ISSN : 2576-3938
Journal of Emergency and Internal Medicine
Prognostic Value of Vitamin D Status in Pediatric Patients with Acute Kidney Injury in Tanta University Emergency Hospital, Egypt
Mohamed A El-Gamasy*, Mohsen M Eldeeb and Mohmed M. Abdelmageed
Faculty of Medicine, Department of Pediatrics, Tanta University, Egypt
- *Corresponding Author:
- Mohamed A El-Gamasy
Faculty of Medicine, Department of Pediatrics, Tanta University Hospital, El-Giesh Street, Tanta, Gharbia, Egypt.
Tel: +2 01208136076
Fax: +20403333666
E-mail: mgamsy@gmail.com
Received Date: May 07, 2017; Accepted Date: June 01, 2017; Published Date: June 07, 2017
Citation: El-Gamasy MA, Eldeeb MM, Abdelmageed MM ( 2017 ) Prognostic Value of Vitamin D Status in Pediatric Patients with Acute Kidney Injury in Tanta University Emergency Hospital, Egypt. J Emerg Intern Med. Vol. 1 No. 1 : 5.
Abstract
Background: AKI is an independent predictor of morbidity and mortality for critically ill children at Pediatric Emergency Departement (PED) which are liable for vitamin D deficiency. It is proposed that vitamin D concentration may be either a biomarker or a co-factor of survival in PED. The aim of this work is to assess serum 25-(OH)D level in critically ill pediatric patients with AKI at PED within the 1st 24 hours of admission and evaluate its correlation with duration of hospital stay and mortality outcome.
Subjects and methods: This study was conducted upon 80 critically ill pediatric patients with AKI during the first 24 hours after hospital admission. AKI was diagnosed according to the Acute Kidney Injury Network (AKIN) criteria for serum creatinine. We analyzed the demographic data, PRISM III for severity of illness, CBC, CRP, serum Ca, serum Phosphorus, serum 25(OH)D and its correlations with studied variables. We compared between vitamin D severely deficient, insufficient and sufficient subgroup of patients.
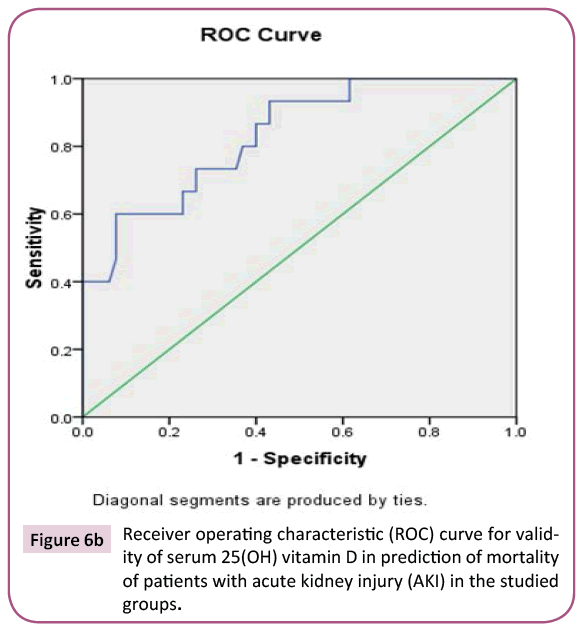
Results: Vitamin D deficiency occurs in two third of studied patients versus one third of studied controls. There is a significant negative correlation between vitamin D level and age of patients, sepsis, death probability and serum phosphorus level, but there is a significant positive correlation between vitamin D level and serum calcium levels. There was statistically significant increase in death outcome with increased number of system failure, PRISM III score, decreased weight, height percentiles and sepsis, so they can be considered as predictors of mortality. ROC curves denote that 25 (OH) D levels are more valid than CRP in prediction of mortality.
Conclusion: Vitamin D deficiency was associated with higher incidence of sepsis and mortality.
Keywords
AKI (Acute Kidney Injury); 25(OH)D; PRISM III score; Mortality; Emergency
Introduction
AKI remains an independent predictor of morbidity and mortality for critically ill children despite of advances in the provision of hospitalized care [1-3]. Management of AKI is directed toward reversing the underlying cause and providing supportive care including avoidance of nephrotoxic medications, normalizing electrolytes and fluid status as well as maintaining hemodynamic stability and kidney perfusion with vasoactive medications and mechanical ventilation [4-7]. Recent evidence suggests that the role of vitamin D is broader than the regulation of calcium metabolism [8]. Vitamin D is a pleiotropic hormone important for the proper functioning of multiple organ systems [9]. Low level of 25(OH)D is associated with greater catecholamine requirements than in normal vitamin D status [9]. Critically ill children at pediatric Intensive Care Unit (PICU) or PED are liable for vitamin D deficiency [9]. Vitamin D has been shown to influence cardiac myocytes and endothelial function through cellular receptors, altering gene and protein expression, signal transduction, and enzymatic reactions [9]. Pediatric case series reported that vitamin D receptors are present on major immune blood cells, modulating white cell proliferation, maturation, cytokine release, antimicrobial peptide, and Toll-Like Receptor levels (TLR) [9].
A recent PICU study observed longer survival times among vitamin D sufficient patients and concluded that vitamin D concentration may be either a biomarker or a co-factor of survival [10].
The aim of the work was to assess serum 25 (OH)D level in critically ill pediatric patients with AKI at PED of Tanta University Emergency Hospital (TUEH) within the 1st 24 hours of admission and evaluate its correlation with duration of hospital stay and mortality outcome.
Materials and Methods
Design of the study and setting
This cross sectional study was conducted upon 80 pediatric patients aged from 3 months to 12 years who were hospitalized at PED of TUEH in the period from June 2016 to June 2017. Their ages ranged from three months to 12 years. They were 46 males and 34 females, 34 cases (below 1 year), 26 cases (between 1 year and 4 years), 20 cases (between 4 years and 12 years). Twenty completely healthy subjects of comparable age and sex were served as a control. They were 11 males & 9 females. 9 (below 1 year), 7 (between 1 year and 4 years), 4 (between 4 years and 12 years). The study was conducted after approval from the Ethical Committee of the Faculty of Medicine, Tanta University and informed verbal or written parental consents from all subjects involved in the study.
Inclusion criteria
Pediatric patients with AKI aged from 3 months to 12 years with hospital admission more than 24 hours. AKI was diagnosed when 0.3 mg/dl or 50% increase in serum creatinine of reference range occurred within 48 hours according to the Acute Kidney Injury Network (AKIN) criteria for seum creatinine [11].
Exclusion criteria
Patients with known or suspected parathyroid gland or pituitary gland disease, Patients transferred from another hospital, Patient were on chronic vitamin D supplementation, ricketic patients, and family history of rickets, patients with chronic hepatic disease or chronic kidney diseases and patients on anti-conversant treatment.
Study protocol
All patients and controls were subjected to history taking (about sun exposure, type of milk supplementation, vitamin D supplementation in infancy, ,onset of disease, hospital admission, presence or absence of sepsis, need for mechanic ventilation(MV) , duration of MV, number of organ system failure and mortality outcome), full clinical examination (weight and height for age percentiles according to Egyptian growth curves).
Severity of illness in the first 24 hours of admission was assessed by Pediatric Risk of Mortality score (PRISM III) [12] and the follow up was with the Sequential Organ Failure Assessment (SOFA) score [13].
The routine laboratory tests were: Complete blood count (CBC) by ERMA BC 210, C-Reactive protein (CRP) by Adiva Centaur CP/ Immunoassay, Arterial blood gases (ABG), Prothrombin time (PT) and activity by Sysmex CA 1500, Serum creatinine by kinetic assay using Kone Lab Prime 60I), liver function tests (AST and ALT) by Kone Lab Prime 60I), serum Calcium (total and ionized), serum Phosphorus and analysis of serum 25(OH)D. Under sterile aseptic techniques, 3 mL of venous blood were withdrawn in a sterile test tube. Blood samples were centrifuged for 10 minutes at 1000- 3000 rpm. The supernatant was stored at -20°C until 25-OH vit D analysis.
The Principle of 25(OH)D assay
It was performed by ELISA technique (within 24 hours of hospital admission) by double-sandwich ELISA technique using ELISA Kit (MyBiosource USA). The pre-coated antibody is human VD monoclonal antibody and the detecting antibody is polyclonal antibody with biotin labeled. Samples and biotin labeling antibody are added into plate wells and washed out with PBS or TBS. Then Avidin-peroxidase conjugates are added to wells in order; Use TMB substrate was used for coloring after reactant thoroughly washed out by PBS or TBS. TMB turned into blue in peroxidase catalytic and finally turned into yellow under the action of acid. The color depth and the testing factors in samples were positively correlated.
Statistical analysis
The collected data were analysed using SPSS version 20 software (SPSS Inc., Chicago, IL, USA). Categorical data were presented as number and percentages whereas quantitative data were expressed as range and median. Chi‑square test, Receiver operating characteristic (ROC) curve was used to determine cutoff values of the studied mortality scores with optimum sensitivity and specificity.
Multiple regression analysis: The accepted level of significance is at 0.05 (P<0.05 was considered significant and P>0.05 is nonsignificant [14].
Results
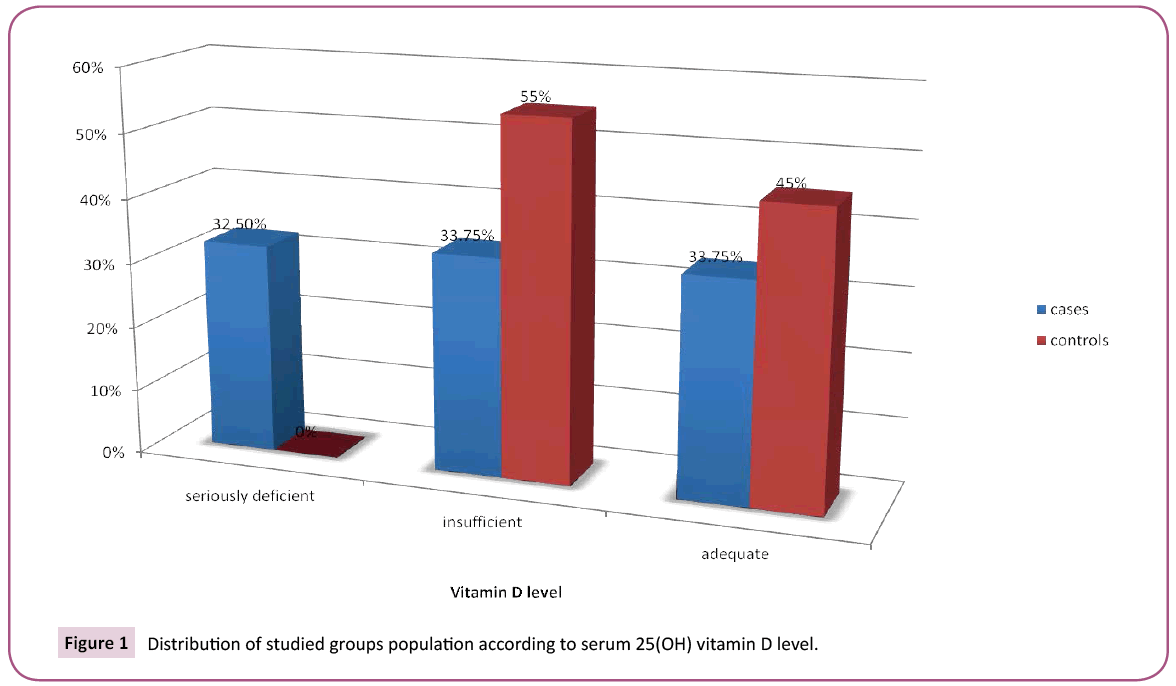
Patients were classified according to 25(OH) Vitamin D level into three subgroups, seriously deficient (< 30 nmol/L), Insufficient (30-75 nmol/L), Adequate (>75 nmol/L) (Figure 1). Table 1 summarizes the causes of AKI in the studied patients. Table 2 summarizes demographic and laboratory data of studied patients. The severity of critical illness on admission was evaluated using PRISM III score which showed no statistically significant difference between studied subgroups. Patients with vitamin D deficiency had higher age than those with adequate levels.
| Cause of AKI | Respiratory | Pneumonia: N (%) | 20 (25%) |
| Bronchiolitis: N (%) | 6 (7.5%) | ||
| Status asthmaticus: N (%) | 10 (12.5%) | ||
| Pleural effusion: N (%) | 4 (5%) | ||
| Neurological | Guillian Barrie Syndrome: N (%) | 6 (7.5%) | |
| CNS infection: N (%) | 1 (1.25%) | ||
| Brain tumor: N (%) | 1 (1.25%) | ||
| Cardiovascular | Heart failure: N (%) | 7 (8.75%) | |
| Septic shock: N (%) | 1 (1.25%) | ||
| Congenital heart disease: N (%) | 7 (8.75%) | ||
| Hematological | Acute hemolytic crises: N (%) | 4 (5%) | |
| Aplastic crises: N (%) | 1 (1.25%) | ||
| Malignancy: N (%) | 1 (1.25%) | ||
| Metabolic | Diabetic ketoacidosis: N (%) | 11 (13.75%) | |
| AKI: Acute Kidney Injury. Data were expressed as number (%) |
|||
Table 1: Admission diagnosis of the underlying causes of AKI in the studied patients.
| Variables | 25OH vitamin D groups (number and percent) |
P-value | |||
|---|---|---|---|---|---|
| Seriously deficient (<30nmol/L) 26 patients |
Insufficient (30-75nmol/L) 27 patients |
Adequate (>75nmol/L) 27 patients | |||
| Age (mo) | Median | 30m | 12m | 10m | 0.02* |
| Range | 3m-144m | 3m-84m | 3m-77m | ||
| Sex | Male No (%) | 16 (61.53%) | 15 (55.55%) | 15 (55.55%) | Chi square=0.879385 P=0.88 |
| Female No (%) | 10 (38.46%) | 12 (44.44%) | 12 (44.44%) | ||
| Onset | Acute | 15 (57.69%) | 16 (59.25%) | 18 (66.67%) | 0.971 |
| Acute on top of chronic | 11 (42.31%) | 11 (40.75%) | 9 (33.33%) | ||
| PRISM III score | Median | 9.5 | 9 | 9 | 0.249 |
| Range | 1-22 | 2-24 | 3-19 | ||
| Weight Percentile | Above 25th | 11 (42.31%) | 17 (62.97%) | 23 (85.18%) | 0.262 |
| Below 25th | 15 (57.69%) | 10 (37.03%) | 4 (14.82%) | ||
| Height percentile | Above 25th | 16 (61.54%) | 20 (74.07%) | 25 (92.59%) | 0.262 |
| Below 25th | 10 (38.46%) | 7 (25.93%) | 2 (7.41%) | ||
| Sepsis or not | No | 6 (23.08%) | 9 (33.33%) | 19 (70.37%) | 0.047* |
| Yes | 20 (76.92%) | 18 (66.67%) | 8 (29.63%) | ||
| Number of organ system failure on admission | < 3 No (%) > 3 No (%) | 2 (2.5%) 21 (26.25%) | 12 (15%) 5 (6.25%) | 40 (50%) 0 (0%) | |
| Mechanically ventilated or not | No | 19 (73.08%) | 21 (77.78%) | 20 (74.07%) | 0.833 |
| Yes | 7 (26.92%) | 6 (22.22%) | 7 (25.92%) | ||
| Duration of mechanical ventilation (days) | Median | 20 | 10 | 15 | 0.476 |
| Range | 0-30 | 0-25 | 0-34 | ||
| Duration of hospital stay (days) | Median | 20 | 20 | 30 | 0.745 |
| Range | 1-40 | 2-30 | 2-45 | ||
| Outcome | 0.04* | ||||
| Death No (%) | No (%) | 14 (53.85%) | 8 (29.63%) | 5 (18.51%) | |
| Discharge No (%) | No (%) | 12 (46.15%) | 19 (70.37%) | 22 (81.48%) | |
| Serum calcium (mg%) | Median | 7 | 9 | 11.2 | 0.045* |
| Range | 6.7-8 | 7-10 | 8-11.8 | ||
| Serum phosphous (mg%) |
Median | 6 | 5.5 | 4 | 0.044* |
| Range | 5-8.17 | 4-7 | 2-5 | ||
Table 2: Demographic and laboratory data of the studied patients.
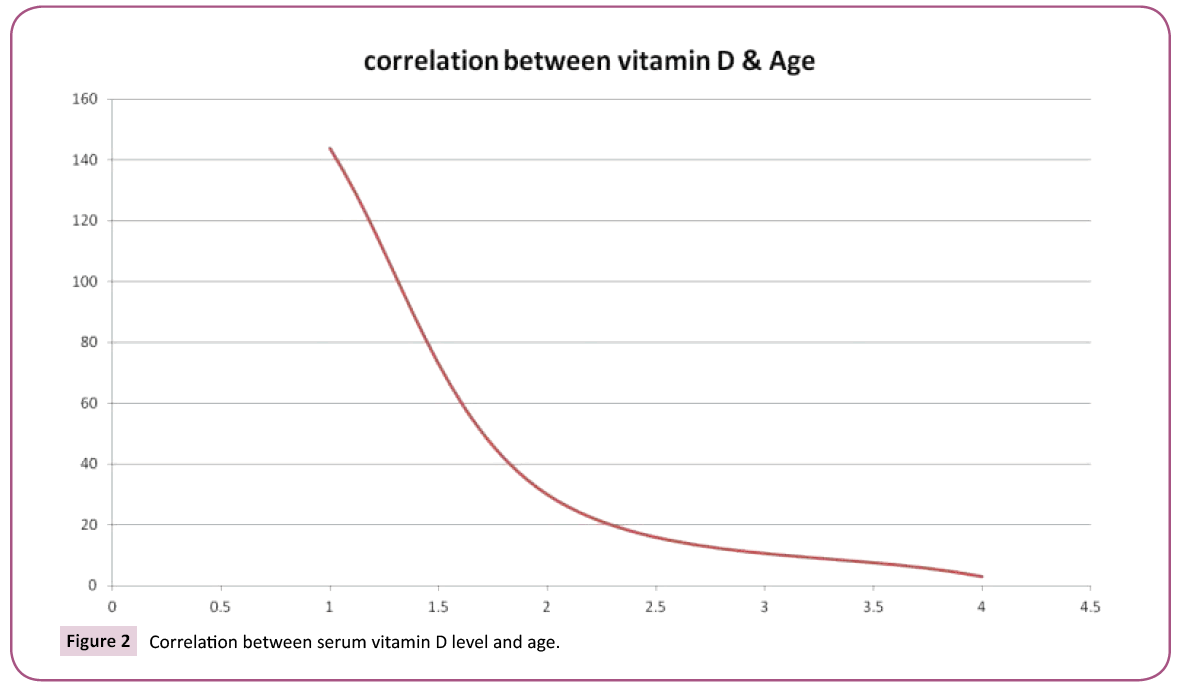
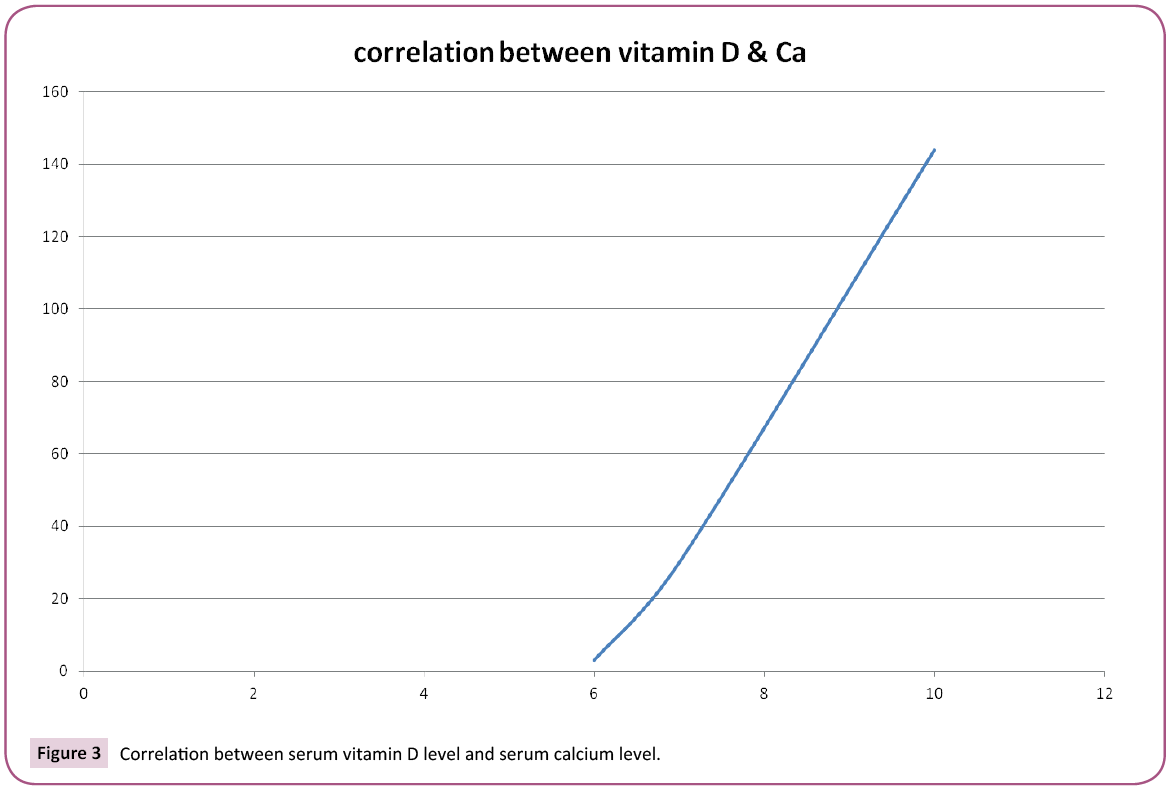
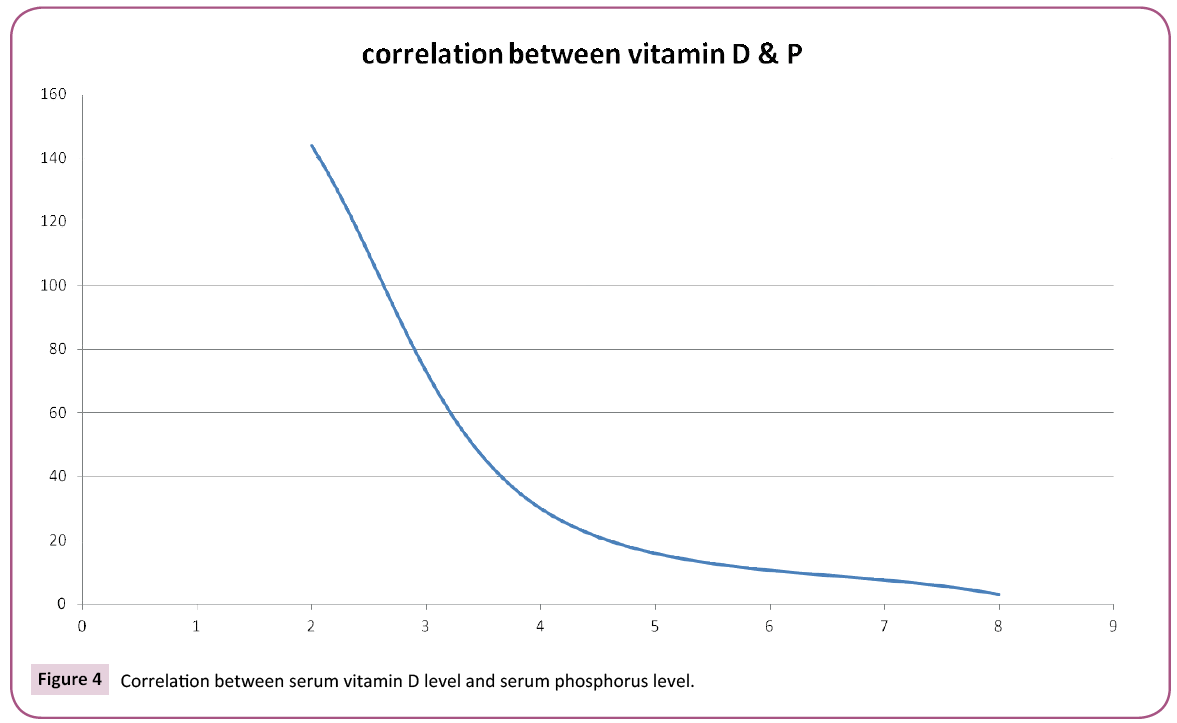
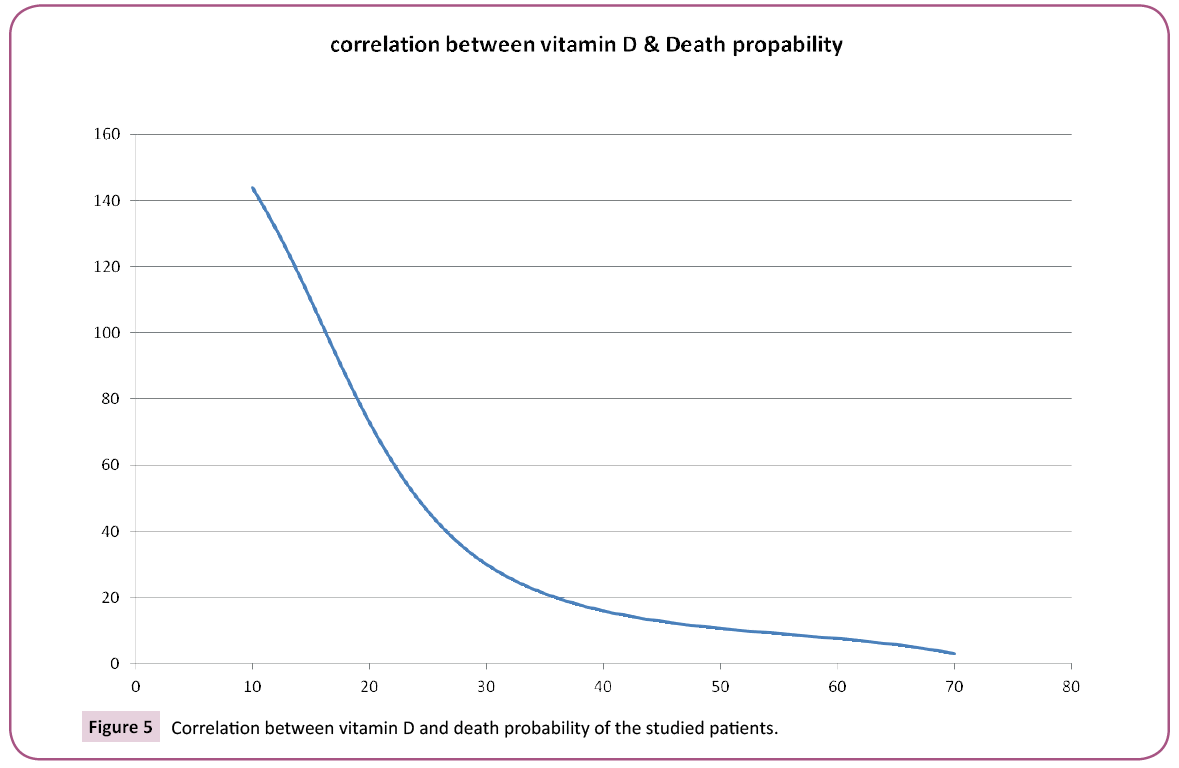
Table 3 and Figures 2-5 showed the correlations between vitamin D level and the studied variables, There is a significant negative correlation between vitamin D level and age of patients, sepsis, death probability and serum phosphorus level, But there is significant positive correlation between vitamin D level and serum calcium level, while there was no correlation between vitamin D level and onset of disease, PRISM III score, weight or height percentiles, mechanical ventilation or it's duration or duration of stay in PICU or number of organ system failure (p-value >0.05).
| Variables | r | P-Value |
|---|---|---|
| Age (mon) | -0.27 (weak correlation) | 0.02* |
| Death probability | 0.324 (weak correlation) | 0.04* |
| Ca | 0.340 (weak correlation) | 0.045* |
| PO4 | - 0.352 (weak correlation) | 0.044* |
| r =Spearman's Rho correlation. *P-value <0.05 is considered significant |
||
Table 3: Correlation between serum vitamin D and the studied variables.
Table 4 showed multiple regression analysis for 25(OH) vitamin D, showing a higher probability of sepsis and mortality outcome with vitamin D deficiency.
| Variables | Comparative analysis | Death | Discharge | P-Value |
|---|---|---|---|---|
| Age | Median | 60m | 72m | 0.271 |
| Range | 3m-144m | 5m-132m | ||
| Number of system failure | Median | 3 | 1 | 0.04* |
| Range | 3-4 | 1-3 | ||
| PRISM III score | Median | 18 | 8 | 0.004** |
| Range | 5-24 | 1-18 | ||
| Sex | Female:N (%) | 14 (51.85%) | 20 (37.74%) | 0.329 |
| Male:N (%) | 13 (48.15%) | 33 (62.26%) | ||
| Onset | Acute:N (%) | 14 (51.85%) | 35 (66.04%) | 0.608 |
| On top of chronic:N (%) | 13 (48.15%) | 18 (33.96%) | ||
| Weight Percentile | Above25th:N (%) | 3 (11.11%) | 48 (90.57%) | 0.040* |
| Below 25th:N (%) | 24 (88.89%) | 5 (9.43%) | ||
| Height percentile | Above25th:N (%) | 9 (33.33%) | 52 (98.11%) | 0.042* |
| Below 25th:N (%) | 18 (66.67%) | 1 (1.89%) | ||
| Sepsis or not | No:N (%) | 3 (11.11%) | 31 (58.49%) | 0.032* |
| Yes:N (%) | 24 (88.89%) | 22 (41.51%) | ||
| Calcium | Median | 8 | 9.6 | 0.232 |
| Range | 6.7-11.8 | 6.7-11 | ||
| Phosphorus | Median | 3.6 | 4 | 0.112 |
| Range | 0.8-8 | 0.7-8.17 | ||
| *P-value < 0.05 is considered significant. | ||||
Table 4: Comparative analysis between died and lived patients according to studied variables.
Table 5 showed comparison between death & discharge outcomes of the studied patients as regard to different studied variables. There was statistically significant increase in death with increased number of system failure, PRISM III score, sepsis and decreased weight , height percentiles (p-value < 0. 05), so they can be considered as predictors of mortality.
| Variables | Coefficients | Standard Error | t Stat | P-value | Lower 95% | Upper 95% |
|---|---|---|---|---|---|---|
| Sepsis | -0.560 | 0.173 | -3.210 | 0.003 | -0.510 | -0.209 |
| Onset | 27.887 | 21.634 | 1.289 | 0.201 | -57.922 | -70.993 |
| Duration of ventilation | -0.593 | 2.513 | -0.236 | 0.814 | -5.600 | 4.414 |
| Duration of stay | 0.359 | 1.957 | 0.184 | 0.855 | -3.539 | 4.258 |
| Outcome | 10.178 | 0.137 | 3.120 | 0.004 | -0.512 | -0.210 |
Table 5: Multiple regression analysis for 25-OH vitamin D level as regard to sepsis, onset, duration of ventilation and duration of stay and outcome.
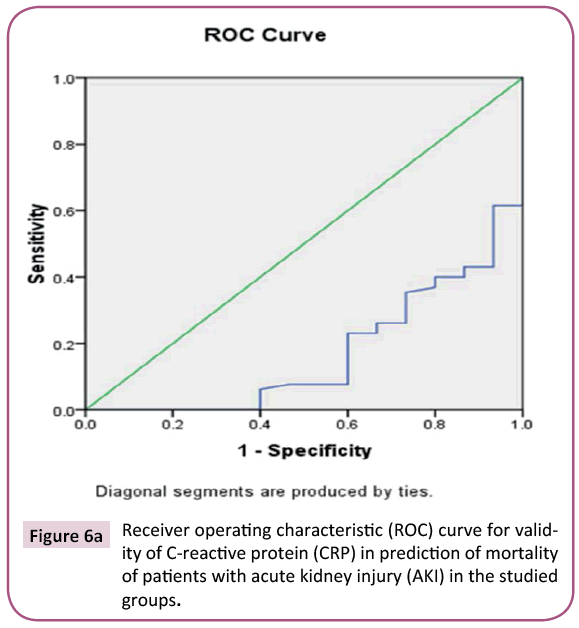
Figures 6a and 6b compares Receiver of Characteristics (ROC) curves for validity of CRP and 25(OH)D level respectively in prediction of mortality, CRP has 65 positive cases,15 negative cases, Area Under Curve(AUC) is 0.168. while 25(OH)D level has 15 positive cases,65 negative cases, Area Under Curve (AUC) is 0. 832 so ROC curves concluded that 25(OH)D level is more valid than CRP in prediction of mortality.
Discussion
The level of 25(OH)D needed for adequate immune and cardiovascular functions is still unclear. Vitamin D deficiency has been associated with increased viral respiratory infections and sepsis in children and adults [15].
Critically ill pediatric patients with AKI mostly have pre-renal aetiology and typically exhibit significantly lower diastolic blood pressure and albumin levels compared to the general population. The mechanism underlying such dramatic loss of binding proteins is still unknown, but it is thought to be related to interstitial extravasation from increased vascular permeability following inflammatory responses, decreased synthesis, and hemodilution during active resuscitation [16]. Vitamin D deficiency in AKI as a critical illness may therefore represent a state of mismatch between substrate supply and tissue requirement, so despite maximal stimulation of 1-alpha-hydroxylase by PTH, local tissue is unable to generate adequate 1,25(OH)2D. Variations in individual patient responses to acute stress in AKI may therefore depend on the degree of vitamin D insufficiency and extent of tissue requirement [16].
In our study, vitamin D deficiency occurs in about two third (66.25%) of studied patients versus about one third (33.75%) of studied controls. Hypovitaminosis D on hospital admission of our studied patients were 32.5% for severely deficient vitamin D (<30 nmol/L) and 33.75% for insufficient level (level between 30-75 nmol/L). This seems close to the prevalence of hypovitaminosis D in study by Rippel et al. in 316 general and cardiac PICU children in Australia, where the level of 25(OH)D was <50 nmol/ L in 34.5% [17]. Our results are in agreement with a study of Madden et al. who reported that 40.1% of their studied PICU patients were 25(OH)D deficient (level < 50 nmol/L) [15]. In another Spanish study, 29.5% of the PICU patients had 25(OH)D <20 ng/mL [18]. On other side, prevalence of 25(OH)D in the current study was less than that in a study by McNally et al. in Canadian PICU children where 25(OH)D level <50 nmol/L was in 69%, and 25(OH)D level between 50 to 75 nmol/L was in 23% [9].
This study included 80 patients 46 (57.5%) males and 34 (42.5%) females. No difference in sex distribution between the studied patients and controls
The studied patients with AKI resulted from five main diagnostic categories including respiratory (50%), cardiovascular (18.75%), metabolic (13.75%), neurological (10%), and hematological (7.5%). It is noticed that this current study includes PICU population of medical type rather than surgical. This is in accordance with Madden et al. in which 70% of studied patients had pre-kidney causes of AKI and 4.5% of studied patients are surgical. 15. In comparison with other studies e. g. McNally et al., most of their patients are surgical [9].
Our results reported no association between vitamin D deficiency and weight or height for age. While in study of McNally et al., higher weight for age ratios were associated with lower 25(OH)D [9].
In this study we found that, the medical history of the illness either acute or acute on top of chronic illness not significantly affect the level of vitamin D (p-value >0.05) and this is in agreement with McNally et al. and Madden et al. who found that there was no association between vitamin D deficiency and pre-existing illness. 9.15. On the other hand, another study found that patients with underlying disease had lower levels of 25(OH)D, these patients are at a higher risk for reduced vitamin D levels through abnormal diets, altered metabolism, or reduced environmental exposure [18].
It has been previously hypothesized that inadequate vitamin D status might predispose to or worsen critical illness pathophysiology. This study on critically ill children with AKI assessed the severity of critical illness on admission using PRISM III score which showed no difference between studied subgroups ( its median was 9.5 for seriously deficient, 9.5 for insufficient and 9 for sufficient vitamin D groups). This result is in agreement with McNally et al. who reported that PRISM III median value was 6 for the whole study group [9] Rey et al. who reported that PRISM III mean was 3.71 for vitamin D deficient group and 3.34 for vitamin D sufficient group [18] and Rippel et al. who reported that no association between vitamin D status and predicted PRISM III [17]. Our results are not in agreement with Madden et al. who reported that 25(OH)D levels at admission were inversely associated with PRISM III in North American children [15] Madden et al., and McNally et al. also reported that each additional PRISM unit increased the odds of being vitamin D deficient by 8% [9].
In this study we found that there is a significant correlation between sepsis and vitamin D deficiency (P-value<0. 05), in agreement with Van den Berghe et al. [19], but wasn’t in agreement with Madden et al. did not find critically ill children with confirmed or suspected infections to have lower 25(OH)D levels than other critically ill patient groups, with the exception of children presenting in severe septic shock [15].
This study included 20 (25%) ventilated children out of 80 patients, 35% of them are vitamin D sufficient, 30% are deficient and 35% are seriously deficient. All previously published studies found no relation between mechanical ventilation and vitamin D deficiency [9,17,18]. The present study did not observe an association neither between vitamin D status and duration of mechanical ventilation nor between vitamin D status and ICU admission duration. Rey et al., proved that duration of mechanical or non-invasive ventilation and length of PICU stay did not show differences between low and normal 25(OH)D groups [18]. Our data are also in agreement with that observed by Rippel et al. [17]. Rippel et al., in Australian children. However, McNally et al. found an association of vitamin D deficiency with longer length of stay. When the PICU length of stay multivariate analysis was performed with 25(OH)D as a continuous variable, every 10 nmol/L decrease was associated with 0. 44 additional days (P value=0. 048).
In this study, the median level of 25(OH)D is 59. 3 nmol/L and range is 10-388. 4 nmol/L. This is in accordance with a study by Ripple et al. in Australia [17]. A study by McNally et al. in Canadian PICU children [9]. While in a study of Madden et al. in North American PICU children, the median 25(OH)D level was lower than our results( 22. 5 ng/mL) [15].
In the present study, there is a significant negative correlation between 25(OH)D levels and age of the studied children. The median age was two years and sex months for the seriously deficient, one year for the insufficient and ten months for the sufficient cases (p- value <0. 05). These results are in agreement with Madden et al. who found that vitamin D level was lower in the older age group [15] and also in agreement with Rey et al. who concluded that incidence of vitamin D deficiency increased with age in their studied patients and controls and reported also that their PICU patients had double the incidence of hypo-vitaminosis D in all age groups and the differences were statistically significant [18].
The present study observes a significant negative correlation between vitamin D level and death probability. No relation was found between vitamin D status and survival outcome in study of McNally et al. [19].
In the current study, there was significant positive correlation between vitamin D level and total calcium level. This result is in agreement with McNally et al. and Rippel et al. [9,17].
In addition, this study demonstrates a relationship between number of organ system failure and the outcome, where death probability increases with multiple organ system failure rather than single system failure. In agreement with a study in Brazil which reported that multiple organ system failure (MOSF) was the main cause of death in 53% of patients [20]. Also in an Australasian study, MOF was the cause of death in 20. 3% of patients admitted to the ICU with severe non-infectious systemic inflammatory response syndrome and in 69% of patients with severe sepsis [21]. MOSF has recently been shown to be the main cause of morbidity and mortality in patients admitted to ICUs, and has been calculated to account for up to 80% of ICU deaths [20].
Patients who died had statistically significant worse severity scores (PRISM III) than those survived in this study and this matches the results of a study in Greece on PICU patients in which the higher the PRISM III score was, the worse the mortality rate became [22].
Sepsis in the current study is strongly related to death outcome since 91.18% of patients without sepsis were discharged, while 52.17% of septic patients died, supporting the study in by Khan et al. which detected high mortality rate in the presence of sepsis in their study population in a tertiary care PICU in Pakistan [23].
Conclusion
Incidence of vitamin D deficiency was high in critically ill pediatric patients with AKI especially those with older age. Vitamin D deficiency was associated with higher incidence of sepsis and mortality.
Recommendations
Sufficient vitamin D status in critically ill infants and children with AKI is essential for decreasing liability for sepsis improving disease outcome.
Acknowledgment
I would like to thank my colleagues and parents of my studied subjects in PICU of TUH, for their wonderful cooperation.
References
- Bailey D, Phan V, Litalien C (2007) Risk factors of acute renal failure in critically ill children:A prospective descriptive epidemiological study. PediatrCrit Care Med 8: 29-35
- Plotz FB, Hulst HE, Twist JW (2005) Effect of acute renal failure on outcome in children with severe septic shock. PediatrNephrol 20: 1177-1181.
- Akcan-Arikan A, Zappitelli M, Loftis LL (2007) Modified RIFLE criteria in critically ill children with AKI. Kidney Int 72:1028-1035.
- Goldstein SL, Currier H, Graf JM (2001) Outcome in children receiving continousvenovenous hemofiltration. Pediatrics 107: 1309-1312.
- Lowrie LH (2000) Renal replacement therapies in pediatric multi-organ dysfunction syndrome. PediatrNephrol 14: 6-12.
- Goldstein SL, Somers MJG, Baum MA (2005) Pediatric patients with multi-organ dysfunction receiving continuous renal replacement therapy. Kidney Int 67: 653-658.
- Foland JA, Fortenberry JD, Warshaw BL (2004) Fluid overload before continoushemofilteration and survival in critically ill children:A retrospective analysis.Crit Care Med 32:1771-1776.
- Venkatram S, Chilimuri S, Adrish M, Salako A (2011) Vitamin D deficiency is associated with mortality in the medical intensive care unit. Crit Care 15:R292.
- McNally JD, Menon K, Chakraborty P, Fisher L, Williams KA, et al. (2012) The association of vitamin D status with pediatric critical illness. Pediatrics 130: 429-436.
- Arnson Y, Gringauz I, Itzhaky D, Amital H (2012) Vitamin D deficiency is associated with poor outcomes and increased mortality in severely ill patients. QJM 105: 633-639.
- Mehta RL, Kellum JA, Shah SV (2007) AKIN:Report of an initiative to improve outcomes in AKI.Crit Care 11:R31.
- Castro RA, Angus DC, Hong SY, Lee C, Weissfeld LA, et al. (2012) Light and the outcome of the critically ill: an observational cohort study. Crit Care 16: R132.
- Acharya SP, Pradhan B, Marhatta MN (2007) Application of the sequential organ failure assessment (SOFA) scores in predicting outcome in ICU patients with SIRS. Kathmandu Univ Med J 5: 475-483.
- Khothari CR (2012) Research methodology, methods and techniques. (2nd edn). New Age International, New Delhi, p: 95-97.
- Madden K, Feldman HA, Smith EM, Gordon CM, Keisling SM, et al. (2012) Vitamin D deficiency in critically ill children. Pediatrics 130: 421-428.
- Quraishi SA, Camargo CA (2012) Vitamin D in acute stress and critical illness. CurrOpinClinNutrMetab Care 15: 625-634.
- Rippel C, South M, Butt WW, Shekerdemian LS (2012) Vitamin D status in critically ill children. Intensive Care Med 38: 2055-2062.
- Rey C, Sánchez-Arango D, López-Herce J, Martínez-Camblor P, García-Hernández I, et al. (2013) Vitamin D deficiency at pediatric intensive care admission. J Pediatr Rio J.
- Van den Berghe G, Van Roosbroeck D, Vanhove P, Wouters PJ, De Pourcq L, et al. (2003) Bone turnover in prolonged critical illness: Effect of vitamin D. J ClinEndocrinolMetab 88: 4623-4632.
- Lobo SM, Rezende E, Knibel MF, Silva NB, Páramo JA, et al. (2011) Early determinants of death due to multiple organ failure afternoncardiac surgery in high-risk patients. AnesthAnalg 112: 877-883.
- Dulhunty JM, Lipman J, Finfer S (2008) Does severe non-infectious SIRS differ from severe sepsis? Results from a multi-centre Australian and New Zealand intensive care unit study. Intensive Care Med 34: 1654-1661
- Volakli E, Sdougka M, Tamiolaki M, Tsonidis C, Reizoglou M, et al. (2011) Demographic profile and outcome analysis of pediatric intensive care patients. Hippokratia 15: 316-322.
- Khan MR, Maheshwari PK, Masood K, Qamar FN, Haque AU (2012) Epidemiology and outcome of sepsis in a tertiary care PICU of Pakistan. Indian J Pediatr 79: 1454-1458.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences