Effects of Local Skin Anaesthesia on Pain During Lumbar Puncture
1Department of Anesthesiology and Intensive Care, University Hospital Muenster, Muenster, Germany
2Department of Anesthesiology and Intensive Care, St. Franziskus Hospital Muenster, Muenster, Germany
- *Corresponding Author:
- Manuel Wenk
Department of Anaesthesiology and Intensive Care
Germany
E-mail: manuelwenk@uni-muenster.de
Received date: November 3, 2017; Accepted date: December 7, 2017; Published date: December 14, 2017
Citation: Wenk M, Massoth C, Weidlich S, Pöpping D M, Gurlit S, et al. (2017) Effects of local skin anaesthesia on pain during lumbar puncture. J Anaesthesiol Crit Care. Vol 1 No.1:1.
Copyright: ©2017 Massoth C, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited
Abstract
Background: Although spinal anaesthesia has a more favourable risk-profile, patients prefer surgery under general anaesthesia. Besides fear of severe but rare neurological complications, reasons for rejection are fear of backache or anticipated pain during puncture. Providing local anaesthesia before lumbar puncture is not a standard procedure. The aim of this randomized clinical trial was to evaluate the efficacy in pain reduction and the effect on patient satisfaction when using different local anaesthetic treatments before puncture.
Methods: 83 patients receiving spinal anaesthesia were randomly allocated to three subgroups: group I (control) did not receive any local anaesthetic pre-treatment of the skin, group II (EMLA) received EMLA patch and group III (Prilocaine) received local skin infiltration using 2 ml of Prilocaine prior to lumbar puncture. Pain during puncture, duration of procedure, comparison of expected versus actual pain as well as future decision for or against spinal anaesthesia was assessed.
Results: Pain during puncture was significantly reduced in the EMLA and Prilocaine groups as compared to patients in the control group. No significant differences between the EMLA and Prilocaine groups were detected, though pain scores were slightly lower in the EMLA-group. Duration of procedure was significantly longer in the Prilocaine-group as compared to the EMLA-group. Although pain was significantly higher in the control group, there was no significant difference between the groups regarding future acceptance of spinal anaesthesia.
Conclusion: Irrespective of the type (EMLA or Prilocaine), the use of local anaesthetic pre-treatment of the skin was found to significantly reduce pain during puncture. Our data supports the use of local anaesthesia prior to spinal puncture in daily routine. There was a trend towards better pain control in the EMLA-group; however, the actual pain in all groups was not clinically relevant in terms of decision for or against future spinal anaesthesia.
Keywords
Regional anaesthesia; Spinal anaesthesia; Analgesic techniques; Anaesthetics local
Introduction
Spinal anaesthesia is a simple, straightforward and safe method for surgery of the lower body that provides profound sensory and motor block by single-shot application of local anaesthetics into the subarachnoidal space, hence providing all benefits of an awake and spontaneously breathing patient. Side effects such as hypotension can usually be foreseen and handled by an experienced anaesthesiologist. Based on the common use of fine (25-27G) and atraumatic pencil point needles the rate of post-dural-puncture headache is distinctly diminished [1-3]. Although severe complications are rare [4-8] and the benefits usually outweigh the risks by far, patients’ acceptance of undergoing surgery under spinal anaesthesia as compared to general anaesthesia is considerably lower [9]. The main reasons for rejecting neuraxial block are –besides the dread of neurological aftermath- fear of any kind of backache as well as the anticipated pain associated with the lumbar puncture [10-12]. In the multimorbid patient preference for regional anaesthesia is associated with better patient outcome compared to general anaesthesia and its accompanying risks [13-15].
There is no general recommendation for providing local infiltration anaesthesia of the skin and subcutaneous tissue before lumbar puncture and its application in daily routine depends on internal clinical standards.
Despite the common administration of spinal anaesthesia, data regarding the effectiveness of various local anaesthetic applications before lumbar puncture are scarce and there is no data available investigating potential future decision for or against spinal anaesthesia. The comparison of local anaesthetic infiltration versus the application of a Eutectic Mixture of Local anaesthetics skin patch (EMLA, containing Prilocaine/Lidocaine) versus placebo before a dermal puncture points to a superior efficacy of the EMLA patch [16-19].
The aim of this trial was to evaluate the efficacy of integrating local anaesthetic pre-treatment in the perioperative procedure to achieve a decrease in pain during puncture and simultaneously to investigate whether pain during puncture has an influence on choosing spinal anaesthesia again in the future.
Methods
This randomized study was approved by the Ethics committee of the University Muenster (2015-350-f-S) and all participants gave written informed consent.
87 patients receiving spinal anaesthesia for vascular or orthopedic surgery during a 3 months study period at St. Franziskus-Hospital, Muenster, were included in the study. Patients with methemoglobinemia, Glucose-6-phosphate dehydrogenase deficiency, confirmed allergies against local anaesthetic agents, coagulopathies and age <18 years were excluded. Demographic data of all patients including sex, age, height, weight, BMI, ASA state, pre-existing affections of the spine and previous administration of spinal anaesthesia was collected.
Patients were randomly allocated to one of the following three groups: Group I (control) did not receive any local anaesthetic treatment prior to lumbar puncture, group II (EMLA) received EMLA patch for at least 60 min prior to lumbar puncture and group III (prilocaine) received local skin und subcutaneous tissue infiltration with 2 ml of prilocaine using a 22G needle (Sterican 30 mm, B. Braun, Melsungen, Germany).
For group II time of application, length of application and removal time of EMLA patch before spinal puncture were recorded and all patients were checked for potential local skin reactions.
Irrespective of group allocation no patient received premedication. Spinal anaesthesia was administered with a 25 G pencil point needle through a 20 G guidance cannula (Pencan Pro Set, B. Braun, Melsungen, Germany).
Total time of procedure was measured as well as the number of attempts to successfully place a spinal puncture. Patients assessed intensity of pain during puncture by visual analogue scale (VAS) and rated it as greater or less than expected. No separated evaluation of pain scores for local infiltration and spinal needle insertion in group 3 was assessed, as patients’ clear differentiation between needles for skin infiltration vs. spinal needle turned out to be restricted.
In addition, future decision towards spinal anaesthesia was surveyed postoperatively.
Statistical analysis was performed using IBM-SPSS version 24.0. Homogeneity of variance of the current population was assessed applying Levene’s test. Analysis of variance was executed to examine the differences among group means. Group-specific differences concerning person-related features and the dependent variable were assessed using univariate ANOVA. Post-hoc-analysis was performed using Scheffé’s method. Effect sizes were calculated using equation of effect size according to Bortz & Döring: (M1-M2)/[(SD1* N1+SD2* N2)/ (N1+N2)] and considered as small (d ≥ 0.2), medium (d ≥ 0.5) or large (d ≥ 0.8) [20,21].
Dichotomous dependent variables were surveyed for differences using contingency tables and chi-squared-test.
Results
Data from 83 patients was included. 4 patients were excluded from the study: 2 patients had received EMLA patch <60 min before puncture, 1 patient received >2 ml prilocaine skin infiltration and 1 patient had a vagal syncope during puncture who was then unable to participate further. (Group =29, Group II =27, Group III =27), 62.7% of participants were women (Control: 55.17%, EMLA: 62.96%, Prilocaine: 70.37%, Chi2 test: 1.382, p=0,5). As expected there were no significant differences in subgroups regarding age, sex, BMI, ASA-state and previous spinal anaesthesia (Table 1). Only one patient had a history of prior spinal surgery.
| Variable | Group | Mean | SD | F | P | Effect Size |
|---|---|---|---|---|---|---|
| Age | 2.188 | 0.119+ | ||||
| 1 | 61.28 | 15.21 | ||||
| 2 | 67.56 | 13.68 | ||||
| 3 | 68.19 | 12.02 | ||||
| BMI | 0.096 | 0.908+ | ||||
| 1 | 28.13 | 6.67 | ||||
| 2 | 27.51 | 4.05 | ||||
| 3 | 27.91 | 4.77 | ||||
| ASA | 0.635 | 0.532+ | ||||
| 1 | 2.00 | 0.60 | ||||
| 2 | 2.11 | 0.58 | ||||
| 3 | 2.19 | 0.68 | ||||
| Previous SPA | 0.404* | |||||
| 1 | 17 | 0 | ||||
| 2 | 11 | 0 | ||||
| 3 | 14 | 0 | ||||
| Number of attempts | 0.169 | 0.845+ | ||||
| 1 | 1.52 | 0.83 | ||||
| 2 | 1.41 | 0.75 | ||||
| 3 | 1.52 | 0.85 | ||||
| 1 vs. 2 | 0.88+ | |||||
| 1 vs. 3 | 1.0+ | |||||
| 2 vs. 3 | 0.88+ | |||||
| Duration of puncture | 4.103 | 0.02+ | ||||
| 1 | 4.39 | 2.07 | ||||
| 2 | 4 | 2.51 | ||||
| 3 | 5.63 | 1.94 | ||||
| 1 vs. 2 | 0.80+ | |||||
| 1 vs. 3 | 0.11+ | |||||
| 2 vs. 3 | 0.03+ | 0.73 |
Table 1: Patient characteristics and procedural data.
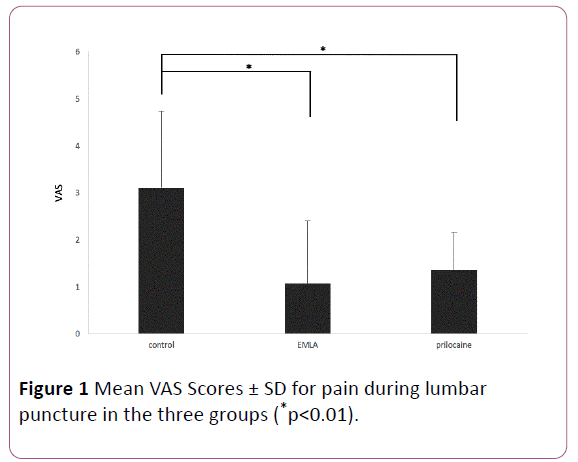
Significant reductions in VAS scores was achieved in group II (EMLA) (VAS mean 1.06 ± 1.33; p<0.01) and Group III (Prilocaine) (VAS mean 1.35 ± 0.8; p<0.01) as compared to group I (control) (VAS mean 3.1 ± 1.62) (Figure 1). Differences in VAS scores between Group II (EMLA) and Group III (Prilocaine) were not significant, but there was a trend towards slightly lower VAS scores in the EMLA-Group.
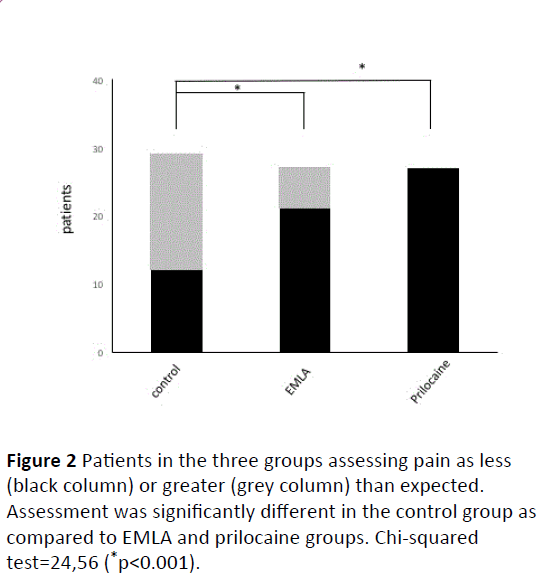
Similar to the VAS scores, pain intensity (greater or less than expected) was rated significantly lower in group II and II in relation to group I (control) (Chi-squared test=24,56 (p<0.001), (Figures 1 and 2). Calculated effect size between group I and group II and group I and III was large according to Cohen with 1.38 and 1.43, respectively (Table 1).
Mean exposure to EMLA amounted to 226 ± 96.7 min (minimum 60 min), 10/27 subjects developed local erythema.
There were no group differences regarding the number of attempts to successful spinal puncture, but the total procedure time was significantly longer in Group III (Prilocaine) (5.63 ± 1.94 min) in comparison to Group II (EMLA) (mean duration (4.0 ± 2.51 min) (Table 1).
95.2% of all participants when asked would choose spinal anaesthesia again for future surgery, hence no significant differences regarding refusing the procedure were detected between groups.
Discussion
Though the efficacy of local anaesthetic application prior to skin punctures has been shown previously [16,17,19,22] there is no general recommendation for such procedure during lumbar puncture.
Our data demonstrates a significant reduction in pain scores as compared to no local anaesthetic when local anaesthetic pretreatment before lumbar puncture with either local anaesthetic infiltration of the skin or application of an EMLA patch was used.
Most trials comparing local infiltration versus application of EMLA-patch prior to dermal puncture resulted in a superior efficacy of EMLA-patch [16-19]. Duration of application is crucial for sufficient efficacy of an EMLA patch since maximum analgesia is only received after a 90-minutes treatment, which was often not considered in earlier trials [23]. A survey from Ralston et al. showed an inferiority of the EMLA-patch to local infiltration, but duration of application was extremely short (mean 9 min), therefore a sufficient effect could not be expected [24].
Regarding pain during lumbar puncture, no significant differences between group II (EMLA) and group III (Prilocaine) were detected, but mean values of VAS scores in group II were slightly lower. Even though we did not reach statistical significance, a superior efficacy of EMLA is consistent with data from most preliminary surveys [16,17,19]. In our study, some variance regarding exposure times to EMLA before puncture was unavoidable since this trial took place in a clinical setting, subjected to the variability of OR times. However, considering the pharmacokinetics of EMLA a minimum application time of 60 min should be met and this was fulfilled in all patients. Nevertheless, the differences in total application time may have led to an attenuated analgesic effect in the individual patient. Overall, the usage of EMLA patches requires meticulous advanced planning in daily clinical routine, as at OR time minus 60 min (defined as the minimum application time) the patient may be still on the ward.
Interestingly, duration of lumbar puncture was significantly prolonged in group III (Prilocaine) in comparison to group II (EMLA) in our trial. The difference between group III (Prilocaine) and group I (control) was not significant, but mean duration of administration of spinal anaesthesia was significantly longer in group III as compared to group II and group I.
A possible masking of anatomical structures by local anaesthetic infiltration causing difficulties to perform lumbar puncture has been discussed but never investigated. However, considering the number of attempts required to successfully site an intrathecal needle, there were no significant differences in the number of attempts between groups, hence we could find no evidence for this hypothesis. Further investigations are needed to evaluate the impact of local anaesthetic infiltration on conditions of spinal anaesthesia. No other factors associated with more difficult conditions were observed in this study population such as extreme obesity and only one patient reported previous spinal surgery [25,26].
Overall, potential acceptance of further spinal anaesthesia in the future was high (95%). There were no significant differences between groups. Only 4 out of 83 patients would decline spinal anaesthesia and instead choose general anaesthesia for future surgery. This finding is supported by earlier data showing an overall high rate of acceptance of spinal anaesthesia after a previous successful attempt (98.5%; 96.3%) [10,17].
As previously suggested by Koscielniak et al. [11], our trial has confirmed that actual pain during puncture is only a minor determinant for acceptance of spinal anaesthesia similar to Gajraj et al. [17] who found fear of backache (33%) and fear of needle (28%) as most frequent answers in an interview in an obstetric population who had refused regional anaesthesia.
Other reasons for refusing future spinal anaesthesia have been described such as more than three puncture attempts, paresthesia at puncture as well as postoperative nausea and vomiting. Interestingly, overall dissatisfaction rate of spinal anaesthesia was only 3.7% [10].
In general, detailed information including patient’s selfeducation using informational web pages about anesthetic procedures is important for patient’s choice, since patients’ decision for or against neuraxial anaesthesia is altered by increased knowledge about anaesthesia [27].
Conclusion
Fear of both pain and neurological damage during lumbar puncture are two of the main determinants affecting patients’ acceptance of first time spinal anaesthesia. Even though there may be pain as high as NRS 5 during puncture, this, however, does not affect the overall decision for or against future spinal anaesthesia. This is most probably due to the fact that the spinal anaesthesia has numerous other advantages for the patient as compared to general anaesthesia that make pain during puncture only a minor component in the decision process. Our data shows that pain during lumbar puncture can be significantly reduced through prior application of local anaesthetics irrespective of the type (EMLA patch or Prilocaine skin infiltration). Therefore, we recommend the liberal use of local anaesthesia as a patch or infiltration technique prior to lumbar puncture in daily routine.
References
- Tsen LC, Hepner DL (2006) Needles used for spinal anaesthesia. Expert Rev Med Devices 3: 499-508.
- Srivastava V, Jindal P, Sharma JP (2010) Study of post dural puncture headache with 27 g quincke & whitacre needles in obstetrics/non obstetrics patients. Middle East J Anaesthesiol 20: 709-718.
- Shaikh JM, Memon A, Memon MA, Khan M (2008) Post dural puncture headache after spinal anaesthesia for cesarean section: A comparison of 25 g quincke, 27 g quincke and 27 g whitacre spinal needles. J Ayub Med Coll Abottabad 20: 10-13.
- Hyderally H (2002) Complications of spinal anaesthesia. Mt Sinai J Med 69: 55-56.
- Limongi JAG, Lins RS de M (2011) Cardiopulmonary arrest in spinal anaesthesia. Rev Bras Anestesiol 61: 110-120.
- Zaric D, Christiansen C, Pace NL, Punjasawadwong Y (2005) Transient neurologic symptoms after spinal anaesthesia with lidocaine versus other local anaesthetics: A systematic review of randomized, controlled trials. Anesth Analg 100: 1811-1816.
- Pitkänen MT, Aromaa U, Cozanitis DA, Förster JG (2013) Serious complications associated with spinal and epidural anaesthesia in Finland from 2000 to 2009. Acta Anaesthesiol Scand 57: 553-564.
- Charuluxananan S, Thienthong S, Rungreungvanich M, Chanchayanon T, Chinachoti T, et al. (2008) Cardiac arrest after spinal anaesthesia in thailand: A prospective multicenter registry of 40,271 anaesthetics. Anesth Analg 107:1735-1741.
- Sosis MB, Parnass SM, McCarthy RJ, Braverman B, Watson G, et al. (1995) Spinal phobia: Survey results of patient attitudes and preferences regarding anaesthesia. J Clin Anesth 7: 389-394.
- Rhee WJ, Chung CJ, Lim YH, Lee KH, Lee SC (2010) Factors in patient dissatisfaction and refusal regarding spinal anaesthesia. Korean J Anesthesiol 59: 260-264.
- Gajraj NM, Sharma SK, Souter AJ, Pole Y, Sidawi JE, et al. (1995) A survey of obstetric patients who refuse regional anaesthesia. Anaesthesia 50: 740-741.
- Gomes B., Sa Couto P, Amadeu M (2013) Evaluation of patients’ discomfort regarding regional anaesthesia. Eur J Anaesthesiol 30: 133.
- Stundner O, Ortmaier R, Memtsoudis SG (2014) Which outcomes related to regional anaesthesia are most important for orthopedic surgery patients? Anesthesiol Clin 32: 809-821.
- Pugely AJ, Martin CT, Gao Y, Mendoza-Lattes S, Callaghan JJ (2013) Differences in short-term complications between spinal and general anaesthesia for primary total knee arthroplasty. J Bone Joint Surg Am 95: 193-199.
- Maurer SG, Chen AL, Hiebert R, Pereira GC, Di Cesare PE (2007) Comparison of outcomes of using spinal versus general anaesthesia in total hip arthroplasty. Am J Orthop (Belle Mead NJ) 36: E101-106.
- Sharma SK, Gajraj NM, Sidawi JE, Lowe K (1996) EMLA cream effectively reduces the pain of spinal needle insertion. Reg Anesth 21: 561.
- Koscielniak-Nielsen Z, Hesselbjerg L, Brushøj J, Jensen MB, Pedersen HS (1998) EMLA patch for spinal puncture. A comparison of EMLA patch with lignocaine infiltration and placebo patch. Anaesthesia 53: 1218-1222.
- Smith M, Gray BM, Ingram DAJ (1990) Double-blind comparison of topical lignocaine-prilocaine cream (Emla) and lignocaine infiltration for arterial cannulation in adults. Br J Anaesth 65: 240-242.
- Elson JA, Paech MJ (1995) EMLA cream prior to insertion of elective epidurals. Anaesth Intensive Care 23: 339-341.
- Bortz J, Döring N (2006) Research methods and evaluation for human and social scientists. Springer-Verlag Berlin Heidelberg, p: 900.
- Cohen J (1988) Statistical power analysis for the behavioral sciences. Stat Power Anal Behav Sci 2: 567.
- Kelsaka E, Guldogus F, Sarihasan B, Tepe Ş (2006) Comparison of EMLA and lidocaine with or without sodium bicarbonate in prevention of spinal needle insertion pain. Anestezi Derg 14: 76-79.
- Bjerring P, Arendt-Nielsen L (1990) Depth and duration of skin analgesia to needle insertion after topical application of EMLA cream. Br J Anaesth 64: 173-177.
- Ralston SJ, Head-Rapson AG (1993) Use of EMLA cream for skin anaesthesia prior to epidural insertion in labour. Anaesthesia 48: 65-67.
- Ruzman T, Gulam D, Drenjancevic IH, Venžera-Azenić D, Ruzman N, et al. (2014) Factors associated with difficult neuraxial blockade. Local Reg Anesth 7: 47-52.
- Kim H-J, Kim WH, Lim HW, Kim JA, Kim DK et al. (2015) Obesity is independently associated with spinal anaesthesia outcomes: A prospective observational study. PLoS One 10: e0124264.
- Groves ND, Humphreys HW, Williams AJ, Jones A (2010) Effect of informational internet web pages on patients’ decision-making: Randomised controlled trial regarding choice of spinal or general anaesthesia for orthopaedic surgery. Anaesthesia 65: 277-282.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences