Large Posterior Perforation of Duodenal Ulcer: A Rare Surgical Emergency
1Department of General Surgery, Dubai Hospital, Dubai, UAE
2Department of Radiology, Dubai Hospital, Dubai, UAE
- *Corresponding Author:
- Aliya Ishaq
Department of General Surgery, Dubai Hospital, Dubai, UAE
Tel: 00971501937655
E-mail: draliya_ishaq@yahoo.com/aishaq@dha.gov.ae
Received date: September 01, 2018; Accepted date: September 19, 2018; Published date: September 24, 2018
Citation: Ishaq A, Noureen S, Khan MJH, Awa AA, Ghazi EH, et al. (2018) Large Posterior Perforation of Duodenal Ulcer: A Rare Surgical Emergency. Int J Case Rep Vol 2:11.
Copyright: © 2018 Ishaq A, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
A 36-year-old previously healthy male presented to the emergency department with several hours history of sudden epigastric pain which increased gradually to become generalized causing findings of an acute surgical abdomen. His leukocyte counts and septic markers were elevated. A plain chest and abdominal X-ray showed no evidence of pneumoperitoneum or obstruction. Abdominal CT scan however, showed free air in the retroperitonium. After urgent resuscitation, the patient was taken for emergency laparotomy. This revealed a large posterior perforation extending laterally in the first part of duodenum. The duodenum was severely inflamed and the retroperitoneal space was contaminated with purulent discharge and debris. The abdomen was thoroughly irrigated with normal saline, and the patient underwent a Graham’s patch repair to the duodenal perforation, a gastrojejunostomy and insertion of a feeding jejunostomy tube. A closed tube drain was inserted to the right hypochondrium. No definitive repair procedure was performed to avoid prolonging operative time further and it was kept in mind that any further leak which was expected will be managed conservatively because of presence of purulent peritonitis as in such an abdomen any surgical intervention is going to cause more harm than good, so only damage control surgery was done. Post-operatively, the patient developed a high output duodenal fistula which was managed conservatively successfully. Complete closure of the fistula was confirmed by performing a gastrografin study. The patient was discharged home tolerating oral feed on the 35th postoperative day.
Keywords
Posterior duodenal perforation; Perforated duodenal ulcer; Duodenal fistula; Conservative management of duodenal fistula
Introduction
Perforated peptic ulcer is a surgical emergency and is associated with short-term mortality and morbidity in up to 30 and 50% [1] of patients, respectively. Worldwide variation in demography, socioeconomic status, Helicobacter pylori prevalence and prescription drugs make investigation into risk factors for perforated peptic ulcer difficult. Perforated peptic ulcer presents as an acute abdominal condition, with localized or generalized peritonitis and a high risk for developing sepsis and death [1].
Posterior perforation of gastro duodenal ulcers is a unique category of peptic ulcer perforations with a distinct clinical presentation [2]. While it is rare, awareness of this surgical emergency is important, as this condition is associated with a high morbidity and mortality. The diagnosis is commonly missed because of the indolent nature on the initial symptoms with catastrophic outcome [3]. Early surgery, either by laparoscopic or open repair and proper sepsis management is essential for good outcome. Selected patients can perhaps be managed non-operatively or with novel endoscopic approaches [4].
We report a case of a perforated large posterior duodenal ulcer which was repaired with an omental patch, gastrojejunostomy and feeding jejunostomy without pyloric exclusion.
Case Report
A previously healthy 36-year-old male presented to the emergency department at Dubai hospital with two days history of progressively worsening lower abdominal pain which became generalized later. The pain was associated with nausea, vomiting and absolute constipation. He was a smoker with no history of NSAIDS or steroid use, and no past surgical history. On examination, apart from tachycardia the rest of his vital signs were stable. His abdomen was distended with generalized tenderness with guarding, his bowel sounds were sluggish and per rectal examination was normal. Laboratory findings showed leukocytosis of 12700/μl and CRP>120 mg/L. All other laboratory parameters were within normal limits. Chest X-ray did not show any evidence of pneumoperitoneum. Abdominal CT scan showed free gas in the retro-peritoneum along with fat stranding. Emergency laparotomy was done and no free fluid found in peritoneal cavity, no perforation noted at the anterior wall of the stomach or duodenum. Duodenum and reteroperitoneal structures were looking unhealthy so the lesser sac opened and kocherization of duodenum was performed. Large amount of foul smelling pus was revealed in the retroperitonium along with necrotic slough and adhesions. There was a large perforation located on the posterior wall of the first part of the duodenum, and the entire lateral and posterior walls were badly scarred, calloused, inflamed and distorted. After adequate irrigation with warm normal saline, the perforation was repaired using an omental patch fixed with 3/0 PDS sutures. Retro-colic loop gastrojejunostomy was fashioned using GIA 60 side-side stapled anastomosis and a feeding tube jejunostomy was inserted 25 cm from the DJ flexure. Two abdominal drains were placed both in the lesser sac and pelvic cavity. The inflammation and scarring of the region was a major contribution to the decision not to perform any resection procedures as in the presence of purulent peritonitis any definitive and prolonged procedure would have done more harm than good so only damage control surgery was done and it was kept in mind that there are high chances of leak of grahm’s patch and in case of any leak the patient will be managed conservatively.
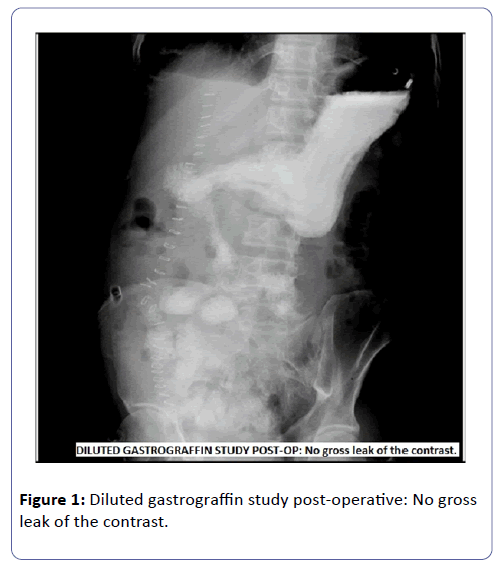
Post operatively, the patient was managed in ICU for 3-4 days but gradually improved and was transferred to the surgical ward. On the 2nd postoperative day, he developed a high output duodenal fistula draining around 750-1000 mL of bile in 24 h. He remained hemodynamically stable and all his laboratory parameters satisfactory. He was started on TPN along with other necessary nursing and wound care. Jejunostomy feed was started on the 9th post op day. Drain output gradually reduced to 20-30 mL daily after 5-6 weeks. Oral feeding commenced on week 7 after a gastrografin study (Figure 1) showed no evidence of leak after few days of nil drainage output. He received a full course of H pylori eradication treatment. The feeding Jejunostomy tube was blocked and eventually removed once the patient had tolerated full oral intake. The patient was discharged on 35th post-operative day, and was well and symptom free when reviewed in the surgical outpatient clinic on weeks 2, 4 and 12 post discharge.
Discussion
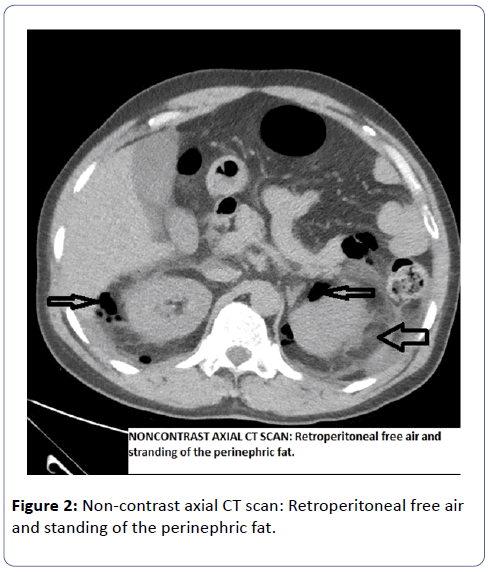
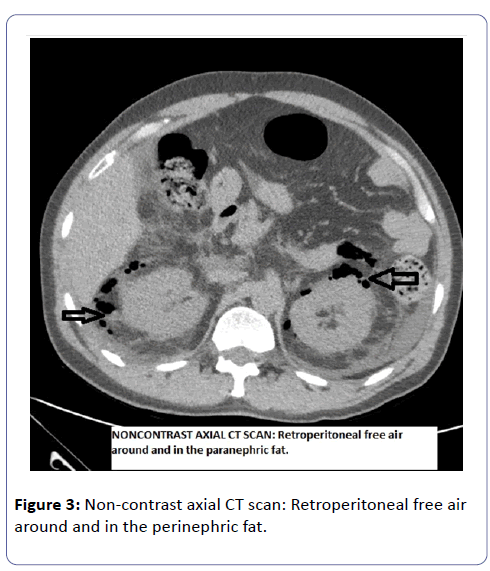
Posteriorly perforated pyloric or duodenal ulcers penetrate into the retroperitoneal space (Figure 2). This results in either retroperitoneal abscess formation, or a spontaneous sealing due to the local inflammatory reaction and fibrosis of the surrounding adherent retroperitoneal tissues (Figure 3). Delayed presentation is a characteristic of posterior perforations. These perforations are commonly missed on initial examination [5]. Routine chest and abdominal roentgenograms are invaluable for evaluation of patients with posterior perforations. Computed Tomography (CT) scanning has an important role in the diagnosis of perforated peptic ulcer and in the determination of the site of perforation. Particular findings on CT scanning that suggest posterior wall perforation are retro-duodenal air and/or fluid collection [6]. The giant saddle ulcer extending from the posterior duodenal wall superiorly and anteriorly usually perforates at its anterior edge near the porta hepatis.
Almost the entire circumference of the duodenum will need to be mobilized to secure pliable tissue for a pyloroplasty. When this dissection is complete, the proximal duodenum will usually have been transected in most of its circumference. Under these circumstances an antrectomy is the simpler procedure. A tube duodenostomy may be performed rather than to close the duodenal stump. However, In the presence of purulent peritonitis, the peritoneal cavity is drained externally [7]. Only purulent peritonitis is a contraindication to an ulcer definitive operation in a properly resuscitated and reasonable risk case with a chronic ulcer. With scar, callous and intense inflammatory reaction seromuscular sutures may cut through or plication would result in obstruction. Abutment with simple through and through chromic catgut sutures may be preferable [8]. Alternatively, the technique advocated by Roscoe Graham can be employed [9]. It consists of the placement of three through and through chromic catgut sutures well back from the edge of the perforation. A free graft of omentum is placed over the perforation itself. The sutures are tied loosely. The omentum acts as a plug and as stated by Graham, "An attempt is not made to actually close the perforation." When the pathology in the pyloroduodenal area is maximal, an attempt at closure by any of the above techniques may fail with high risk of re-perforation, obstruction or both. In the case of saddle ulcer of "kissing" ulcers hemorrhage may complicate the postoperative course.
Berne and Mikkelson in 1958 noted that closure with a badly diseased duodenum may be more safely achieved by pyloroplasty or antrectomy, with or without tube duodenostomy than by so called simple closure [10]. Based on retrospective reviews, a number of features were considered contraindications to definitive operations, including shock, old age, perforations of greater than 12 h duration, and peritoneal contamination [11]. In our case we did only omental patching with drainage of peritoneal cavity and secondary feeding route was made in the form of feeding jejunostomy and gastrojejunostomy made to drain the stomach contents. No attempt was made for pyloroplasty or other definitive procedures as the scarred duodenum associated with fibrosis would have resulted in increased morbidity had a definitive resection procedure been attempted.
The patient developed a high output fistula on the 2nd post op day which was due to partly or complete breakdown of the graham patch repair. As the patient was clinically, hemodynamically and biochemically doing well and was tolerating jejunostomy feed, we continued with the plan to manage the fistula conservatively and this subsequently closed. He did not show any signs of intra-abdominal sepsis.
Although the patient had a prolonged hospital stay which is expected in conservative management of controlled fistula, this conservative approach was considered the safest option taking into consideration the initial operative findings.
The patient had adequate nutritional support using TPN and jejunostomy feed with good monitoring of electrolyte and vitamin balance and replacement. The oral feeding also started at 6th week post op which did not initiate re-leakage and was fully tolerated.
Conclusion
Posterior perforations of duodenal ulcers have a high mortality. Delayed presentation due to insidious and non specific initial symptoms and missed diagnosis at laparotomy are major contributory factors. Posterior perforations if delayed are associated with peritonitis, sepsis, and multi-organ failure. In cases of purulent peritonitis, performing definitive surgical procedure is a contraindication and only damage controlled surgery should be performed. In the badly scarred and contracted duodenum the matter of both secure closure and adequate channel for gastric emptying must be considered. The attending surgeon responsible for the care of the individual case is free to select a form of therapy that differs from the standard protocol, if he/she considers such a selection to be in the best interest of the patient.
References
- Møller MH, Adamsen S, Thomsen RW (2011) Multicentre trial of a perioperative protocol to reduce mortality in patients with peptic ulcer perforation. Br J Surg 98: 802-810.
- Badawy AA (2016) A large posterior perforation of gastric ulcer: a rare surgical emergency. Egypt J Surgery 35: 74-76.
- Williams N, Bullstrode C, Connell RO (2010) Bailey and Love’s short practice of surgery, 25th ed. Ann R Coll Surg Engl 92: 178.
- Soreide K, Thorsen K, Harrison EM, Bingener J, Moller MH, et al. (2015) Perforated peptic ulcer. Lancet 386: 1288-1298.
- Wong CH, Chow PK, Ong HS, Chan WH, Khin LW, et al. (2004) Posterior Perforation of Gastric Ulcer. Surgery 49: 1882-1883.
- Chen CH, Huang HS, Yang CC, Yeh YH (2001) The features of perforated peptic ulcers in conventional computed tomography. Hepatogastroenterology 48: 1393–1396.
- Donovan AJ, vinson TL, Maulsby GO, Gevin JRB (1979) Selective Treatment of Duodenal Ulcer with Perforation. Ann Surg 89: 627-635.
- Berne CJ, Rosoff L (1977) Acute perforation of peptic ulcer. Br J Surg 64: 247-249.
- Piper CC, Yeo CJ, Cowan SW (2014) Roscoe Reid Graham (1890 to 1948): A Canadian pioneer in general surgery. Am Surg 80: 431-433.
- Berne CJ, Mikkelsen WP (1958) Management of Perforated Peptic Ulcer. Surgery 11: 591-603.
- Gray JG, Roberts AK (1976) Definitive emergency treatment of perforated duodenal ulcer. Surg Gynecol Obstet 143: 890894s.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences