Giant Angiolymphoid Hyperplasia: A Rare Cause of Prepatellar Bursitis and Review of its Unusual Presentations
Balu Ravi, Narendran Pushpasekaran*, Kavish Singh and Sathyamurthy Palanisaamy
Department of Orthopaedics, Medical Trust Hospital, Kerala, India
- *Corresponding Author:
- Narendran Pushpasekaran
Medical Trust Hospital, Mahatma Gandhi Rd
Pallimukku, Kochi, 682016, Kerala, India
E-mail: drnaren247ortho@gmail.com
Received date: December 12, 2017; Accepted date: March 29, 2018; Published date: April 06, 2018
Citation: Ravi B, Pushpasekaran N, Singh K, Palanisaamy S (2018) Giant Angiolymphoid Hyperplasia: A Rare Cause of Prepatellar Bursitis and Review of its Unusual Presentations. Int J Case Rep 2:4.
Copyright: © 2018 Ravi B, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Angiolymphoid hyperplasia with eosinophilia or epithelioid haemangioma is a rare benign vascular proliferative disorder usually affecting the scalp, face and neck and rarely reported in peripheral locations. Differentiation from Kimura disease, tuberculoma and Kaposi sarcoma is of utmost importance. The literature has no consensus in the treatment due to the paucity of cases reported. The recurrence rate has varied between 5-55% with the least rates reported after surgical excision. We report in a 15-year boy, a giant sized epithelioid haemangioma occurring as left prepatellar bursa swelling and presenting with a diagnostic dilemma. He underwent excision and wide marginal clearance and no adjuvants. He had no recurrence in a follow-up period of two years. We report this case in view of its varied presentation of this pathology and also review the cases of angiolymphoid hyperplasia with eosinophilia having unusual presentations and its current management.
Keywords
Angiolymphoid hyperplasia; Knee; Kimura disease; Tuberculoma; Recurrence
Abbreviations
ALHE: Angiolymphoid Hyperplasia with Eosinophilia
Introduction
Angiolymphoid hyperplasia with eosinophilia or epithelioid haemangioma is a rare benign vascular proliferative disorder that rarely occurs at peripheral locations and unusual large sized lesions are reported to have vascular associations [1,2]. There is no concise treatment at present and recurrence is the most common problem among the various treatment modalities available [3]. We describe the peculiar presentation, management and follow up of a giant sized epithelioid haemangioma occuring in the left prepatellar bursa of an adolescent male. We report this case in view of the varied presentation of this pathology and concomitant involvement in the knee arterial circulation. In this scenario, we also review the cases of angiolymphoid hyperplasia with eosinophilia having unusual presentations and its current management in order to concise a treatment strategy in the future.
Case Report
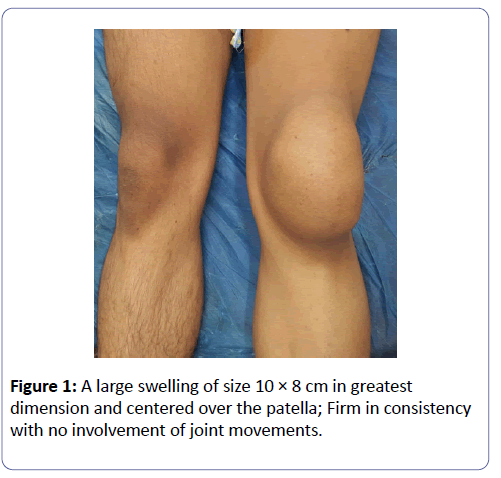
A 15 year boy presented with the chief complaints of gradually progressive swelling over the left knee for 5 years. He had occasional pain and discomfort on knee flexion. He denied any significant history of trauma, constitutional symptoms. His medical reports for the similar presenting problem revealed anti-tubercular medications for 8 months. On examination of the left knee, a solitary and localized swelling of 12 × 8 cm in greatest dimension and centering over the patellar region was noted (Figure 1). It was non-tender, firm in consistency and mobile with the patella. There was a limitation of flexion by 300. Inguinal and popliteal lymph nodes were comparable on both sides. General and systemic examinations were within normal limits.
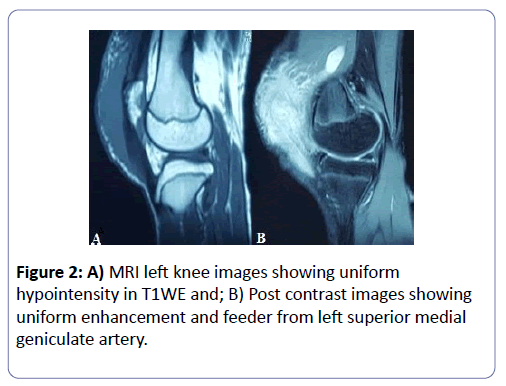
Blood investigations showed normal hemoglobin levels and total leucocyte count with normal differentials. ESR was 22 mm at 1 h. quantitative C-reactive protein was 2 mg/L. liver enzymes, renal parameters, and uric acid were within normal range. Viral markers were negative. Urine routine and microscopic examinations were also normal. Attempted aspiration of the swelling ended as dry tap. MRI of the left knee revealed a poorly encapsulated hypointense lesion on T1WE (Figure 2A) and mixed hyperintense lesions on T2WE images. Post contrast images showed uniform enhancement and contrast filling likely from the superior medial geniculate artery. (Figure 2B).
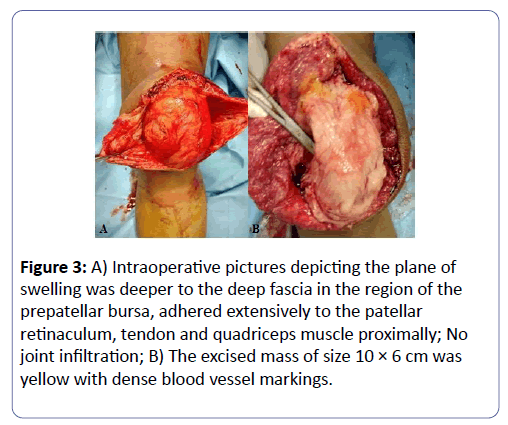
Planned excision biopsy was done through midline approach and under spinal anesthesia. The plane of swelling was deeper to the deep fascia in the region of the prepatellar bursa, adhered extensively to the patellar retinaculum, tendon and quadriceps muscle proximally (Figures 3A and 3B). No joint infiltration was seen and adequate clearance of about 0.5 cm margin was done. The excised mass of size 10 × 6 cm was yellow with densely coursing blood vessels and had granulomatous surface. No adjuvants were used.
Figure 3: A) Intraoperative pictures depicting the plane of swelling was deeper to the deep fascia in the region of the prepatellar bursa, adhered extensively to the patellar retinaculum, tendon and quadriceps muscle proximally; No joint infiltration; B) The excised mass of size 10 × 6 cm was yellow with dense blood vessel markings.
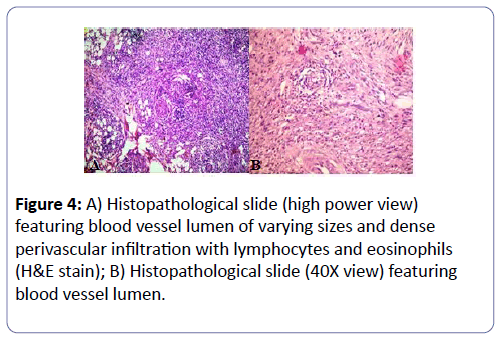
Histopathological examination showed small vessels of different calibers and shapes with interstitial and perivascular inflammatory infiltrate rich in lymphocytes and some eosinophils about 7%. No giant cells or granuloma formation was observed (Figures 4A and 4B).
The patient was put on knee brace for pain relief and ambulation till suture removal. The range of motion exercises and quadriceps strengthening started from day 3 post op. the patient returned to his normal activities after two weeks and kept in close follow-up for two years. No recurrence was noted during this period.
Discussion
Angiolymphoid hyperplasia with eosinophilia (ALHE) or epithelioid haemangioma or histoid hemangioma is rare benign vascular proliferative disorder. Various etiopathogenesis have been suggested, however, none have proven to be conclusive or definitive [1]. Differentiation from the similar spectrum of Kimura’s disease is of paramount importance. The involvement of deeper tissues such as lymph nodes, salivary glands the absence of adnexal structure involvement, peripheral eosinophilia and increased IgE levels and higher eosinophilic histopathology are differentiating features [4]. Our patient with superficial involvement (prepatellar bursa), the absence of lymph nodes and adnexal involvement favored ALHE. Peripheral eosinophilia is notably present only in 21% of cases [2].
The usual sites involved are centrally located in the region of the scalp, face and head with rare reports of the axilla, breast and penile involvement [4,5]. The presentation at unusual sites poses a diagnostic dilemma (Table 1). Hui-Wen Tseng et al. reported one such peripheral location in the forearm of a 34- year male [6]. There were multiple non-tender reddish lesions with a maximum of 1 cm size arising from a scar caused by welding burn. He underwent wide elliptical excision and skin grafting with no recurrence. Our patient was a 15-year boy with the involvement of left knee prepatellar bursa without any antecedent factors. It was solitary and in subfascial plane. He underwent excision with 0.5 cm clearance. We had no recurrence in 1 year follow up. Differential diagnosis of such a lesion in prepatellar bursa/bursitis involves trauma to the knee, Gout, Sarcoidosis, Kaposi sarcoma, CREST syndrome and Diabetes mellitus. Staphylococcus and tuberculous infection of the bursa can also occur [7].
| Sl. No | Author | Year | Presenting feature | Treatment instituted | Follow up | Remarks |
|---|---|---|---|---|---|---|
| 1 | Fite-Trepat L et al. [4] | 2017 | 57/F, Right occipital region for three years. | Surgical excision. | No recuurence in 9 months. | 7 × 6 cm excised mass had its feeder from right occipital artery. |
| 2 | Guinovart RM et al. [7] | 2014 | 47/F, Right retro auricular region for 8 years | Intralesional corticosteroids. | Recurrence in 5 months. | 4 × 3 cm coalescing lesions that did not respond to steroids. |
| 3 | Damle DK et al. [8] | 2013 | 36/M, ventral aspect of penis for 3 months | Surgical excision and circumcision. | No recurrence in 14 months. | Immunocompromised status (HIV). 3 × 2 cm lesion excised. |
| 3 | Doloi PK et al. [5] | 2012 | 18/F, left supra orbital region for about a year. | Repeat Surgical excision and triamcinolone instillation. | No recurrence in 7 months. | 2.5 × 2.2 cm mass excised in the second surgery. |
| 4 | Kukreja N al. [6] | 2011 | 29/ M, | Surgical excision and left axillary arterial repair. | No recurrence in 1 year. | 2.9 × 1.8 cm mass attached to the left axillary artery distal portion. |
| Left axilla for 2 years. | ||||||
| 5 | Tseng HW et al. [9] | 2010 | 35/ M, left forearm for 6 months | Surgical excision and split skin grafting. | No recurrence in 5 years. | About 10 nodular swellings arising from scar caused by welding burn. |
Table 1: The unusual sites of Angiolymphoid Hyperplasia with Eosinophilia and their treatment reported in literature; M: Male; F: Female; HIV: Human Immunodeficiency Virus.
Associations with large arteries like axillary, brachial and occipital artery have been reported leading to giant sized ALHE [2]. Laia Fite-Trepat et al. reported a 7 × 6 cm lesion in right suboccipital region with a large feeder from the occipital artery [4]. In our case, a giant size (10 × 6 cm) lesion in the left prepatellar bursa had its feeder from the left superior medial geniculate artery (Figure 3B).
Treatment of ALHE has not reached consensus and vary from case to case basis with judgments made from the previous case reports. Modalities include intralesional corticoid therapy, interferon therapy, laser, radiotherapy, cryotherapy, photodynamic therapy and application of imiquimod. However, surgical treatment has been the most common modality for primary, other failed modalities and with least recurrence rate [3]. We underwent an excision of the lesion with a marginal clearance of 0.5 cm and we had no recurrences. Similar has been noted in other reports [8-10].
In conclusion, ALHE infrequently occurs in a peripheral location and is one of the rare differentials for a prepatellar bursa swelling. Lesions progressing to giant size usually have active feeder vessels. There is no clear consensus on treatment at present. However, excision with adequate marginal clearance has shown to prevent recurrence in most reported cases.
Consent
Except for the personal identity, the patient consented to reveal his disorder for academic purposes.
References
- Guo R, Gavino ACP (2015) Angiolymphoid hyperplasia with eosinophilia. Arch Pathol Lab Med 139: 683-686.
- Vandy F, Izquierdo L, Liu J, Criado E (2008) Angiolymphoid hyperplasia involving large arteries. J Vasc Surg 47: 1086-1089.
- Adler BL, Krausz AE, Minuti A, Silverberg JI, Lev-Tov H (2016) Epidemiology and treatment of angiolymphoid hyperplasia with eosinophilia (ALHE): A systematic review. J Am Acad Dermatol 74: 506-512.
- Fite-Trepat L, Martos-Fernandez M, Alberola-Ferranti M, Pablo-Garcia-Cuenca AD, Bescosatin D (2017) Angiolymphoid hyperplasia with eosinophilia involving the occipital artery: a case report and review of literature. J Clin Diagn Res 11: ZD21-ZD23.
- Doloi PK, Khanna S (2012) Angiolymphoid hyperplasia with eosinophilia- A Case Report. Int J Otolaryngol 1: 44-47.
- Kukreja N, Koslowski M, Insall R (2011) Angiolymphoid hyperplasia with eosinophilia presenting as an axillary artery aneurysm. BMJ Case Rep.
- Guinovart RM, Bassas-Vila J, Morell L, Ferrándiz C (2014) Angiolymphoid hyperplasia with eosinophilia: A clinicopathologic study of 9 Cases. Actas Dermosifiliogr 105: e1-e6.
- Damle DK, Raotole SS, Belgaumkar VA, Mhaske CB (2013) Angiolymphoid hyperplasia with eosinophilia on penis in HIV-positive patient: An unusual presentation. Indian J Dermatol Venereol Leprol 79: 109-111.
- Tseng HW, Chien SH, Wu CS, Tseng HH, Tseng CE (2010) Angiolymphoid hyperplasia with eosinophilia developing on antecedent welding burn: a case report. Kaohsiung J Med Sci 26: 266-269.
- Naranje S, Mittal R, Kumar A, Nataraj R (2009) Hemorrhagic prepatellar bursitis: a rare case report and review of the literature. Eur J Orthop Surg Traumatol 19: 281-284.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences