Proposal of fetal asphyxia treatment without caesarean delivery
Kazuo Maeda*
Department of Obstetrics and Gynecology,Seirei-Mikatahara Hospital, Hamamatsu,Japan
- *Corresponding Author:
- Kazuo Maeda
Department of Obstetrics and Gynecology
Seirei-Mikatahara Hospital, Hamamatsu
Japan
Tel: +81 53-474-2222
Fax: 81-859-22-6856
E-mail: maedak@mocha.ocn.ne.jp
Received date: February 08, 2018; Accepted date: February 11, 2018; Published date: February 16, 2018
Citation: Maeda K (2018) Proposal of Fetal Asphyxia Treatment without Caesarean Delivery. J Women’s Health Reprod Med. Vol.2 No.1:1
Abstract
Aim: To reduce caesarean delivery in NRFS cases with intrauterine treatment of fetal asphyxia.
Method: The nonreassurig fetal status (NRFS) case of high placental gray level histogram width (GLHW), which is a tissue characterization, in fetal growth restriction (FGR), the mother is proposed to be treated by heparin infusion, if diagnosed as fibrin depsit in placental intervillous space, under monitoring with ultrasonic Doppler uterine arterial flow, fetal heart rate (FHR) and hemorrhagic tendency etc. a vaginal delivery is selected, if NFRS disappeared, GLHW lowered, estimated fetal weight recovered, and uterine arterial Doppler normalized. The vaginal delivery is carefully monitored in hospital, preparing caesarean delivery in any abnormality.
Results: A 2nd trimester FGR case who had high GLHW was treated byheparin 5000 U infusion every day 17-31 weeks every day.
Keywords
Fetus; Asphyxia; Fetal heart rate; Tocolysis; Maternal posture; Fetal growth restriction; Fibrin deposit; Intervillous space; GLHW; Tissue characterization; Heparin
Introduction
Fetal hypoxia caused fetal brain damage [1], where nonreassuring fetal status (NRFS) caused by hypoxia has been treated curing the fetus with Caesarean delivery (C-delivery) increasing maternal morbidity. Is it impossible to reject hypoxia while keeping fetus in the uterus without C-delivery? Maternal oxygen inhalation was tried but failed to achieve sufficient oxygenation [2]. Uterine hypercontraction, a cause of asphyxia, was treated by tocolysis [3], placental insufficiency was treated when asphyxia was caused by the compression of iliac artery reducing placental blood flow, i.e. it was removed by maternal lateral posture in late deceleration [4]. Studies were targeted to placental villi but only its dysplasia was found in preeclampsia by scanning electron microscopy [5] and its role to develop fetal hypoxia was unknown. The oxygen transfer function of chorionic membrane of placental villi was unknown in the past. The fibrin deposit in intervillous space was found to cause fetal growth restriction (FGR) and hypoxic damages [3]. Dangerous changes in pulsed Doppler flow wave were pointed out, but its developing mechanism was not reported. As the dangerous flow wave was absent or reverse flow of end-diastole (ARED), and high resistance index indicating increased peripheral flow resistance.
Methods
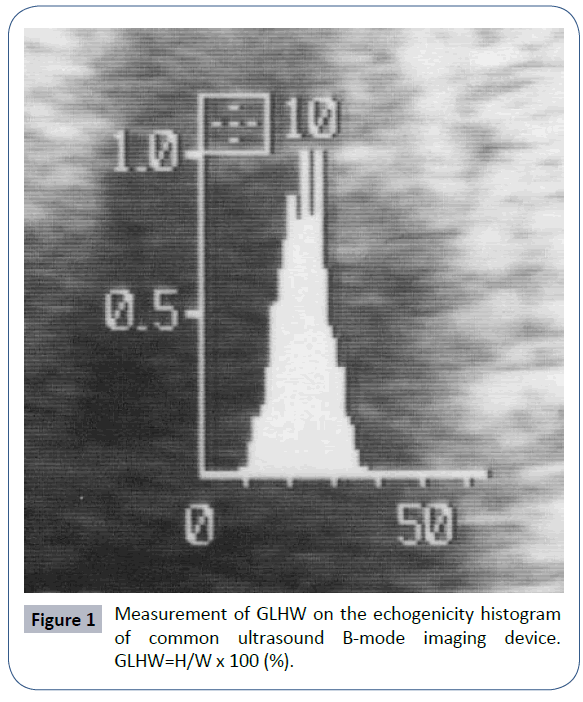
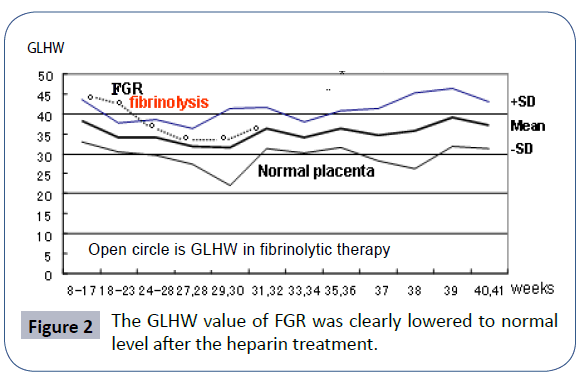
The clue of this study was the solution of fibrin deposit in placental intervillous space by heparin administration to the mother of fetal growth restriction (FGR), estimated by reduced fetal weight in the 2nd trimester, where the fibrin deposit in the placenta was estimated by the increased gray level histogram width (GLHW) tissue characterization calculated by the histogram width divided by full length of 64 bits length in the echogenicity histogram of common ultrasound B-mode devices (Figure 1), Which was standardized using RMI 412 ultrasound phantom (Radiation Measurement Inc. Middleton, WI, USA) and various ultrasound B-mode imaging devices [3]. Automated GLHW is shown by “%W” index in the histogram of Aloka B-mode device (Tokyo). The GLHW value was stable if the device gain was changed, but it increased if the image contrast was high, thus, the contrast level of B-mode device was the lowest in GLHW studies. GLHW value was high also in malignancy, fibroid, fetal periventricular echo density, meconium stained amniotic fluid [4], and it was low in immature fetal lung [5]. As cardiolipine was positive in the patient of high GLHW due to fibrin deposit in placental intervillous space, which was treated every day by 5000 U heparin infusion, where GLHW was lowered, estimated fetal weight increased, no asphyxia developed, and achieved normal neonate (Figure 2). While the fetus of no heparin treatment was died in previous pregnancy of the same mother [3]. Therefore, it was estimated that placental villi transfer of nutritive material was reduced by fibrin deposit developing FGR, while the small molecules of oxygen was restricted in later period of pregnancy, developing severe hypoxia to cause fetal demise in previous gestation. The theory was confirmed in another work on asphyxia in FGR, where 20 FGR cases of normally positive FHR acceleration and the other 20 FGR cases of no acceleration were compared. Positive acceleration cases maintained normal brain response to fetal movements, and there was no fetal asphyxia, however the 20 cases who lost FHR acceleration against fetal movement burst (non-reactive fetal state) developed severe asphyxia receiving C-delivery followed by severe neonatal asphyxia and neonatal death and the loss of FHR variability, which was the sign of fetal brain damage, namely FHR variability was the response of fetal brain to minor fetal movements. Namely, firstly lost FHR acceleration then severe fetal asphyxia with the loss of FHR variability, where fetal brain function was lost, which was the same as fetal anencephaly, and neonatal death appeared even after C-delivery [6]. Intervillous space fibrin deposit may develop uterine arterial resistance which will be shown by the ARED by ultrasonic pulsed Doppler flow wave, at the same time of increased placental GLHW, namely, the NRFS indicates fetal hypoxia, which would be treated by the fibrin deposit solution by heparin in cases of high placental GLHW, where the fibrin deposit was solved by heparin, of which favorable effect was shown in the FGR treatment in Utsu’s study [3].
Results
The conditions of hypoxic fetal damage were FGR, high GLHW tissue characterization and abnormal Doppler flow wave indicating increased placental blood flow resistance. The conditions will suggest the solution therapy of placental fibrin deposit, of which pathological evidence (Figure 2) would be confirmed by placental tissue sampling, if necessary. The effect of heparin treatment was shown in the improvement of FGR resulting the recovery to fetal normal estimated weight, recovery to normal uterine arterial Doppler flow wave, the loss of fetal asphyxia, prevention of fetal damage even preventing fetal death after the heparin treatment as shown in our past report [3].
Discussion
Proposal
Above results will show the effect of heparin treatment to fetal asphyxia, reduced GLHW, increased estimated fetal weight, and recovery of abnormal FHR, by recovered placental blood flow, normal Doppler flow of uterine artery, recovery from fetal hypoxia in the FGR associating low fetal estimated weight, high placental GLHW and abnormal pulsed Doppler flow of uterine artery, even if there is no placental tissue sampling, which will be a high risk technique, while heparin is not contraindicated if there is no hemorrhagic disease. Thus, fetal asphyxia associated NRFS of FHR, FGR and increased ultrasonic echo-density which is confirmed by high GLHW level, will be tried to be treated with 5000 unit heparin infusion every day measuring uterine arterial Doppler flow, placental GLHW, estimated fetal weight, and the care on the tendency to hemorrhage. Heparin therapy will be sustained when NRFS disappear, estimated fetal weight increased, placental GLHW is normal pregnancy level and uterine arterial Doppler flow is normal. Very careful fetal monitoring is needed in hospitalized condition, enabling C-delivery any time, if vaginal delivery is selected.
Conclusion
A novel technique to treat hypoxic NRFS curing from the brain damage or fetal/neonatal death by heparin therapy is proposed in the FGR associating high GLHW tissue characterization and abnormal pulsed Doppler flow of uterine artery, hopefully without C-delivery.
References
- Maeda K, Kimura S, Nakano H (1969) Pathophysiology of Fetus, Shukudai report, 51st Ann Convention, JSOG, Kanazawa, Japan.
- Tsubaki O (1979) Scanning electron microscopic studies on the placental villi in toxemia of pregnancy. Acta Obstetrica Gynecol Jpn 31: 537
- Maeda K, Utsu M, Kihaile PE (1998) Quantification of sonographic echogenicity with grey leel histogram width. A clinical tissue characterization. Ultrasound Med Biol 24: 225-234.
- Maeda K (2005) Ultrasound tissue characterization with the gray level histogram width of the B-mode. Ultrasound Rev Obstet Gynecol 5: 92-95.
- Serizawa M, Maeda K (2010) Non-invsive fetal lung maturity prediction based on ultrasonic gray level histogram width. Ultrasound Med Biol 36: 1998-2003.
- Teshima N (1993) Non-reactive pattern diagnosed by ultrasonic doppler fetal actocardiogram and outcome of the fetuses with non-reactive pattern. Acta Obstet Gynecol Jpn; 45: 423-430.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences