Non-Invasive Ventilation and Its Potential Misuse in End of Life Care
Ankur Sinha1*, Sushilkumar Satish Gupta1 and Yizhak Kupfer2
1Departments of Internal Medicine, Maimonides Medical Center, Brooklyn, NY, USA
2Divisions of Pulmonary Disease and Critical Care Medicine, Maimonides Medical Center, Brooklyn, NY, USA
- *Corresponding Author:
- Ankur Sinha
Department of Internal Medicine, 4802 10th Avenue
Brooklyn, NY 11219, USA
Tel: 267-916-7785
E-mail: ansinha@maimonidesmed.org
Received date: May 16, 2017; Accepted date: May 25, 2017; Published date: May 31, 2017
Citation: Sinha A, Gupta SS, Kupfer Y. Non- Invasive Ventilation and Its Potential Misuse in End of Life Care. J Clin Med Ther. 2017, 2:2.
Abstract
Non-invasive Ventilation (NIV) has undergone radical transformations over the past decades since its inception, when it was used to aid patients suffering from Duchene muscular dystrophy. There have been significant improvements in this technique making it possible to deliver safe and reliable ventilation to patient with a myriad of respiratory illnesses. We aim to illustrate that chronic use of NIV can lead to significant morbidity and poor quality of life.
Introduction
Non-invasive Ventilation (NIV) can be defined as a modality that supports breathing without the need of endotracheal intubation or placement of a surgical airway like tracheostomy. With an exponential growth in both the availability and functionality of the devices that deliver NIV, the onus of patient selection and humane delivery of therapy falls on the physicians.
The international consensus conference in intensive care medicine held in 2000, aimed to reach a common ground and enhance guidelines for NIV. The conference gave crisp and concise recommendations for indications, patient selection, rationale for therapy, equipment and modes of ventilation, and setup required to safely deliver NIV. The consensus states that the goals of NIV vary depending on the clinical scenario, and some of the salient features of their recommendations have been summarized in the Table 1.
| Indications of NIV | Rationale |
|---|---|
| 1. Acute asthma and COPD exacerbations | • Offloading the respiratory muscles |
| • Improved alveolar ventilation | |
| • Stabilization of arterial pH | |
| 2. Chronic ventilatory failure | • Reversal of atelectasis |
| • Resting the respiratory muscles | |
| • Elimination of CO2 | |
| 3. Obesity hypoventilation syndrome | • Maintaining airway patency |
| • Increasing lung volume | |
| • Augmenting alveolar ventilation | |
| 4. Cardiogenic pulmonary edema | • Improves cardiac output |
| • Reduces work of breathing and improving oxygenation | |
| 5. Weaning from endotracheal intubation | • Significant decrease in the period of endotracheal intubation |
| 6. Patients on Do Not Intubate status | • Supports the patient giving a chance to reverse short term causes of acute respiratory failure |
Table 1: Summarizing the indications for non-invasive ventilation as per the International consensus conference in intensive care medicine held in 2000.
When NIV is instituted for the correct candidates, it offers a clear advantage over endotracheal intubation. The various positive features have been summarized in the Table 2.
| Advantages of NIV over ET Intubation | |
|---|---|
| 1. Increased risk of infection in ET Intubation | • ET Intubation bypasses the mechanical defense of the upper airway predisposing to ventilator associated pneumonia |
| • Creates a pocket of secretions from the upper airway between the vocal cords and the ET tube cuff | |
| 2. Localized trauma | • Trauma to the structures of the oral cavity, as well as the upper airway during intubation |
| • Long term intubation leading to ulceration of the respiratory tract | |
| • Bleeding from the respiratory tract | |
| • Vocal Cord palsy | |
| 3. Requirement of sedation | • Complications related to sedation like hypotension as well as electrolyte abnormalities. |
| 4. Prolonged hospital course | • Prolonged ICU stay |
| • Poor patient experience | |
| • Deconditioning requiring pulmonary rehabilitation | |
Table 2: Summarizing the advantages of non-invasive ventilation over endotracheal intubation.
Limitations and Complications
While the advantages of NIV are abundant, there are certain limitations as well as complications which should be borne in mind while initiating therapy.
Appropriate Setup
NIV should be implemented only when the staff is well versed with the equipment and adequately trained in its management. This is because successfully delivering NIV therapy is complex. Specific requirements include monitored divisions such as the Intensive Care Unit (ICU), High Dependency Unit (HDU), or the Pulmonary Care Unit (PCU). Provision for escalating therapy to endotracheal intubation must be available in case of failure of NIV. Patients needing NIV should not be managed on regular medical floors.
Air Seal and Pressure
NIV requires an airtight facial seal with the face straps tightly fastened. The mask should be an appropriate size to ensure a tight fit. A balance should be maintained between maintaining a tight air seal and avoiding pressure related complications to the skin.
NIV works on the principle of applying carefully maintained positive pressure via a face mask. The pressure has to be titrated to maintain patency of the airway while avoiding barotrauma to the respiratory tree. Discomfort, dryness, ear and sinus pain, gastric insufflation are common complications. Severe complications such as pneumothorax [1] and pneumocephalus [2] although rare, are known to occur.
Mucus Plugging and Aspiration
NIV lacks the airway protective effect of ET intubation and patients with altered mental status are not ideal candidates for NIV. Severe complications like aspiration of regurgitated gastric contents as well as inspissation of secretions to form mucus plugs may occur leading to significant morbidity and mortality.
Skin Care
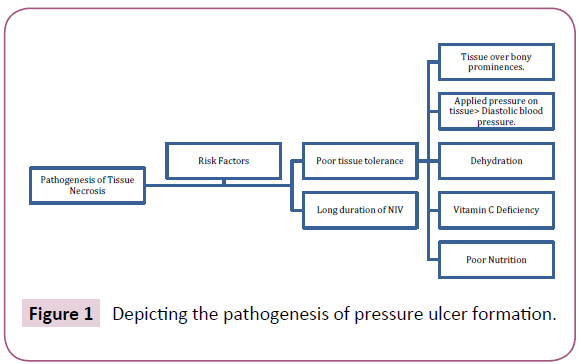
Vigilant observation for skin and tissue changes like skin rash, excoriations, pressure ulcers, and skin necrosis is necessary. A prospective observational study [3] looked at the pressure effects of various face masks. The nasal bridge was most prone to pressure ulcers due to relatively low underlying subcutaneous tissue. This study mentions that normal tissue will have an inherent auto-regulatory mechanism to counter pressure known as tissue tolerance [4]. Vasodilation and redistribution of external pressure is protective as well [5]. Figure 1 shows a detailed schematic of the pathogenesis of pressure ulcers in general.
Figure 1: Depicting the pathogenesis of pressure ulcer formation.
Potential Hazard
In order to counter the pressure related complications of NIV, several devices have been formulated to off load the pressure on the nasal bridge. These include gel inserts to redistribute pressure evenly on the mask-skin interface, as well as protective creams with a soothing effect to the excoriated skin. We report a potential hazard associated with the concomitant use of these gel-inserts with the protective creams. The inserts have an adhesive surface which reinforces its hold over the nasal bridge. We tested the hold of the several inserts on skin with the adhesive surface placed with and without a protective cream. The presence of cream severely hampers the adhesive quality of the gel inserts. A scenario where the gel insert slips into the oral cavity with the NIV apparatus actively applying positive pressure may have catastrophic results. The insert has the potential of blocking the airway at several levels including the glottis leading to serious complications including death.
Ethical Issues
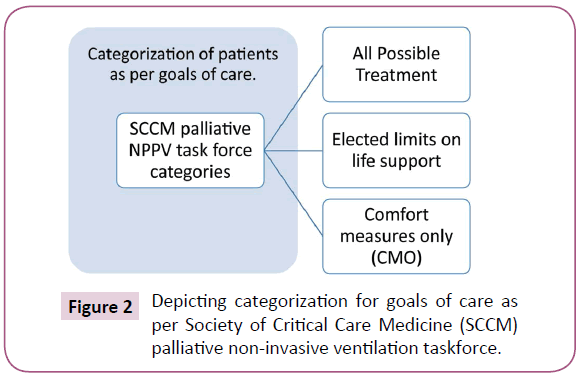
Patients with indications for respiratory support should be categorised appropriately to have a clear idea of the goals of care. A representative categorizatuon as per Society of Critical Care Medicine (SCCM) palliaive NIV taskforce has been depicted in Figure 2.
NIV can be suitable modus operandi in patients with acute respiratory distress who have chosen to receive all possible treatment, but its use in patients with advanced diseases and comfort measures only (CMO) status should be after a full consideration of goals of care, both immediate and short term. Quill and Brody [6] referred to an interesting concept of ‘Bad Death’ whereas Steinhauser [7] studied the idea of ‘Good Death’ amongst terminally ill cancer patients. We have summarized these concepts in Table 3.
| Table summarizing the concept of ‘Good vs. Bad Death’ | |
|---|---|
| Good Death | Bad Death |
| 1. Patient autonomy is maintained | 1. No opportunity to plan ahead |
| 2. Patient has predetermined clinical decisions | 2. No advanced treatment decisions |
| 3. Patient can achieve closure in personal relations | 3. The individual is unable to put personal affairs in order |
| 4. The family gets to bid an appropriate farewell | 4. Sudden as well as unexpected deterioration of condition with sudden death |
| 5. No burden on family | 5. Family is burdened with financial and legal matters |
| 6. Short and comfortable end of life care | 6. Painful and un-necessary procedures with no benefits in final outcome |
| 7. Disfigurement of body | |
Table 3: Summary of the concept of ‘Good Death’ vs. ‘Bad Death’.
The physicians should make sure that these issues are addressed while the patient has the capacity to make end of life decisions. The primary care providers should form a relation of trust with their patients and commit to the fulfilment of their patient’s wishes. The facts should be presented in non-medical terminology, and the physicians should ensure that all questions are addressed. The discussion should focus on the maintenance of a doctor-patient relationship, while offering help and support regardless of the selected level of care.
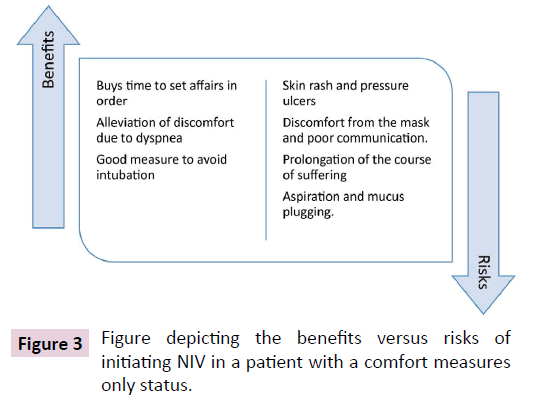
Quite often in our practice we come across situations when a patient loses capacity and a next of kin is called upon to make decisions. The relatives and health care surrogates should be making the decisions in line with the patient’s wishes, rather than guilt, or personal opinions. Decisions about initiating NIV in DNR/ DNI and patients with CMO orders continue to be a challenge, and the final outcome of the disease should be kept in mind. Figure 3 depicts the benefits vs risk of initiating NIV in a CMO patient and they should be weighed before initiating therapy.
Conclusion
NIV is a useful measure that can help patients transition from endotracheal intubation with mechanical ventilation to spontaneous breathing. It can also be used in patients with Do Not Intubate (DNI) status to buy time to get the patient’s affairs in order. Long term, continuous use of NIV involves significant morbidity and should be avoided. The risks of therapy should be weighed against its benefits and a decision should be made respecting the patient’s wishes. Frequent discussions should be made with the patients and their families, and a plan with the final goals of care should be formulated.
References
- Simonds AK (2004) Pneumothorax: an important complication of non-invasive ventilation in neuromuscular disease. Neuromuscular Disord 14: 351-352.
- Nair SR, Henry MT (2005) Pneumocephalus induced by non-invasive ventilation: A case report. Resp Med Extra 1: 75-77.
- Munckton K, Ho KM, Dobb GJ, Das-Gupta M, Webb SA (2007) The pressure effects of facemasks during noninvasive ventilation: a volunteer study. Anaesthesia 62: 1126-1131.
- Defloor T (1999) The risk of pressure sores: a conceptual scheme. J Clin Nurs 8: 206-216.
- Kosiak M (1961) Etiology of decubitus ulcers. Arch Phys Med Rehabil 42: 19-29.
- Quill TE (1995) You promised me I wouldn't die like this!' A bad death as a medical emergency. Arch Intern Med 155: 1250-254.
- Steinhauser KE (2000) In search of a good death: observations of patients, families, and providers. Ann Intern Med 132: 825.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences