GravesÃÆâÃâââ¬Ãââ⢠disease and Down syndrome: A Case Report
1Consultant Endocrinology, Head of Endocrinology Department, Salmanyia Medical Complex, Bahrain
2Chief Endocrinology Resident, Department of Endocrinology, Salmanyia Medical Complex, Bahrain
3Radiology Resident, Department of Radiology, Salmanyia medical Complex, Bahrain
- *Corresponding Author:
- Ebtihal Al Yusuf
Chief Endocrinology Resident, Department of Endocrinology,
Salmanyia Medical Complex, Bahrain
Tel: +973 33322488
E-mail: ealyusuf82@gmail.com
Citation: Khalaf S, Yusuf E, Yusuf Z (2018) Graves ’ disease and Down Syndrome: A Case Report. Endocrinol Res Metab Vol.2.No.1:11.
Copyright: © 2018 Yusuf E, et al. This is an open-access article distributed under the terms of the creative commons attribution license, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Down syndrome is the most common chromosomal abnormality in humans. People affected by Down syndrome have high prevalence of autoimmune diseases. The most common autoimmune disease in this group of people is hypothyroidism. Hyperthyroidism occurs less frequent in this group of patients, but it is likely to be underestimated. We are presenting a case of Down syndrome and Graves’ disease. A 17-year-old Bahraini girl with Down syndrome and congenital heart disease, presented with history of weight loss within 6 months. Graves’ disease was confirmed based on laboratory and imaging results. Carbimazole 30 mg daily was started and increased to 40 mg daily. Adequate clinical and laboratory results were achieved. The association between Graves’ disease and Down syndrome is well known in medical practice and frequently reported in the literature. High clinical suspicion is crucial for early diagnosis and treatment. Different treatment modalities are available. Each modality carries different remission rate.
Keywords
Down syndrome; Graves’ disease; Hyperthyroidism
Introduction
Thyroid disorders are common in people with Down syndrome (DS) [1]. It’s estimated that 4% to 18% of children with DS, have thyroid dysfunction [2]. Autoimmune disturbance has been the most important contributing aetiology for the acquired thyroid disorders in DS [3].
Thyroid disorders in DS are a focus of interest in researches for decades [4]. Prevalence studies have shown that hyperthyroidism occurs less frequently than hypothyroidism in people with DS [5]. However, Hyperthyroidism is more prevalent in people with DS than in general population (6.55 in 1000 (0.66%) in DS vs. 1 in 5000 (0.02%) in general population) [6]. In 1946, Glichrist has reported the first case of hyperthyroidism in a person with DS [7]. Twelve cases of Graves’ disease were diagnosed in a large systemic review of 1,856 patients with DS which was held from 1991 to 2006 in Spain [8]. No data about the prevalence of thyroid dysfunction in DS in Bahrain population. In Kuwait, one of the countries in the same region, a study of thyroid dysfunction in 58 subjects with DS was reported by Ali F. and his colleagues. One subject only was found to be hyperthyroidism in the studied group [9]. Debate on how best to treat people with DS and hyperthyroidism still continues. Some studies have suggested that Radioactive Iodine I-131 (RAI) ablation is preferred, because of failure of remission while on Carbimazole and repeated relapse after discontinuation [10]. Other studies reported that response is good to Propylthiouracil when thyroid stimulating antibodies are elevated [11].
We report this case of a girl with DS and hyperthyroidism because of the relative rarity of the condition.
Case Report
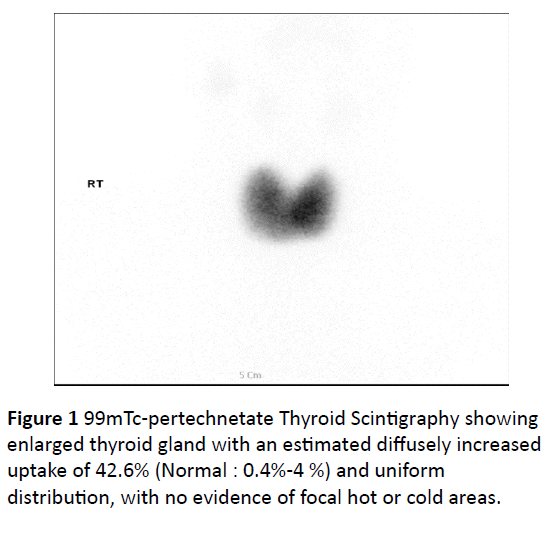
A 17-year old Bahraini girl who was diagnosed with Down syndrome (DS) after birth, when chromosomal analysis confirmed triosomy-21-karyotype (47, XY, +21). She had Patent Ductus Arteriosa which has been repaired at the age of 2 years, without any residual shunt on subsequent follow up. She was on regular follow up in the cardiology clinic. Weight loss was noticed by her mother when she was 12 years old. She lost around 5 kgs in a 6 months period. She also had palpitation and hyperhidrosis. She has been investigated by her cardiologist for whom his initial laboratory results were consistent with hyperthyroidism. She was referred to endocrinology clinic. Physical examination revealed a thin girl with features of DS, worm sweaty hands, fine tremors, sinus tachycardia, diffuse goitre, and exophthalmos. Her weight was 19 kg, height was 128 cm, and pulse was regular with a rate of 110 beats per minute. Thyroid function test was consistent with hyperthyroidism (Table 1). Thyroid scan showed enlargement of both lobes of thyroid gland with diffuse increased uptake of 42.6% (Normal: 0.4%-4%) (Figure 1). Thyroid antibody assay was negative. A diagnosis of Graves’ disease was made. She was started on propranolol 60 mg daily. Treatment modalities were explained to the mother and RAI was offered as a first line treatment measure. Since the patient was having intellectual disability, her mother was the decision maker for her. She chose the RAI therapy. But on the day of the appointment of RAI the patient refused to swallow the RAI capsule, because she has difficulty in swallowing the tablets. Carbimazole tablets 30 mg daily was started which was taken regularly by the patient after dissolving it in water. Her follow up Thyroid function with up titrating the Carbimazole up to 40 mg daily was normalized (Table 1). Her weight has risen to 24 kg. She is on regular follow up appointments in the endocrinology clinic with thyroid function test 6 monthly.
Table 1 Serial change of values of thyroid function test. TSH: Thyroid stimulating hormone, T3: Triiodothyronine, FT4: Free Thyroxine.
| Test | Results | Reference range | units | ||
|---|---|---|---|---|---|
| on presentation | 1 year on Carbimazole | 2 years on Carbimazole | |||
| TSH | 0 | 0.01 | 5 | 0.25-5.0 | mlU/L |
| T3 | 14 | 11 | 6 | 2.5-7.8 | pmol/L |
| FT4 | 57 | 34 | 12 | 6.0-24.5 | pmol/L |
Discussion
Hyperthyroidism in people with DS is rarely reported in the literature despite that hyperthyroidism in children and adolescent with DS is more common than in general population [6,12]. Clinical characteristics of hyperthyroidism in people with DS are similar to those found in general population with exception for the following: earlier presentation, no gender predominance, more frequent association with other autoimmune diseases, higher frequency of antecedent Hashimoto’s thyroiditis, less severe clinical course, and less frequent thyroid eye disease [6,12,13].
Literature review of the preferred treatment of hyperthyroidism in people with DS showed conflicting results. The first reported case of hyperthyroidism and DS in 1946 was treated with Lugols solution [7]. Most of the reported cases after that time were treated with thionamide and most of them reached euthyroid status. There are regional differences in the preferred treatment modality for patients of hyperthyroidism in DS. In USA, RAI therapy is preferred by most thyroid specialists. In Europe and Japan, antithyroid drugs are the preferred first line therapy [14]. In a large Italian study of 28 patients of DS with Graves’ disease, no patient required non-pharmacological treatment for which methimazole was continued for an average period of 2.8 ± 1.6 years [12]. The problem with thionamide treatment is the need for prolong course to achieve remission, poor compliance in this mentally subnormal group of patients, susceptibility to infections with the disturbed immune function in DS [4,15]. On the other hand, RAI can lead to fast remission in 95% of the cases [12]. It can be chosen as a treatment modality if there is any contraindication or failure of antithyroid medication. In a Spanish study of 12 patients of DS with Graves’ disease, all the patients required treatment with RAI due to short remission on Carbimazole [6]. RAI eliminates the compliance problems in this group of patients since it’s administered one time. The side effects of RAI are not significant such as: nausea and pain in the area of thyroid gland. Prescribing RAI for hyperthyroidism children with DS remains open for debate because of the risk of cancer. The younger the patient the higher the risk of cancer development [16]. Thyroidectomy in people with DS carries a negligible role because those patients do carry a high surgical risk because of short neck [15].
All available treatment modalities should be considered, and individualization of treatment option is a key concept in treating this group of patients because of the variability in therapy outcomes. Each modality has its own benefits and risks. Medical treatment can be complicated by poor compliance, RAI may increase the risk of cancers and surgery is invasive.
In the patient who was described in this case report, RAI was offered and was preferred by the mother. But because of difficulty in swallowing it was not taken and antithyroid pharmacotherapy was prescribed thereafter. Carbimazole results in normalization of thyroid function while on therapy. No side effects were noticed, but remission has not achieved.
Conclusion
Graves’ disease in patients with Down syndrome is more prevalent than in general population. High clinical suspicion of this condition is needed to achieve early diagnosis and treatment. Different treatment modalities carry different remission rates and the choice of treatment modality should be individualized.
References
- Graber E, Chacko E, Regelmann M, Costin G, Rapaport R (2012) Down Syndrome and Thyroid Function. Endocrinology and Metabolism Clinics of North America 41: 735-745.
- Bull M (2011) Health Supervision for Children With Down Syndrome. Pediatrics 128: 393-406.
- Aversa T, Lombardo F, Valenzise M, Messina M, Sferlazzas C, et al. (2015) Peculiarities of autoimmune thyroid diseases in children with Turner or Down syndrome: An overview. Italian Journal of Pediatrics 41:39.
- Kennedy R, Jones T, Cuckle H (1992) Down's syndrome and the thyroid. Clinical Endocrinology 37: 471-476.
- Prasher V (1994) Prevelance of thyroid dysfunction and autoimmunity in adults with Down syndrome. Down Syndrome Research and Practice 2: 67-70.
- Goday-Arno A, Cerda-Esteva M, Flores-Le-Roux J, Chillaron-Jordan J, Corretger J, et al. (2009) Hyperthyroidism in a population with Down syndrome (DS). Clinical Endocrinology 71: 110-114.
- Gilchrist L (1946) Thyrotoxicosis in a Mongol. BMJ 1: 237-238.
- Claret-Torrents C, Goday-Arno A, Cerdà-Esteve M, Flores-Le Roux J, Chillarón-Jordan J, et al. (2009) Hyperthyroidism in Down Syndrome. International Medical Review on Down Syndrome 13: 2-8.
- Ali F, Bayoumy H, Mohammad A, Al-Busairi W, Al-Othman A (2002) Thyroid Function in Kuwaiti Subjects with Down’s Syndrome. Medical Principles and Practice 11: 206-209.
- Damle N, Das K, Bal C (2011) Graves’ disease in a Down’s syndrome patient responds well to radioiodine rather than antithyroid drugs. Journal of Pediatric Endocrinology and Metabolism 24:611.
- Bhowmick S, Grubb P (1997) Management of Multiple-Antibody–Mediated Hyperthyroidism in Children With Downʼs Syndrome. Southern Medical Journal 90: 312-315.
- De Luca F, Corrias A, Salerno M, Wasniewska M, Gastaldi R, et al. (2009) Peculiarities of Graves' disease in children and adolescents with Down's syndrome. European Journal of Endocrinology 162: 591-595.
- Burch H (1993) Graves' ophthalmopathy: current concepts regarding pathogenesis and management. Endocrine Reviews 14: 793.
- Wartofsky L, Glinoer D, Solomon B, Nagataki S, Lagasse R, et al. (1991) Differences and Similarities in the Diagnosis and Treatment of Graves' Disease in Europe, Japan, and The United States. Thyroid 1: 129-135.
- Takahashi H, Bordy M, Sharma V, Grunt J (1979) Hyperthyroidism in Patients with Down's Syndrome. Clinical Pediatrics 18: 273-275.
- Dickman P, Holm L, Lundell G, Boice J, Hall P (2003) Thyroid cancer risk after thyroid examination with131I: A population-based cohort study in Sweden. International Journal of Cancer 106: 580-587.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences