
He was subsequently transferred to the trauma surgery unit. The patient continued to have decreasing hemoglobin despite resuscitation efforts. Hemodynamic instability and continued failure of resuscitation efforts three weeks post-injury led to repeated computed tomography evaluation.
CT revealed active extravasation of contrast along the obturator internus muscle on the left, in addition to acute hematoma within the musculature of the pelvis.
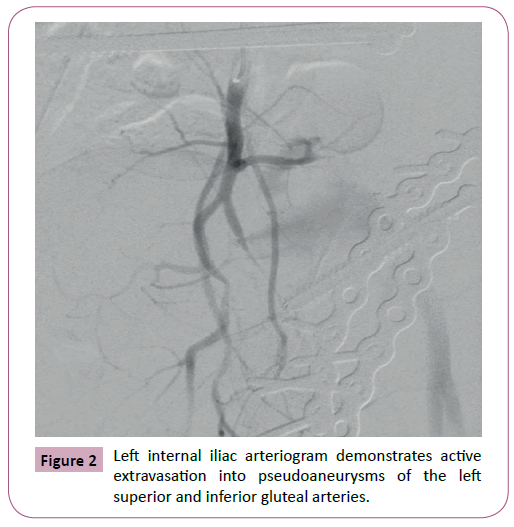
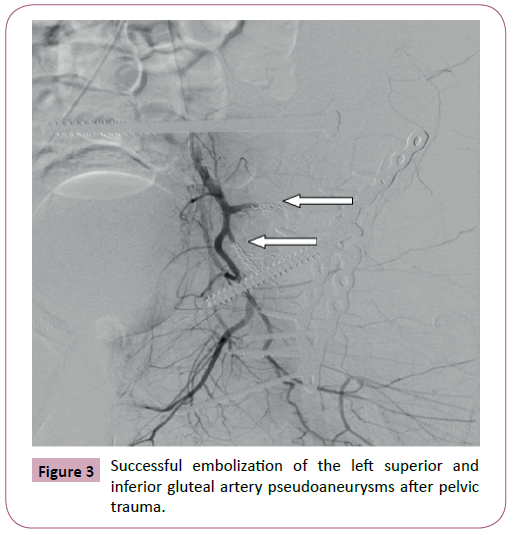
The patient was transferred to the interventional radiology suite where arteriography revealed active extravasation of contrast into pseudoaneurysms of the superior and inferior gluteal arteries, with adequate collateral flow to the buttocks (Figure 2). Coil embolization of the left gluteal arteries was performed (Figure 3).
The patient tolerated the procedure well initially and had no acute events or complications for the remainder of his hospital stay. There was no drainage and the orthopedic wound was healing appropriately, thus the patient was subsequently discharged to rehab post-embolization day 5. Follow up evaluation by the orthopedic surgeon1 week after discharge revealed wound dehiscence and wound infection. The patient also reported low grade fevers. Examination revealed full-thickness ulcerations over the incision as well as a bed of hematoma and smaller ulcerations in the form of eschar and wound dehiscence at the medial aspect of the hip. Wound care consultation was subsequently obtained. Initially the wound was treated conservatively with serial debridements, incision and drainage, and wound vac placement.
Subsequent wound care follow up revealed expanding ulceration and the new development of purulent drainage. At this time, the patient was admitted to the hospital for intravenous antibiotic therapy, surgical debridement, and extensive pelvic washout. Upon pelvic exploration it was noted that he had extensive necrosis of the gluteus maximus, gluteus medius and gluteus minimus, which required extensive muscle debridement and antibiotic bead placement along with aggressive, copious wound irrigation. The wound subsequently required four additional surgical debridements over the course of two weeks before formal closure was performed. The patient was subsequently discharged to rehab with an extended course of intravenous antibiotics and planned reconstructive surgery in the future.
Discussion
Vascular injury is common in pelvic fractures due to the close proximity of the vasculature in the pelvis and is a frequent cause of mortality in this group of patients [4,5]. Additionally, due to the large volume of potential space in the pelvis, hemodynamic instability can be seen in up to 20% of patients, with a reported mortality rate up to 40% [6]. Blunt traumatic pelvic injuries can lead to vascular injuries that include bleeding that is venous, osseous, or arterial. There can be complete or partial vessel transection, pseudoaneurysms, arteriovenous fistulas, dissection and thrombosis. Penetrating traumas are more likely to form pseudoaneurysms [1]. Moreover, traumatic pseudoaneurysms are at high risk for rupture and should be identified quickly and preferably treated endovascularly [7]. The recent advances in computed tomography technology, with the development of CT angiography, allow detailed evaluation of vascular trauma. Digital subtraction diagnostic angiography allows further evaluation of vascular injury and simultaneous endovascular treatment. Advances in endovascular techniques have improved management of patients with vascular injury. In order to have successful outcomes of these endovascular techniques, there must be a multidisciplinary approach in which both trauma surgeons and interventional radiologists collaborate to understand the indications and complications of embolization.
In our case, CT accurately identified the reason for the patient’s hemodynamic instability. However, active hemorrhage and vascular injuries may be subtle on CT. Computed tomography angiography or diagnostic angiography may be needed to identify these injuries. Therefore a high suspicion for and knowledge of the natural history of potential vascular injuries is required.
Nonselective embolization of a capillary bed is directly related to tissue ischemia. When choosing embolization, the choice of embolic agent is equally important, as this can be a good predictor of tissue ischemia [1]. Embolization can be performed with coils, gelfoam, vascular plugs, particles or a combination of these agents. Coils and vascular plugs are permanent embolization agents with which once you obtain proximal embolization, distal access is not possible. These agents are larger and induce occlusion by thrombosis distal to the device. Gelfoam induces occlusion by mechanical obstruction, but it is a temporary embolic agent. It eventually becomes absorbed by the body with recanalization in a few weeks. The small size of embolic particles increases the risk of nonselective distal capillary embolization, which may lead to ischemia. The chosen size of the embolic material should be large enough to prevent distal capillary occlusion but small enough to perform a selective embolization. Smaller the embolic agent, greater is the chance of tissue ischemia. In our case the interventional radiologists used embolization coils yet there were still complications of tissue ischemia.
Although complications of gluteal necrosis are more often seen in bilateral internal iliac artery embolization, unilateral embolization can also cause gluteal necrosis. Embolization can cause skin breakdown, poor wound healing, lower limb paresis, bladder necrosis, and rectal necrosis [1,8]. High clinical suspicion and early diagnosis of post-embolization complications can decrease mortality. Along with a high clinical suspicion, the trauma team should be cognizant of which arteries are occluded during the process of TAE. As in this case, our patient developed significant gluteal muscle necrosis complicated by wound infection and wound dehiscence. Despite these potential complications, when indicated transcatheter angiographic embolization can significantly reduce morbidity and mortality associated with traumatic pelvic ring disruption.
Conclusion
Dual superior and inferior gluteal pseudoaneurysms are a rare but important entity and are often related to penetrating trauma, but can be a sequela of blunt trauma as well. Trans arterial embolization is the treatment of choice for this disease process. Unfortunately this can result in gluteal necrosis with significant morbidity and mortality. High clinical suspicion and careful attention are advised after significant blunt pelvic trauma and subsequent TAE of the gluteal arteries. Early detection and close follow up will prevent significant morbidity and mortality.
References
- Wilkins LR, All J, Angle JF (2014) Transcatheter embolization for trauma of the pelvis. Endovascular Today 2014: 60-66.
- Agarwal M, Iannoudis PV, Syed AA, Hinsche AF, Matthews SJ, et al. (2003) Pseudoaneurysm of the inferior gluteal artery following polytrauma: diverse presentation of a dangerous complication: A report of two cases. J Orthop Trauma 17: 70-74.
- Matityahu A, Marmor M, Elson JK, Lieber C, Rogalski G, et al. (2013) Acute complications of patients with pelvic fractures after pelvic angiographic embolization. Clin Orthop Relat Res 471: 2906-2911.
- Chong K, DeCoster T, Osler T, Robinson B (1997) Pelvic fractures and mortality. Iowa Orthop J 17: 110-114.
- Salsamendi J, Quintana D, Kably I, Narayanan G (2013) Special considerations for embolization in trauma cases. Endovascular Today, 2013: 42-50.
- Fu C, Wang Y, Wu S, Chen R, Hsieh C, et al. (2012) Angioembolization provides benefits in patients with concomitant unstable pelvic fracture and unstable hemodynamics. Am J Emerg Med 30: 207-213.
- Bauer JR, Ray CE (2004) Transcatheter arterial embolization in the trauma patient: A review. Semin Intervent Radiol 21: 11-22.
- Suzuki T, Kataoka Y, Minehara H, Nakamura K, Uchino M, et al. (2008) Transcatheter arterial embolization for pelvic fractures may potentially cause a triad of sequela: Gluteal necrosis, rectal necrosis, and lower limb paresis. J Trauma 65: 1547-1550.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences