ISSN : 2576-3911
Integrative Journal of Global Health
Responses to Clinical Questions: Specialist-Based Medicine vs. Reasonable Clinic in Family Medicine
1Health Center Santa Maria de Benquerencia, Toledo, Spain
2Regional Health Service of Castilla la Mancha (SESCAM), Toledo, Spain
- *Corresponding Author:
- Jose Luis Turabian
Health Center Santa Maria de Benquerencia
Toledo, Spain
Tel: 34925154508
E-mail: jturabianf@hotmail.com
Received date: January 03, 2017; Accepted date: January 13, 2017; Published date: January 20, 2017
Citation: Turabian JL, Franco BP. Responses to Clinical Questions: Specialist-Based Medicine vs. Reasonable Clinic in Family Medicine. Integr J Glob Health. 2017, 1:1.
Abstract
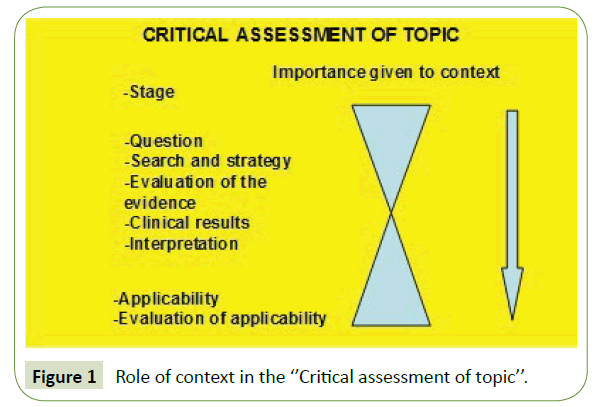
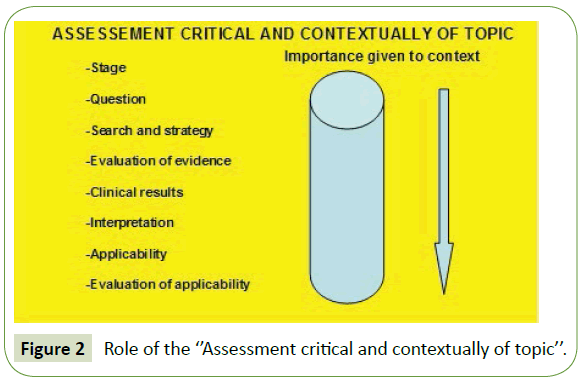
The usual procedure to resolve a clinical doubt is relatively standardized by following a series of steps that make up the specialist-based medicine or “Critical Assessment of a Topic”. In the resolution of these steps, the biopsychosocial context from which the question is extracted acquires a special emphasis in the beginning of this process-Initial stage/initial scenario and in the final stages of the process-applicability of the results and their evaluation. But, there is an alternative proposal which implies a greater relevance of the biopsychosocial context in all the phases of answer to the clinical question, by what it would be call the result of this process reasonable clinic in family medicine or “Assessment Critical and Contextually of a topic”. Medical science suffers from a kind of agnosia which avoids matters related to contextual judgment, the particular, the personal, and is made exclusively abstract and statistical. But the quantitative and the Evidence- Based Medicine cannot give us integral responses. In medical decision making there is an imposture of rational maximization without valuate this could be not reasonable. Quantitative studies are necessary, indispensable, but in this article, we have been forced to speak of stories as well as cases.
Keywords
Evidence based medicine; Family practice; Narration; Holistic health; Clinical questions
Introduction
Despite the progress in our diagnostic and therapeutic media, the uncertainty remains consubstantial with clinical practice. The clinic emerges-it is perceived by the clinician within its theoretical framework that nuances reality. From that moment, there are a number of clinical strategies to manage the uncertainty of decision-making.
From the paradigm of positivistic science ("quantitative and objective"), the specialist clinician uses primarily as strategies to manage uncertainty the clinical epidemiology and Evidence- Based Medicine (EBM) [1]. To this strategy we could call it "specialist-based medicine" or "Critical Assessment of Topic" (Figure 1). But the family doctor, although employing this strategy, also frequently uses many more techniques, not quantitative but qualitative, which are based on the "particular", and which we could call "reasonable clinic in family medicine" or "Assessment Critical and Contextually (Figure 2), which includes contextualization, experience, continuity of care for the person, common sense, strategic planning, resource use and strengths of patients and the same health professional, the self-esteem, selfcapacity, self-efficacy, emotion, intuition, ethics, participation of patients and communities, use of our senses, test of time, compassion, ecological and network relationships, the focus on the process instead Of the result, clinical interview and empathy, clinical history and narration, efficiency and effectiveness, the creativity, etc. In this alternative, the importance of the context remains with the same intensity in all phases of the search for response to clinical questions [2].
In contrast to what happens in the “Critical Assessment of a Topic” (Figure 1), in the “Assessment Critical and Contextually of a topic” model (Figure 2) we find it important to be aware that the selection of the scenario is not neutral and any scenario we choose already determines the choice of some questions instead of others [3].
Science asks questions about what can be objectively verified. EBM can be considered as "The conscious, explicit and judicious use of the best evidence available to make clinical decisions in sick individuals" [1]. But in primary health care (PHC) we do not differentiate between sick and healthy individuals, so we speak of global or integral individuals whose approach always requires considering multiple variables that interact in a complex and dynamic way. In PHC the pathology is organized more as health problems than as isolated diseases. Segregating one aspect of the total health problem could lead to the misconception that the sum of clinical questions constitutes the whole of the clinical management of integrated health problems in a real patient. Therefore, in an “Assessment Critical and contextually of a topic”, the qualitative aspects and the form of expression of the context, must be part, not only of the scenario but also of the own question thus establishing the natural relations between the parts and the whole.
Including qualitative data in the question of an “Assessment Critical and contextually of a topic” obliges to search, besides tests in quantified digitized databases as in the “Critical Assessment of a Topic”, also qualitative tests of the answer that we give ourselves. Its test search strategy requires specific skills: conversational, observational, documentary, etc.
Clinical Observation
Clinical question including qualitative data (contexts)
Homer, 69, has important forgetfulness that affects the comfort of his life and his family. In addition, he has diabetes and hypertensive heart disease with heart failure, obesity and venous insufficiency. He has been referred from the emergency department to a neurology clinic, and he comes with diagnosis of Alzheimer's Dementia. After several months already treated with galantamine the family (two daughters and a daughter-in-law) doubt whether or not the patient had experienced improvement in memory or quality of life. Family doctor ask the daughter, more involved in their care, that if this treatment is essential to improve their memory or quality of life given that they take many other medications (diabetes, hypertension, health failure, etc.) and if she would like to remove it if it were not essential.
Search strategies quantitative and qualitative
Selection of MBE resources with studies on results in treatment with acetylcholinesterase inhibitors in patients with Alzheimer's disease in databases. Establish contact with the patient and relatives interested in expressing an opinion on the level of improvement-quality of life-of his/her relative and interested in expressing opinion on the suitability of the indefinite use of the medication. Establish contact with nurse and social worker and know their impressions after the visit to the patient's home and social resources for the problem. Review of the clinical history of the patient to know the rest of their health problems and thus weigh better benefits and damages related to the acetyl cholinesterase inhibitor drugs. Reflect and comment with other professionals on the praxis of Hospital Care and Primary Care in our area for this health problem and be able to make our solution practicable.
Quantitative and qualitative results
-The quality of studies is poor.
-There are minimum benefits in memory.
-No benefits in the quality of life of patients or caregivers.
-It does not avoid institutionalization.
-Patients who do not stabilize or improve in the first few months (about six months) of anticholinesterase therapy are unlikely to have any benefit afterwards.
-The caretaker who "paid more attention" to the patient after 8 months of treatment did not have the impression that her father's quality of life had improved and aspired to a better life alternative for her father.
Interpretation of tests
-Clinical relevance is only valued by the specialist.
-The diagnosis and need for treatment with acetyl cholinesterase inhibitors in Alzheimer's disease is based on a certain difference in cognitive tests, whose clinical relevance in terms of its effect on disability and institutionalization has not yet been established.
-The main caretaker seems to demand that we do something that is "really useful" to both her and her father.
Decision making
-To reinforce -via social worker and appropriate social resources- a more intense support to the caregiver who seemed most effective for the welfare of Homer.
-To raise a reinforcement to the educational work of nursing (maintenance of the activity, aids to the memory, etc.).
-Reinforce family support (coaching interviews with caregivers, etc.).
-Monitor the treatment of complications.
-Be aware of novelties in the pharmacological approach of "Alzheimer's disease".
-Be attentive to developments in the non-pharmacological approach of "Alzheimer's disease".
-Be aware of novelties of potential benefits of cholinesterase inhibitor drugs in people with concomitant cardiovascular problems and Alzheimer's disease and in patients with Vascular Dementia and Mixed Dementia.
Evaluation of applied decisions
-The family continues to give acetylcholinesterase inhibitors treatment to Homer, but the primary caregiver talks about suspending it. Homer has begun to receive the visit of a grand daughter who works in a nursery with which plays children's games twice a week.
-The Health Center nursing team is debating whether to include patients with cognitive disorders between their scheduled visits.
-Homer's family doctor has initiated a more comprehensive approach in of the rest of his patients with cognitive disorders.
-The confidence in Homer's family doctor has been greatly reinforced by the entire family of Homer.
Discussion
Parallel to the universal acceptance of MBE, a whole science of makeup of clinical trials has been constructed; whose objective is the introduction of new treatments in clinical practice". One of many consequences is that we are moving towards an increasingly medicalized life, where almost nobody goes to get rid of being treated, not because of an illness which affects their quality of life, but for having one or more risk factor's [4]. This makes us think that the critical reading of quantitative studies increasingly requires skills that are moving away from the most crucial skills of family doctor. A feasible alternative to the interpretation of quantitative tests by the family doctor itself could be to take refuge in the filtered sources of MBE Resources.
Also, qualitative quality assessment, on the other hand, requires specific technology and must be practiced in “Assessment critical and contextually of a topic”: epistemological adequacy, relevance, validity and reflexivity [5]. The clinical results in the "Assessment critical and contextually of a topic” imply both the description of the quantitative and qualitative results.
The superficial thought is summarized in that the specialist tends to know much of almost nothing and the generalist to know almost nothing of almost everything. However, a developed thought will be one where the generalist studies the fragments from the knowledge of the whole [6,7]. The solution of the conventional Scientific Method is to zoom in and divide it into fragments. The “Assessment critical and contextually of a topic” or reasonable clinic in family medicine, involves applying systemic thinking by focusing on meaningful relationships. Thus, an interpretation a diagnosis is constructed by inducing categories, triangulating and analyzing speeches.
In family medicine we need to know that "dividing an elephant in half does not produce two small elephants". As human systems are infinitely complex, we cannot understand everything (or dividing it into parts); we have cognitive limitations. The division of disciplines makes it impossible to take what is woven together so, that to maintain this systemic approach, is required, increasingly, a general practitioner. It has been shown that an increased use of specialists not associated with better health and it increases costs. It is best to keep the patient in primary care whenever possible. Seeing a holistic or comprehensive view of the patient is to take into account the interrelationships of the various dimensions of a person and see the whole as greater than the sum of its parts, as well as the acceptance of integration, or the whole, as a fact.
Uncertainty in family medicine is not solved, "it is managed" [8]. The King Solomon used common-sense knowledge to fill the gaps of evidence by using his wisdom to resolve the conflict by obtaining more evidence. He was a king famous for his wisdom. Two women claiming to be the mother of a baby were once to his audience. Solomon had little evidence since there were no witnesses and the two testimonies seemed equally plausible. His solution was to order the child to be cut in two. When one of the women protested that she preferred to be given to the other before baby was killed, the king acknowledged that she was the true mother. A "good" decision is one whose execution reduces uncertainty, usually by obtaining more information, or reduces the impact of uncertainty. Controlling a problem is basically deciding what to do next.
In the “Assessment critical and contextually of a topic” or reasonable clinic in family medicine is necessary to take into account the individual and unique of each patient. We can discriminate between many approaches to reduce uncertainty, as well as between different kinds of evidence, and judge the "usefulness" of it and decide whether it has value. The appropriateness of the evidence depends on what it is going to be used for. In addition, we must see the evidence in context. The same evidence does not have the same weight for each context. And it may be appropriate in one context, but not in another. Therefore, the interpretations of "true" and "false" have to be modified. A conclusion may be "sufficiently true" in one situation, but not in another. On the other hand, there are degrees of trust in the evidence: for example, in most contexts, witness testimony is preferable to circumstantial evidence, direct evidence to indirect, the corroboration to contradiction, inference to the assumption [8]. In family medicine we also use the contextualization, clinical experience, empathy, problem solving, therapeutic alliance, etc. [2,9-11].
In relation of the difference between reasonableness and rationality (reasonable and rational), Sen, Harvard University, once devoted the class to examining the difference between these concepts, and expounded the tragic example of the person who is going to commit suicide and that carefully evaluates the most efficient methods of killing oneself by comparing its economy of pain and suffering, Time between the lethal action and actual death and the safety of achieving the ultimate goal. For this purpose he or she compared the death by firearm or poison, by means of the gallows or by throw him or herself off a cliff until finding the most effective means to achieve its purpose. By its procedures, the suicide is rational because it maximizes the utility of the means with respect to the ends, but it is not reasonable since the purpose of taking the life leads them to the end of all possibility of proposing a purpose. Sen with this ingenious metaphor of contemporary economics illustrate the imposture of rational maximization but not reasonable [12].
The objective is also to make explicit the reasoned basis of a clinical decision that we have prioritized for any reason: in short, to practice a “Clinically Reasonable quantitatively and qualitatively”. A clinical question is always part of a network of questions only partially contained in clinical guidelines since they contain only those that are considered common to other individuals similar to our patient but not their specific ones [13]. The final objective is to see to what extent that response seems to explain the initial scenario and modify it. Sound clinical decisions should ideally be driven by an amalgam of evidence, values or preferences, and circumstances [14].
Conclusion
Medical science suffers from a kind of agnosia [15]. It avoids matters related to contextual judgment, the particular, the personal, and is made exclusively abstract and statistical. But technology, the quantitative, and the MBE cannot give us integral responses and both restore our professional satisfaction. Our profession will have to rebuild the sense of qualitative, teamwork, community and the bonds that unite us as human beings. This will require spending more time between specialists and generalists and our patients, restoring some rituals that are meaningful both to us and to the people we care about and eliminating those who are not [16]. So, in this alternative way, to resolve the clinical doubt implies a greater relevance of the biopsychosocial context in all the phases of answer to the clinical question, that is to say, to means a “reasonable clinic” or “Assessment Critical and Contextually of a topic”.
EBM, clinical trials and quantitative studies are necessary, indispensable, yes, but why not the stories, the tales and the cases? It was Hippocrates who introduced the historical concept of disease, the idea that diseases follow a course, from their first signs to their climax or crisis, and then to their fatal or happy outcome. Hippocrates thus introduced the clinical history, a description of the natural history of the disease. Such records, as actually EMB, nothing tells us about the context in which the individual experiences and confronts his illness [17]. In the rigorous specialist-based medicine or in the “Critical Assessment of a Topic” there is no context or "subject". Its responses to clinical questions or comments could be also applied as to a rat in the lab the same form that to a human being in the family and community. To delve into the true clinical history we have to do storytelling. Only then will we have a "who" as well as a "what", a real individual in a particular context. Thus, we, as Sackcs says, in this article, have been forced to speak of stories as well as cases [15].
References
- Sackett DL, Richardson WS, Rosenberg W, Haynes RB (1997) Evidence-based medicine. Howtopractice andteach EBM. New York: Churchill Livingstone, USA.
- Turabian JL, Pérez FB (20003) Habilidades cruciales del médico de familia y sus implicaciones en la Gestión y la formación: Diagnóstico, tratamiento, cura y resolución. Cuadernos de Gestión 9: 70-87.
- Thomas P (2006) General medical practitionersneedto be aware of thetheoriesonwhichourworkdepend. Ann FamMed 4: 450.
- Orueta SR, Rodríguez SC, González HE (2011) Medicalisation of every-daylife (I). RevClinMedFam, p: 4.
- Calderón GC (2009) Assessingthequality of qualitativehealthresearch: Criteria, process and writing. ForumQualitativeSozialforschung/Forum: Qualitative Social Research, p: 10.
- Pérez FB, Turabian JL (2007) Framework of competences of familydoctors:Clinicsorpeople? Aten Primaria 39: 41-43.
- TurabianJl (2007) El misterioso caso delmédico de familia. JANO 1636:14.
- Turabian JL, Perez FB (2006)Theprocessbywhichfamilydoctorsmanageuncertainty: Noteverythingiszebrasorhorses. Aten Primaria 38:165-167.
- Turabián FJL, Pérez FB (2005) A waytomakeclinicalpragmatismoperative: Sistematizationof theactuation of competentphysicians. MedClin (Barc) 124:476.
- Turabian JL (2009) Specifictoolstomanagecomplexconsultations in general practice. BMJ 338:b1187.
- Turabian JL, Perez Franco B (2008) Do familydoctorsseemliketurtles? Semergen 34:373-375.
- Sen A (2002) Rationality and freedom. Cambridge: MA: Harvard UniversityPress, USA.
- Hayes C, Naylor R, Egger G (2012) Understandingchronicpain in a lifestylecontext: Theemergenceof a whole-personapproach. Am J LifestyleMed 6: 421-428.
- Naylor CD (2001) Clinicaldecisions: Fromart toscience and back again. Lancet 358:523-525.
- Sacks O (1998) Themanwhomistookhiswifefor a hat. New York: Touchstone, USA.
- Rosenthal DI, Verghese A (2016) Meaning and thenature of physicians.Work N Engl J Med 375:1813-1815.
- Turabian JL, PerezFB (2016)Thefamilydoctors: Images and metaphors of thefamily doctor tolearnfamily medicine. New York. Nova Publishers, USA.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences