ISSN : 2393-8854
Global Journal of Research and Review
Lipochondromatous Pulmonary Hamartoma-A Case Report
1Assistant Professor, Department of Pathology, Chalmeda Anand Rao Institute of Medical Sceinces, Karimnagar, Telangana state, India
2Associate Professor, Department of Radiology, Chalmeda Anand Rao Institute of Medical Sceinces, Karimnagar, Telangana state, India
3Professor, Department of Surgery, Chalmeda Anand Rao Institute of Medical Sceinces, Karimnagar, Telangana state, India
4Post graduate, Department of Anaesthesia, Gandhi Medical College, Hyderabad, Telangana State, India
Abstract
Benign tumours of the tracheobronchial tree are very uncommon tumours. Hamartoma is the most common benign tumour of the lung. We herein report a case of Lipochondromatous pulmonary hamartoma in a 45 year old male patient.
Keywords
Pulmonary hamartoma, Benign, Adipose tissue, Cartilage.
Introduction
Benign tumors are very rare tumours of the lung and constitute less than 1% of all lung neoplasms. Hamartomas are the commonest benign tumours of the lung. The incidence ranges between 0.025%-0.32% [1]. They are situated commonly in the peripheral part of the lung and rarely in the endobronchial region. Patients with intrapulmonary lesion are usually asymptomatic and it is an incidental finding. The size of the tumour varies from 1 cm to 8 cm. Patients with endobronchial lesion are often symptomatic with fever, wheezing or hemoptysis [2].
We report a case of incidentally found pulmonary hamartoma in a 45 years old male patient.
Case Report
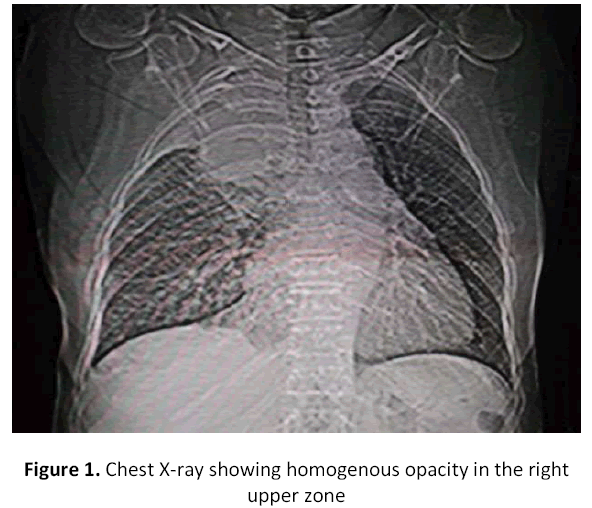
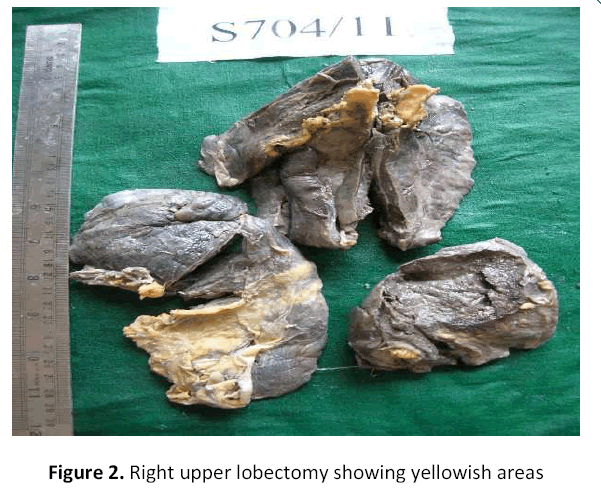
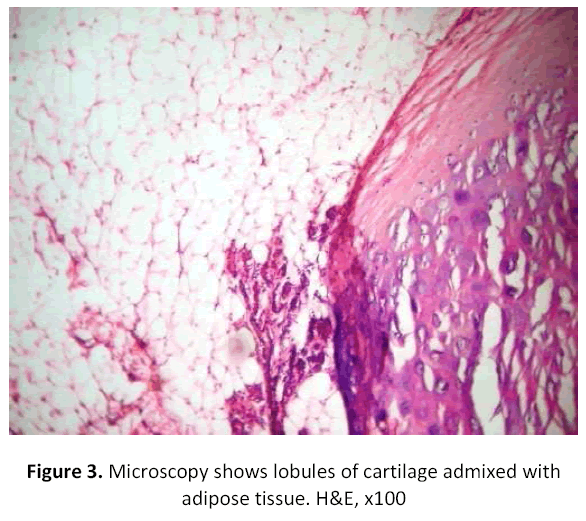
45 years old male patient, labourer by occupation presented with cough, chest pain, dyspnea for 3 months. There was no history of smoking, tuberculosis or weight loss. On examination, he was moderately built and moderately nourished .There was no cyanosis or clubbing. Respiratory system examination showed decreased respiratory sounds in the right lung. Chest x-ray showed a homogenous opacity in the right lung upper zone (figure-1). Bronchogenic carcinoma was suspected basing on clinical findings and chest X-ray and right upper lobectomy was done and sent for histopathological examination. Grossly, the tumour was 7.5x 6x 4cms, solid, lobular, yellowish to grey brown (figure-2). Microscopically, lobules of mature cartilage intimately admixed with mature adipose tissue interspersed by cleft like spaces are seen (figure-3). These spaces are lined by pseudostratified columnar epithelium. The pathological diagnosis of lipochondromatous hamartoma of right upper lobe of lung was made. After 3 years of follow up, the patient is healthy with no signs of recurrence. His chest x-ray showed complete resolution of the opacity.
Discussion
The term hamartoma was introduced by Albrecht in 1904 to describe a tumour like growths which were considered to be developmental anomalies [3]. Hamartomas are now considered as true neoplasms rather than developmental anomalies. Their rarity in childhood and appearance in adult life is strongly suggestive of a neoplastic lesion. Furthermore, several cytogenetic studies have identified recombination of chromosomal bands 6p21 and 14q24 supporting the neoplastic nature of the lesion [4]. Hamartomas are composed of an admixture of mesenchymal and epithelial elements like cartilage, bone, fat and fibrous tissues [5]. Basing on the varying histological components of the tumour, they have been called chondroma, osteochondroma, lipochondroma, lipo-osteochondroma and bronchioma. Hamartomas are divided into intraparenchymal and endobronchial types basing on the location of the lesion. Hamartomas present usually as intraparenchymal nodules in the peripheral part of the lung [6]. Typically, endobronchial hamartomas contain more fat than parenchymal hamartomas [7]. Our patient had an intrapulmonary hamartoma, predominantly composed of adipose tissue and cartilage.
Radiologically, hamartomas constitute 7-14% of pulmonary coin lesions [8]. They may show different patterns of calcification, including an irregular popcorn, stippled or curvilinear pattern or even a combination of all 3 patterns. However, the characteristic calcification is seen in only approximately 15% of the patients. Our patient also presented with opacity in the right upper zone without calcification on chest X-ray.
Since hamartomas are very difficult to distinguish from malignant neoplasms by nonsurgical techniques, surgical excision is indicated. Definite diagnosis can only be made by histological examination of the lesion. Today, even with the advancement in medical therapy, pulmonary resection remains the most important treatment of patients with pulmonary hamartomas. Pulmonary hamartomas are usually asymptomatic and show slow growth [9]. The pulmonary hamartoma has the tendency of expansion or recurrence and chronic inflammatory stimulation of lesion may contribute to the development of malignancy. Therefore, when a solitary pulmonary lesion is more than 2.5 cm or the possibility of malignancy cannot be excluded, surgical resection is to be done and should be mandatory [10].
Conclusion
Pulmonary hamartoma is a benign tumour with good prognosis and slow annual growth. Definite diagnosis can only be made by histological examination of the lesion. As pulmonary hamartomas are impossible to distinguish from malignant tumours by nonsurgical techniques, surgical excision is mandatory.
References
- Mondello B, Lentini S, Buda C, Monaco F, Familiari D, et al. Giant endobronchial hamartoma resected by fibreoptic bronchoscopy electrosurgical snaring. J Cardiothoac Surg. 6:2011:97.
- Murray J, Kielkowski D, Leimen G. The prevalence and age distribution of peripheral pulmonary hamartomas in adult males. An autopsy based study. S Afr Med J. 79:19:247-249.
- Albrecht E. Ueber Hamartoma. Verh Deutsch Ger Path. 7:1904:153.
- Lien YC, Hsu HS, LiwY, Wu PC, Hsu WH,et al. pulmonary hamartoma. J Clin Med Assoc. 67:2004:21-26.
- Lakhotia S, Dewan RK. Endobronchial lipomatous hamartoma: a rare cause of bronchial occlusion with destroyed lung. Indian Journal of Thoracic and Cardiovascular Surgery. 24; 2008:201-202.
- Simon M, Ballon LT. An unusual hamartoma. J Thorac. Surg. 16: 1947:379.
- Gaerte SC, Meyer CA, Winer Muram HT, Tarver RD, Concer DJ. Fat containing lesions of the chest. Radiographics. 22:2002:61-78.
- Wiatrowska BA, Yazdi HM, Matzinger FR, Mac Donald LL. Fine needle aspiration biopsy of pulmonary hamartomas. Radiologic Cytologic and Immuno- cytochemical study of 15 cases. Acta Cytol. 1995; 39:1167-74.
- J.A. Gjevre, J.L Myeres, U.B.S.Prakash. Pulmonary hamartomas. Mayo clinic proceedings. vol 71, no 1, 1996:14-20.
- Guo W, Zhao YP, Jiang YG, Wang RW, Ma Z. Surgical treatment and outcome of pulmonary hamartoma; a retrospective study of 20 year experience. J ExpClin Can Resp. 2008; 27:8.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences