ISSN : 2393-8854
Global Journal of Research and Review
Knowledge of Neonatal Danger Signs and its Determinant Factors among Mothers Attending Postnatal Care in Nekemte, Ethiopia, 2019: Cross Sectional Descriptive Study
Ayana Chimdessa1*, Italem Tamiru2, and Feyyissa Lemmessa3
1 Department of Nursing and Midwifery College of Medicine and Health Sciences, Ambo University, Ambo, Ethiopia
2 Department of Intensive Care Medicine, Bako Tibbe District hospital, Bako, Ethiopia
3 Department of Intensive Care Medicine,Bako Tibbe District hospital, Bako, Ethiopia
- *Corresponding Author:
- Ayana Chimdessa
Department of Nursing and Midwifery College of Medicine and Health Sciences,
Ambo University,
Ambo,
Ethiopia
E-mail: ayanayoom@gmail.com
Received Date: September 21, 2020;Accepted Date: October 05, 2020; Published Date: October 12, 2020
Citation: Chimdessa A, Tamiru I, Lemmessa F (2020) Knowledge of Neonatal Danger Signs and its Determinant Factors among Mothers Attending Postnatal Care in Nekemte, Ethiopia, 2019: Cross Sectional Descriptive Study. Glob J Res Rev Vol.7 No.2:53
Abstract
Background: Globally, 75% of neonatal death occurs within the first seven days of delivery. Neonatal mortality accounts for 40% of total child mortality. Low and middleincome countries contribute 99% of neonatal deaths. Globally, Ethiopia is one of top ten countries with the highest number of neonatal deaths. To alleviate this, Ethiopian Federal Ministry of Health launched Reproductive Maternal Neonatal and Child Health (RMNCH) services to be provided by Health Extension Workers (HEWs). Despite to this, health centers and health posts (HPs) Service Availability and Readiness Assessment (SARA) report showed health care facilities do not have adequate necessary materials and capacities to provide quality RMNCH services. Therefore, it was the aim of this study to examine the knowledge of neonatal danger signs and its determinant factors among mother’s attending postnatal care in public health care facilities in Ethiopia.
Methods: Institutional based cross sectional survey was conducted to evaluate mother’s knowledge of neonatal danger signs and its determinant factors among mothers’ attending postnatal care in Ethiopia. A total of 250 women who attended Post-Natal Care (PNC) follow up in four public health care institutions were recruited by simple random sampling. Data was collected by using pre-tested interviewer administered questionnaire and analyzed using logistic regression.
Results: The study has examined knowledge of neonatal danger signs and its determinant factors among mother’s attending postnatal care in public health care facilities, Ethiopia. Overall, 73.71% mothers had poor knowledge of neonatal danger signs. Multivariate analysis shows being younger women, government employed, high monthly income, regular Antenatal Care (ANC) follow up, and receiving neonatal danger signs counseling and being urban residence were major contributing factors to had good knowledge of neonatal danger signs. However, never had been to school, place of delivery were factors contributing in poor knowledge of neonatal danger signs.
Conclusions: Knowledge of neonatal danger signs is poor among participants, where 73.71% of mothers had poor knowledge about danger signs. Therefore, educating mothers during ANC and PNC period, health messages of neonatal danger signs and establishment of pregnant mothers’ group discussion and capacity buildings should be considered.
Keywords
Knowledge; Neonatal; Danger signs; Nekemte; Ethiopia
Abbreviations
ANC: Ante-Natal Care; B.Sc.: Bachelor of Science; EDHS: Ethiopian Demographic and Health Survey; FMH: Federal Ministry of Health; HEWs: Health Extension Workers; IMNCI: Integrated Management of New-born and Childhood Illness; RMNCH: Reproductive Maternal Neonatal and Child Health; SARA: Service Availability and Readiness Assessment; PNC: Post-Natal Care
Background
Neonatal death is a global public concern. Globally, about 75% of neonatal death occurs within the first seven days of delivery [1]. Each year, dozens of neonates die during the first 4 weeks of their life. Worldwide neonatal mortality makes up 40% of total child mortality. Low and middle-income countries contributes about 99% of deaths [1,2]. The study shows that most neonatal deaths occurred soon after birth, about 3/4 were caused by low birth weight/prematurity or asphyxia [3]. Mothers’ knowledge and practice play a crucial role for the survival and future healthy life of neonates. Good maternal knowledge of neonatal danger signs has positive impact for child health and survival [4].
Postnatal period has been identified as a one of crucial time, to deliver messages about neonatal danger signs, able mothers to identify neonatal risks and make them to seek medical assistance on early time. Early identification of new born danger signs, prompt and appropriate health care serves are a backbone to reduce neonatal death [4,5]. Neonates are more prone to show subtle signs of danger signs that need immediate health care services [5,6].
Different tools have been identified and integrated to health care services to reduce neonatal mortality in several countries. Integrated Management of New born and Childhood Illness (IMNCI) developed by World Health Organization (WHO) that focuses on assessment of general danger signs to examine children presenting with different illness [7]. Families should have awareness about assessment tools to encourage early health care seeking behaviour. On this assessment tools twelve neonatal danger signs were described and noted well [7].
Poor knowledge of neonatal danger signs negatively affects health care seeking behaviour of families. Mothers and primary health caregivers’ lack of knowledge coupled with poor cultural beliefs to seek health care are contributing factors for serious neonatal morbidity and mortality. Further, quality of health care services and counselling message of neonatal danger signs practice are critical determinant factors for neonatal mortality and morbidity [4,8]. Neonatal deaths account huge number in sub-Saharan countries. Different studies show that majority of neonatal deaths occur at home, indicating families do not recognize neonatal danger signs and result in poor health care seeking behaviours [8,9].
Research findings show that about 72% of neonatal deaths might be averted if universal health coverage of proven cost effective interventions and quality health care put into practices [10,11]. Universal health coverage caught up by several barriers. Particularly, in sub-Saharan countries these barriers contribute for a dozens of new born mortality. The potential barriers include/but not limited to unavailability of health care services, inadequate number of skilled personnel, geographical inaccessibility, poor quality, financial constraints, no need for such services, cultural practices, mothers’ awareness and sociodemographic characteristics (income, educational status) are prominent factors [12,13].
Ethiopia is one of top ten countries with highest number of neonatal deaths globally. Ethiopian Demographic and Health Survey (EDHS) show that skill full assisted delivery accounts about 10%, which is very low. In addition, low antenatal and postnatal care coupled with poor quality care results in 122,000 new born deaths each year [4,11,14]. To respond to this problem, Ethiopian Federal Ministry of Health (FMOH) launched Reproductive Maternal Neonatal and Children Health (RMNCH) to be provided by Health Extension Workers (HEWs) in all parts of the country [15,16]. Despite to this measure, HEWs and health centers Service Availability and Readiness Assessment (SARA) report showed that HEWs and health centers (ANC, PNC, delivery and EPI unities) do not equip with necessary medicines, medical supplies, guidelines and up-to date trainings to provide quality RMNCH services. Even though several efforts made so far in the country, neonatal mortality rate remains high (37/1000 live births). Nationally, Oromia regional state contributes (40 per 1,000 live births) deaths which is higher than the national [4,14]. Hence, it was the purpose of this study to assess mothers’ knowledge about neonatal danger signs and its determinant factors in four public health facilities. This finding provide directions for both health care policy makers and front line health care providers to plan for counselling message of neonatal danger signs and provide on time and appropriate interventions to reduce neonatal mortality in low and middle income countries.
Materials and Methods
Study design
Institutional based cross sectional survey was conducted to evaluate mother’s knowledge of neonatal danger signs and its determinant factors among mother’s attending postnatal care in Nekemte town, Ethiopia from March to April 2019.
Sample size
Simple random sampling, particularly lottery method was used to recruit participants in to the study. A total of 250 women who attended Post-Natal Care (PNC) follow up in four public health care institutions (two hospitals and health centers) were recruited into the study. Participants who were critical ill during data collection period were excluded from the study. Sample size was calculated by using p=18.2% from the previous study. The study used CI 95%, margin of error d=0.05 and 10% of non-response rate. In this study, participants who answered an average of danger signs questions (six out of twelve) scored good knowledge and who scored below an average considered as having poor knowledge of neonatal danger signs.
Data collection procedure
Standardized structured interview-based questionnaire was used for data collection. The questionnaire first prepared in English language and then translated by formal translator to local language (Afan Oromo) then back to English to check for its consistency of meanings. Finally, the local language version was used for data collection. Before actual data collection, the questionnaire was pre-tested on 5% of sample size in Sire town. Based on the pretest results, some amendments of questionnaire were done. Data were collected by 6 B.Sc. Nurses and Midwifes and two trained supervisors supervised data collection. For all data collectors and supervisors, two days of intensive training was given on the objectives, procedures and content of the study.
Data processing and analyzing
Data were first interred in to Epi Info 7 and exported to IBM SPSS statics version 20.0 to clean and analyze data. Frequencies, proportions, mean and summary statics were used to describe parameters under investigations. Association between outcome variable and independent variables were assessed and presented using odd ratio and confidence intervals. Multivariate logistic regression is done to control for possible confounders.
Ethical clearance was obtained from Wollega University, school Nursing and Midwifery Institutional Review Board (IRB) committee. Prior to actual data collection, a formal letter was given to all health care institutions. Verbal informed consent was obtained from each study participants before actual data collection. Participation in the study was voluntary and information collected kept confidential.
Results
A total of 250 study participants have taken part in the study and 247 (98.8%) included into analysis. Three respondents excluded from analysis for a gross incompleteness of responses.
As shown in Table 1, the mean age of respondents was 26.8 (± 4.7) years. About 180 (72.9%) and 39 (15.8%) respondents were from Oromo and Amhara ethic group respectively. Majority, 205 (83%) of participants were protestant while, 33 (13.4%) orthodox followers. Above half, 214 (86.63) of respondents were married and 8 (3.1%) were single. Of the total, 76(30.8%) participants never had been to school, whereas, the remaining participants educational background ranges from primary to B.Sc. About 159 (64.4%) were housewives, 59 (23.9%) self-employed and 29 (11.7%) were government employed. About 65 (26.3%) respondents were from rural resident.
| Variables | Frequency | |
|---|---|---|
| Number | % | |
| Age: mean=26.8 (± 4.7) | ||
| 15-24 | 13 | 5.3 |
| 25-34 | 159 | 64.4 |
| 35-44 | 65 | 26.3 |
| Above 45 | 10 | 4 |
| Ethnicity | ||
| Oromo | 180 | 72.9 |
| Amhara | 39 | 15.8 |
| Others | 28 | 11.3 |
| Religion | ||
| Muslim | 9 | 3.6 |
| Orthodox | 33 | 13.4 |
| Protestant | 205 | 83 |
| Others | 3 | 1.2 |
| Occupation | ||
| House wife | 159 | 64.4 |
| Government employed | 29 | 11.7 |
| Self employed | 59 | 23.9 |
| Educational status | ||
| Never been to school | 76 | 30.8 |
| Primary | 44 | 17.8 |
| Secondary | 46 | 18.6 |
| Diploma and above | 81 | 32.8 |
| Marital status | ||
| Married | 214 | 86.7 |
| Single | 7 | 2.8 |
| Divorced | 21 | 8.5 |
| Widowed | 5 | 2 |
| Neonate sex | ||
| Male | 125 | 50.6 |
| Female | 122 | 49.4 |
| Monthly house hold income | ||
| Low | 129 | 52.2 |
| Medium | 87 | 35.2 |
| High | 31 | 12.6 |
| Mothers residency | ||
| Urban | 182 | 73.7 |
| Rural | 65 | 26.3 |
| Distance to health institution | ||
| <5 km | 176 | 71.3 |
| 5-20 km | 29 | 11.7 |
| >20 km | 42 | 17 |
Table 1: Socio-demographic characteristics of women attended PNC follow up in public hospitals and health centers in Nekemte Town, Ethiopia, 2018 (n=247).
Health seeking behaviors and obstetric history of mothers
Majority, 160 (64.8) of participants were multiparous mothers. About 165 (66.8%) of participants had visited health institutions for antenatal care services during their last pregnancy. Above half 89 (53.9%) of respondents initiated antenatal care after 16 weeks of gestational age for their last pregnancy. Whereas, 76 (46.1%) were seek ANC follow up earlier (<16 weeks of gestational age). About 91 (55.2%) of study participants were visited health institutions for ANC services less than WHO recommended times (<4 times) in their last pregnancy.
Only 43 (26.1%) of mothers were received neonatal danger signs counseling message during their last pregnancy of ANC visits.
Majority, 113 (45.7%) of participant’s last place of delivery was hospitals. Of the total, 231 (93.5%) and 16 (6.5%) participants had vaginal and caesarian section mode of delivery respectively. Only 79 (32.0%) mothers received neonatal danger signs counseling during PNC services (Table 2).
| Variables | n | % |
|---|---|---|
| Parity | ||
| Uniparous | 87 | 35.2 |
| Multiparous | 160 | 64.8 |
| ANC follow up of last pregnancy | ||
| Yes | 165 | 66.8 |
| No | 82 | 33.2 |
| Health providers of ANC follow up | ||
| Health professionals (B.Sc. and above) | 109 | 66.1 |
| Health extension worker | 56 | 33.9 |
| Time of first ANC visit | ||
| <16 weeks | 76 | 46.1 |
| ≥ 16 weeks | 89 | 53.9 |
| Number of ANC visits | ||
| <4 | 91 | 55.2 |
| ≥ 4 | 74 | 44.8 |
| Counseled on neonatal danger signs at ANC | ||
| Yes | 43 | 26.1 |
| No | 122 | 73.9 |
| Place of delivery | ||
| Hospitals | 113 | 45.7 |
| Health center | 75 | 30.4 |
| Health post | 12 | 4.9 |
| Private clinic | 15 | 6.1 |
| Home | 32 | 13 |
| Mothers assisted during deliver | ||
| Health care professionals | 183 | 74.1 |
| Health extension workers | 35 | 14.2 |
| TBA | 9 | 3.6 |
| UTTBA | 20 | 8.1 |
| Mode of delivery | ||
| Vaginal | 231 | 93.5 |
| C/section | 16 | 6.5 |
| Mother received PNC services in 1st week | ||
| Yes | 194 | 82.6 |
| No | 53 | 17.4 |
| Health care providers of PNC | ||
| Professionals (B.Sc. and above) | 154 | 49.8 |
| Health extension | 40 | 33.2 |
| Neonatal danger sign counseling during PNC | ||
| Yes | 79 | 32 |
| No | 168 | 68 |
Table 2: Maternal health seeking behaviours and obstetric history of women attended PNC follow up in public health institutions in Nekemte Town, Ethiopia, 2018 (n=247).
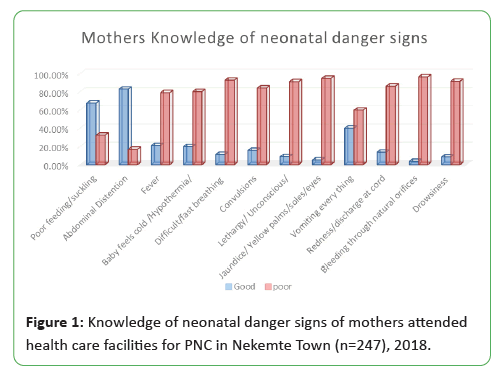
The overall knowledge of mothers’ on each of twelve neonatal danger signs
This study finding showed that the overall percentage of Good and Poor knowledge of mothers about neonatal danger signs accounted 26.29% and 73.71%, respectively.
The above Figure 1 shows that the knowledge of neonatal danger signs among postnatal visitor mothers. Majority, 167 (67.61%) of participants had good knowledge of poor feeding and abdominal distension 205 (82.99%) of danger signs. Contrarily, majority of the study respondents had poor knowledge of all the remaining neonatal danger signs ranging from 99 (40.08%) to 9 (3.64%) accounted by vomiting everything and bleeding through natural orifices, respectively.
Determinant factors of danger signs knowledge Among postnatal mother’s
Different variables were tested against participants’ knowledge of neonatal danger signs by using bivariate and multivariate logistic regressions. Multivariate analysis shows that being younger women (age rage 15-19 years ) (AOR 2.87, (95% CI, 4.78, 1.41)), government employed (AOR 3.07, (95% CI, 2.41, 1.89)), high average monthly income of house hold (AOR 3.11, (95% CI, 3.73- 2.18)), ANC follow up (AOR 3.41, (95% CI, 3.92-2.04)), receiving neonatal danger signs counselling message during post-natal care (AOR 3.70, (95% CI, 2.06, 1.49)) and urban residence (AOR 1.72, (95 CI, (2.04-1.68)) were recognized as major favouring factors likely to have good knowledge of neonatal danger signs compered to their counterparts. However, never had been to school (AOR 0.15, (95% CI, 0.52-0.25)), place of delivery (AOR 0.46, (95% CI, 0.38, 0.24)) or (AOR 0.32, (95% CI, 0.63, 1.27)) were major factors to likely have poor knowledge of neonatal danger signs compared to their comparable groups (Table 3).
| Variables | Good Knowledge | Poor knowledge | COR(95% CI) | p-value | AOR(95% CI) | p-value |
|---|---|---|---|---|---|---|
| Age category | ||||||
| 15-19 | 8(3.2.%) | 5(2.0%) | 2.67(2.50-8.43) | 0.001 | 2.87(4.78-1.41) | 0.002 |
| 20-29 | 124(50.2%) | 35(14.2%) | 3.62(3.99-6.29) | 0.253 | 3.32(2.64-3.49) | 0.358 |
| 30-39 | 30 (12.1%) | 35(14.2%) | 3.40(3.68-5.52) | 0.28 | 4.34(2.37-3.08) | 0.239 |
| >40 | 2 (0.81) | 8 (3.2) | 1 | 1 | ||
| Educational status | ||||||
| Never had been to school | 21(8.5%) | 55(22.3%) | 0.81(0.76-0.47) | 0.003* | 0.15(0.52-0.25) | 0.001* |
| Primary | 14 (5.7%) | 30(12.1%) | 0.61(0.37-0.57) | 0.004* | 0.52(0.27-0.39) | 0.06 |
| Secondary | 28(11.3%) | 18(7.3%) | 0.37(0.21-0.52) | 0.002* | 0.23(0.14-0.21) | 0.07 |
| Diploma and above | 67(27.1%) | 14(5.7%) | 1 | 1 | ||
| Occupational status | ||||||
| Housewife | 29 (11.7) | 130(52.6) | 1 | 1 | ||
| Self-employed | 32 (13.0%) | 27(11.0%) | 3.29(2.17-1.88) | 0.04 | 2.51(2.05-1.64) | 0.27 |
| Government employed | 26(10.5%) | 3(1.2%) | 4.32(3.02-2.50) | 0.003 | 3.07(2.41-1.89) | 0.002 |
| Monthly house hold income | ||||||
| Low | 35(14.2%) | 94(38.1%) | 1 | 1 | ||
| Medium | 39(15.8%) | 48(19.4%) | 0.97(0.41-0.215) | 0.003* | ||
| High | 28(11.3%) | 3(1.2%) | 4.08(4.23-3.09) | 0.001* | 3.11(3.73-2.18) | 0.002* |
| Parity | ||||||
| Uniparous | 59(23.9%) | 28(11.3) | 1 | |||
| Multiparous | 98(39.7%) | 62(25.1%) | 2.373(1.158-4.84) | 0.018* | ||
| ANC follow up of last pregnancy | ||||||
| Yes | 101(61.2%) | 64(38.8%) | 4.03 (5.82-4.10) | 0.003 | 3.41(3.92-2.04) | 0.013 |
| No | 15(18.3%) | 67(81.7%) | 1 | - | - | |
| Place of delivery | ||||||
| Home | 3(1.2%) | 29(11.7%) | 0.63(0.59-0.36) | 0.001 | 0.46(0.38-0.24) | 0.01 |
| Health post | 4(1.6%) | 8(3.2%) | 0.56(0.84-0.45) | 0.025 | 0.32(0.63-1.27) | 0.02 |
| Health center | 39(15.8) | 36 (14.6) | 0.72(0.62-0.43) | 0.061 | ||
| Private clinic | 9(3.6) | 6(2.4) | 0.41(0.92-0.31) | 0.08 | ||
| Hospital | 101(40.9) | 12 (4.9) | 1 | 1 | ||
| Counseling of neonatal danger signs during PNC follow up | ||||||
| Yes | 57(72.2%) | 22(27.8%) | 7.09(4.65-2.49) | 0.021 | 3.70(2.06-1.49) | 0.031 |
| No | 63 (37.5%) | 105(62.5%) | 1 | 1 | ||
| Mothers residence | ||||||
| Urban | 123(67.6) | 59(32.4) | 2.51(3.72-2.10) | 0.03 | 1.72(2.04-1.68) | 0.012 |
| Rural | 11(16.9) | 54(83.1) | 1 | |||
| Distance to health institution | ||||||
| <5 km | 145(58.7) | 31(12.6) | 1 | 1 | ||
| 5-20 km | 21(8.5) | 8(3.2) | 0.63(0.57-2.06) | 0.07 | ||
| >20 | 14(5.7) | 28(11.3) | 0.32(0.32-2.05) | 0.04 | ||
Table 3: Determinant factors of neonatal danger signs knowledge among postnatal mothers’ in public health care facilities, Nekemte, Ethiopia, 2018 (n=247).
Discussion
This study examined the prevalence and determinant factors of neonatal danger signs knowledge among postnatal care mothers in Nekemte town, Ethiopia.
The findings revealed that poor knowledge of neonatal danger signs among the study units was massive. Majority, 73.71% have poor knowledge of neonatal danger signs. However, previous studies conducted in India and Bangladesh shows about 76.7% and 65% of participants have good knowledge of neonatal danger signs, respectively [17,18]. The difference might be due to socioeconomic and educational background of study participants. This study asserts that women who have higher level of education were likely to have better knowledge of neonatal danger signs than their counterparts; which is similar with other findings.
In this study, about 30.8% and 17.8% of participants were never had been to school and completed primary education respectively. Whereas, the study conducted in India and Karnataka shows that about 46.7% and 26% participants were completed primary education and there are no mothers never had been to school among study participants [17,18]. The difference might be due to economy, cultural belief on education and residence of the study participants. This finding shows that an average monthly house hold income is found as one of significant predictors whether to have good or poor knowledge of danger signs. Those women with high average monthly income were knowledgeable of danger signs compared to their comparable group. This finding is similar with others studies conducted in India [19,20]. ANC follow up is one of determinant factors that determine the knowledge of neonatal danger signs. Participants who followed ANC were more knowledgeable than their counter group. However, the study conducted in Ethiopia shows only 34% mothers’ attend ANC follow up at least once for their last birth [21]. The study conducted in Sir-Lank and Ghana shows that mothers’ who follows regular ANC have good knowledge of neonatal danger signs than non-followers of ANC [22,23]. This study revealed that only 26.1% of mothers were received neonatal danger signs counseling message during their last pregnancy of ANC visits. However, the study conducted in Kenya shows that about 42.8% mothers received neonatal danger signs counselling during antenatal care. This difference might be due to quality service of RMNCH, poor counseling capacity and inadequate medical supplies in health centers and health posts facilities [24,25].
This finding shows that more of study subjects have good knowledge of poor feeding and abdominal distension danger signs out of the total (twelve danger signs), while on the rest of danger signs; mothers have poor knowledge. In line to this finding, the research conducted in Nigeria shows that mother’ knowledge ranges from 25.4% to 1.7% for fever and fast breathing, respectively [26].
Conclusion
Mother’s knowledge of neonatal danger signs was low among mothers attending postnatal care. Overall, 73.71% mothers had poor knowledge of neonatal danger signs. Multivariate analysis shows being never had been to school, place of delivery (home and health posts) were factors contributing in poor knowledge of neonatal danger signs.
Recommendation
Health care force role in educating mothers during ANC and PNC period should be emphasized. Efforts should be made to provide health messages about neonatal danger signs for all mothers attending ANC and PNC. Establishment of pregnant mothers’ group discussion session during ANC and PNC (group ANC and PNC), supporting HPs and health centers by providing capacity buildings through trainings and regular feedback should be considered.
Limitation of the Study
This study used only institutional cross-sectional study design in a single town of the country
Ethical Approval and Consent to Participate
Ethical approval for the research was sought from Wollega University, school Nursing and Midwifery Institutional Review Board (IRB) committee. Permission to interview mothers was obtained from the management of respective health facilities and verbal consent taken from each participant. Participation in the study was voluntary and information collected kept confidential.
Author’s Contribution
Ayana Chimdessa, Italem Tamiru and Lati Melkamu actively participated from conceptualizing the study protocol to the final result write-up and Ayana Chimdessa prepared the manuscript. Both authors read and approved the final manuscript.
Consent for Publication
Not applicable
Competing Interest
All authors declare that they have no any competing interest.
Declaration
This research is our original work and has not been submitted for publication anywhere else.
Availability of Data and Materials
All data generated and analyzed during this study are available upon request.
References
- Lawn JE, Kerber K, Enweronu-Laryea C, Bateman OM (2009) Newborn survival in low resource settings are we delivering? BJOG: An international journal of obstetrics and gynaecology 116: 49–59.
- Lawn JE, Lee AC, Kinney M, Sibley L, Carlo WA, et al. (2009) Two million intrapartum-related stillbirths and neonatal deaths: Where, why, and what can be done? Int Journal Gynecology Obstet 107(S1): 5-18.
- Matendo RM, Engmann CM, Ditekemena JD, Gado J, Tshefu A, et al. (2011) Challenge of reducing perinatal mortality in rural Congo: findings of a prospective, population-based study. J Health Popul Nutri 29: 532–540.
- Bhutta ZA, Darmstadt GL, Hasan BS, Haws RA (2005) Community-based interventions for improving perinatal and neonatal health outcomes in developing countries: A review of the evidence. Pediatrics 115(S2): 519–617.
- Bang AT, Bang RA, Reddy MH, Baitule SB, Deshmukh MD, et al. (2005) Simple clinical criteria to identify sepsis or pneumonia in neonates in the community needing treatment or referral. Pediatric Infect Dis J 24: 335–341.
- Baqui AH, Rahman M, Zaman K, El Arifeen S, Chowdhury HR, et al. (2007) A population-based study of hospital admission incidence rate and bacterial etiology of acute lower respiratory infections in children aged less than five years in Bangladesh. J Health Popul Nutr 25: 179-188.
- WHO recommendations on postnatal care of the mother and new born. (2013)
- Lawn JE, Kerber K, Enweronu-Laryea C, Cousens S (2010) 3.6 million neonatal deaths-what is progressing and what is not? Semin Perinatol 34: 371-386.
- Lawn JE, Kinney MV, Black RE, Pitt C, Cousens S, et al. (2012) Newborn survival: A multicounty analysis of a decade of change. Health Policy Plan 27(S2): 6-28.
- Darmstadt GL, Oot DA, Lawn JE (2012) Newborn survival: Changing the trajectory over the next decade. Health Policy Plan 27(S3): 1-5.
- World Health Organization. Integrating maternal, newborn and child health programmers: The world health report 2005. (2005)
- SNL/Save the Children Ethiopia combine report. (2000)
- Federal Democratic Republic of Ethiopia. Ministry of Health National. Reproductive Health strategy (2006).
- Callaghan-Koru JA, Seifu A, Tholandi M, Graft-Johnson JD, Daniel E, et al. (2013) Newborn care practices at home and in health facilities in 4 regions of Ethiopia. BMC Pediatrics 13: 198.
- Ministry of Health (MOH) Ethiopia. Health Sector Development Programme IV 2010/11-2014/15.
- Ethiopia’s Health Extension Program: Pathfinder International Support (2008) 2003-2007.
- Choi Y, El Arifeen S, Mannan I, M Rahman S, Bari S, et al. (2010) Can Mothers Recognise Neonatal Illness Correctly? Comparison of Maternal Report and Assesment by Community Health Workers in Rural Bangladesh. Trop Med Int Health 15: 743-53.
- Dongre A.R., Deshmukh P.R., Garg B.S (2009) Awareness and health care seeking for newborn danger signs among mothers in peri-urban Wardha. Indian J Pediatr 76: 691-693.
- Darmstadt GL, Bhutta ZA, Cousens S, Adam T, Walker N, et al. (2005) Evidence-based, cost-effective interventions: How many newborn babies can we save? Lancet 365: 977-88.
- Tripathy P, Nair N, Barnett S, Mahapatra R, Borghi J, et al. (2010) Effect of a participatory intervention with women’s groups on birth outcomes and maternal depression in Jharkhand and Orissa, India: A cluster-randomized controlled trial. Lancet 375: 1182–1192.
- Chimdessa A, Estifanos N, Markos J (2019) Magnitude of late ANC booking and its determinant factors among pregnant women attended public health centers and private clinic in Artumafursi district Amara regional state, special zone of Oromia, Ethiopia 2017. Glob J Med Res: K interdisciplinary 19: 1-7.
- Dongre AR, Deshmukh PR, Garg BS (2008) Perceptions and health care seeking about newborn danger signs among mothers in rural wardha. Indian J Pediatr 75: 325-9.
- Waiswa P, Kallander K, Peterson S, Tomson G, Pariyo GW (2010) Using the three delays model to understand why newborn babies die in eastern Uganda. Tropical Medicine and International Health 15: 964-972.
- Kibaru EG, Otara AM (2016) Knowledge of neonatal danger signs among mothers attending well baby clinic in Nakuru Central District, Kenya: Cross sectional descriptive study, BMC Res Notes 9: 481.
- Asp G, Sandberg J, Ezechi O, Pettersson KO (2011) Challenges of immediate newborn care in maternity units in Lagos, Nigeria: an observational study. J Obstet Gynaecol 31: 612-616.
- Ekwochi U, Ndu IK, Osuorah CDI, Amadi OF, Okeke IB, et al. (2015) Knowledge of danger signs in newborns and health seeking practices of mothers and care givers in Enugu state, South-East Nigeria. Ital J Pediatr 41:18.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences