Massive Internal Hemorrhoid Bleeding in a Patient Taking Antiplatelet Therapy: A Risky Rectal Swab
Pavel Fedarenchik*, Saleem Abu Rajab and Sofia Rimbrot
Department of Internal Medicine A, HaEmek Medical Center, Afula, Israel
- *Corresponding Author:
- Pavel Fedarenchik
Department of Internal Medicine,
HaEmek Medical Center, Afula,
Israel,
E-mail: Pavells.f@gmail.com
Received date: March 03, 2024, Manuscript No. IPIJCR-24-18702; Editor assigned date: March 06, 2024, PreQC No. IPIJCR-24-18702 (PQ); Reviewed date: March 20, 2024, QC No. IPIJCR-24-18702; Revised date: March 27, 2024, Manuscript No. IPIJCR-24-18702 (R); Published date: April 03, 2024, DOI: 10.36648/ipijcr.8.1.07
Citation: Fedarenchik P, Rajab SA, Rimbrot S (2024) Massive Internal Hemorrhoid Bleeding in a Patient Taking Antiplatelet Therapy: A Risky Rectal Swab. Int J Case Rep Vol.8 No.1: 07.
Abstract
Lower Gastrointestinal (GI) bleeding due to internal hemorrhoids is a common nuance, usually causing mild bleeding. Massive GI bleeding usually occurs as a complication of surgical procedure, or due to rectal mucosa physical damage and coagulopathy. A 66-year-old male without prior history of bleeding, under dual anti-platelet therapy suffered massive lower GI bleeding after rectal Carbapenem- Resistant Enterobacterales (CRE) swab self-collection. He was rushed to intervention angiography for arterial embolization of the superior rectal artery. During the bleeding he required red blood cells and platelets transfusion. A follow up check after discharge revealed internal hemorrhoids, which were the probable cause of the bleeding.
Keywords
Rectal bleeding; DAPT; Rectal swab; Lower GI bleeding
Introduction
Internal hemorrhoids are a prevalent occurrence with a significant impact on quality of life, primarily due to bleeding associated with bowel movement. Massive lower gastrointestinal bleeding due to internal hemorrhoids is rare and occurs usually as complication of surgical intervention. Patients with coagulopathy such as anticoagulation therapy or vascular malformations are at risk of massive hemorrhage with lesser degree of physical insult to the rectal mucosa [1,2]. Here we describe a case of severe internal hemorrhoid bleeding initiated after rectal swab was collected by a Q-tip, aggravated by antiplatelet therapy.
Case Report
A 66-year-old male with a history of smoking, hypertension, dyslipidemia and stage 3 chronic kidney disease, presented at the Emergency Department. For the past year, he had been taking Dual Antiplatelet Therapy (DAPT) including aspirin and effient, due to Percutaneous Coronary Intervention (PCI) and Drug- Eluting Stent (DES) implantation in the Left Anterior Descending Artery (LAD). He was admitted to the hospital with exertional dyspnea and chest tightness, without any other complains or signs of gastrointestinal bleeding.
On admission he was hypertensive, with systolic blood pressure around 200, while the rest of the vital signs were normal. His physical exam, as well as, the Electrocardiogram (ECG), chest X-ray and laboratory test were unremarkable. The patient was hospitalized for high blood pressure management and observation. He was asked to undergo a rectal swab test for Carbapenem-Resistant Enterobacterales (CRE) screening, as part of a standard protocol. The nurse instructed him to collect a stool sample using the soft Q-tip of the swab and return it to the nurse’s station.
The stool sample was collected and returned to the nurse by the patient without any incidents. About an hour later, the attending physician was called to see the patient. He had serious rectal bleeding, the hind parts of the pant was soaking with blood, as well as the bed that the patient was sitting on. The attending physician called the attending surgeon to assess the patient’s condition. During the time until the surgeon’s arrived the patient became diaphoretic, with blood pressure dropping to 150 systolic.
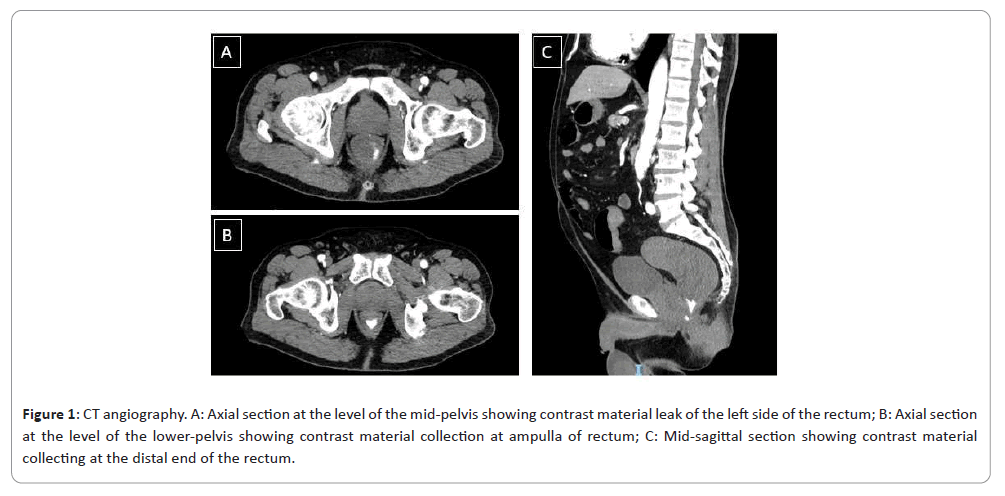
The surgeon was unable to spot the source of bleeding due to active bleeding and blood cloths blocking the visual field of the rectoscope. In order to achieve homeostasis, a gelfoam was inserted into the rectal ampulla, but due to the continuing worsening of vital signs, the patient was rushed to CT Angiography (CTA). The CTA confirmed active bleeding at the rectum, with collection of blood at the ampulla of the rectum. The exact vessel involved was not spotted but the most probable candidate was one of the superior rectal vessel branches (Figure 1).
Figure 1: CT angiography. A: Axial section at the level of the mid-pelvis showing contrast material leak of the left side of the rectum; B: Axial section at the level of the lower-pelvis showing contrast material collection at ampulla of rectum; C: Mid-sagittal section showing contrast material collecting at the distal end of the rectum.
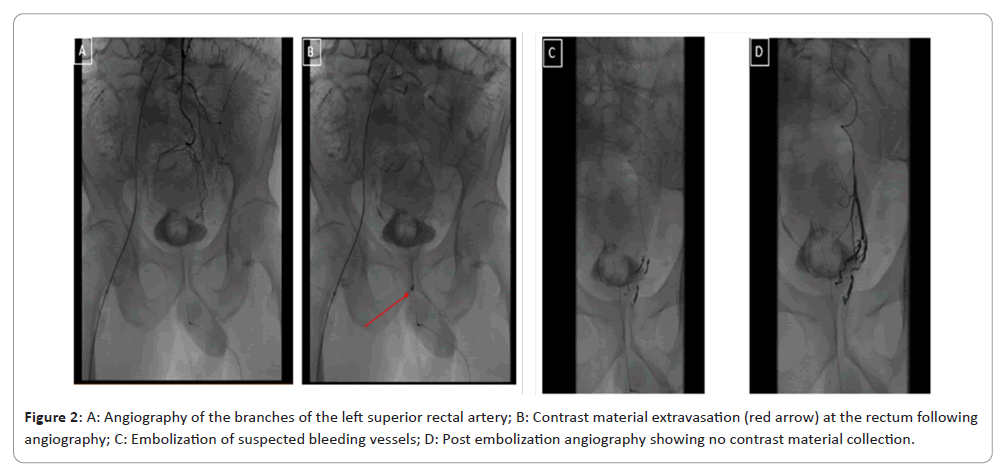
The patient was then rushed to interventional angiography for embolization of the bleeding artery. The angiography was performed using the right femoral artery for catheterization, inspecting the inferior mesenteric and then the superior rectal arteries. Contrast material extravasation was seen at one of the branches of the left superior rectal artery, which was successfully embolized (Figure 2).
Before and during the agio-embolization the patient received 1-unit red blood cells and 5 units platelets. After the procedure, the patient’s vital signs normalized and no more active bleeding was visible. At follow up questioning of the patient after this incident, he stated that he didn’t feel any pain during the rectal swab collection, he did not see any blood on the swab after he was done and overall felt normal after he delivered the swab back to the nurse. His baseline hemoglobin of 14 g/dL dropped to 11.2 g/dL during the active phase of the bleeding and stabilized at 8.9 g/dL at discharge, two days later. During his hospitalization he received iron transfusion to replenish his iron storage. He was discharged with recommendation to adhere to the blood pressure lowering therapy, repeat complete blood count test and resume aspirin treatment after 1 week and ceases treatment with effient.
One week after discharge, the patient had a follow up visit to the surgeon. Physical exam revealed small single external hemorrhoid and on anoscope exam, several small internal hemorrhoids without signs of bleeding.
Results and Discussion
Internal hemorrhoids are dilated submucosal blood vessels located above the dentate line. About 40% of people with internal hemorrhoids are asymptomatic, while the most common symptom is Lower Gastrointestinal (GI) bleeding associated with bowel movement or strenuous toilet activity. The bleeding is almost always painless and presents as bright red bleeding [3,4]. Hemorrhoid bleeding accounts for about 6%-16% of lower GI bleeding and is usually minor [5]. Massive hemorrhoid hemorrhage can develop under two main conditions: A mechanical insult to the area such ano-rectal instruments insertion, digital exam, or fecal impaction, since the hemorrhoids can be easily injured and a coagulopathic state, such as taking anti-coagulation or antiplatelet therapy.
The patient discussed in the case report had no prior history of rectal bleeding or any gastrointestinal complaints except reflux due to Helicobacter pylori infection 5 years ago. He developed a painless massive lower GI bleeding, without any predisposing activity except the rectal CRE swab stool collection, aggravated by anti-platelet therapy.
A case series of eight cases by Ozdil et al. presents cases of massive internal hemorrhoid bleeding in elderly patients taking anticoagulation [1]. All of the patients reported had either fecal impaction or recent rectal interventions due to constipations, which apparently served as an insulting factor to the rectal mucosa and hemorrhoids. Unlike the case series patients mentioned above, the patient we present had no rectal insulting factor except the CRE Q-tip stool collection, which hardly can seriously irritate the hemorrhoids.
A case report by Kim et al. describes a massive lower GI bleeding due to Dieulafoy lesion of the rectal arteries and pseudoaneurysms of the superior mesenteric artery, in a patient treated with clopidogrel due to recent CVA [2]. The patient described in this case report had a vascular malformation as a predisposing factor for massive bleeding, unlike the patient we are presenting here. The patient’s bleeding was controlled using angio-embolization.
Recent works showed the efficiency of embolization of the superior rectal artery or its branches in treatment of internal hemorrhoids bleeding [6,7]. During the angio-embolization the radiologist speculated that the radiography picture resembled the procedure mentioned above and could potentially be an internal hemorrhoidal bleeding.
As reflected in the case we are presenting and the cases mentioned above, a massive bleeding originated from internal hemorrhoids usually requires two conditions: Trauma or insults leading to initial bleeding and a coagulopathy usually due to medication, as an aggravating factor. We speculate that the patient inadvertently irritated one of the internal hemorrhoids when he was inserting the rectal swab, causing it some degree of injury and later on causing it to bleed and due to anti-platelet therapy the bleeding became serious, requiring urgent intervention and blood transfusions.
Conclusion
We would like to stress the importance that rectal swab should be collected by a healthcare provider, which can see any potential problems like external lesions or hemorrhoids and avoid insulting them. Also, any rectal exam should consider the possibility of occult internal hemorrhoids, that when combined with antiplatelet or anti-coagulation therapy could result in serious, albeit rare, bleeding.
References
- Ozdil B, Akkiz H, Sandikci M, Kece C, Cosar A (2010) Massive lower gastrointestinal hemorrhage secondary to rectal hemorrhoids in elderly patients receiving anticoagulant therapy: Case series. Dig Dis Sci 55: 2693-2694.
[Crossref], [Google Scholar], [Indexed]
- Kim M, Song HJ, Kim S, Cho YK, Kim HU, et al. (2012) Massive life-threatening lower gastrointestinal hemorrhage caused by an internal hemorrhoid in a patient receiving antiplatelet therapy: A case report. Korean J Gastroenterol 60: 253-257.
[Crossref], [Google Scholar], [Indexed]
- Soeseno SW, Wahyudi PAE, Febyan F (2021) Diagnosis and management of internal hemorrhoids: A brief review. European Journal of Medical and Health Sciences 3: 1-5.
- Sun Z, Migaly J (2016) Review of hemorrhoid disease: Presentation and management. Clin Colon Rectal Surg 29: 22-29.
[Crossref], [Google Scholar], [Indexed]
- Bleday R, Breen E (2023) Hemorrhoids: Clinical manifestations and diagnosis.
- Sun X, Xu J, Zhang J, Jin Y, Chen Q (2018) Management of rectal bleeding due to internal haemorrhoids with arterial embolisation: A single-centre experience and protocol. Clin Radiol 73: 985.e1-985.e6.
[Crossref], [Google Scholar], [Indexed]
- Han X, Xia F, Chen G, Sheng Y, Wang W, et al. (2021) Superior rectal artery embolization for bleeding internal hemorrhoids. Tech Coloproctol 25: 75-80.
[Crossref], [Google Scholar], [Indexed]
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences