Effective Management of a School-Acquired Cardiac Wound in a Hospital with Limited Resources: A Case Report and Review of the Literature
Lamboni D1*, Koulekey D1, Sama H2, Barnabo-Nampoukine K3, Issa-Toure A1 and Sakiye A1
1Department of Surgery and Surgical Specialties, CHU Sylvanus Olympio, University of Lome, Lome, Togo
2Department of Anaesthesia and Intensive Care, CHU Sylvanus Olympio, University of Lome, Lome, Togo
3Department of Cardiothoracic and Vascular Surgery, Tongji Medical College, Huazhong University of Science and Technology, Wuhan, China
*Corresponding Author:
- Lamboni D
Department of Surgery and Surgical Specialties, CHU Sylvanus Olympio, University of Lome, Lome, Togo
E-mail: damsane@yahoo.fr
Received date: September 28, 2023, Manuscript No. IPJETC-23-17961; Editor assigned date: October 02, 2023, PreQC No. IPJETC-23-17961 (PQ); Reviewed date: October 16, 2023, QC No. IPJETC-23-17961; Revised date: January 02, 2025, Manuscript No. IPJETC-23-17961 (R); Published date: January 09, 2025, DOI: 10.36648/IPJETC.9.1.057
Citation: Lamboni D, Koulekey D, Sama H, Barnabo-Nampoukine K, Issa-Toure A, et al. (2024) Effective Management of a School-Acquired Cardiac Wound in a Hospital with Limited Resources: A Case Report and Review of the Literature. J Emerg Trauma Care Vol:10 No:1
Abstract
Blunt objects in the school environment can cause serious injuries that can be life-threatening. We report the exceptional case of a thoracic wound caused by scissors in a teenager in haemodynamic shock. The patient rapidly benefited from a multidisciplinary approach involving cardiac and thoracic surgeons and a resuscitating anesthetist, all of whom helped to preserve the adolescent's vital prognosis.
Case report: The patient was a 14 years old schoolboy who presented with a scissors thoracic wound during a game in the playground. The wound was located in the 3rd left intercostal space. The patient presented with cardiac tamponade and was rapidly taken to the surgical emergency department of the Sylvanus Olympio university hospital in Lome by non-medical transport. Rapid recognition of the severity of the lesions by the medical team in the surgical emergency department enabled rapid management in the operating theatre, where haemostasis of a cardiac wound at the left atrio-ventricular junction was successfully performed a ter emergency sternothoracotomy without the need for extracorporeal circulation, which was unavailable in our centre.
Conclusion: Blunt objects can cause serious injury in schools. Our observation highlights the need to control and monitor the use of these objects in schools, and also to raise public awareness of the seriousness of thoracic wounds. The establishment of a surgical and anaesthesia/ cardiothoracic resuscitation team with an operating theatre equipped with extracorporeal circulation is imperative in the surgical emergency department of the CHU SO for effective management of these injuries, which are not incompatible with life.
Keywords
Cardiac injury; Life threatning; Limited resources
Introduction
Cardiac injury are defined as a break in continuity of the heart wall and/or the pericardial envelope. They are most often caused by thoracic wounds, and there are generally two types of vulnating agent: Knife wounds and firearm wounds. These are rare injuries, but are rapidly life-threatening, which is why treatment is absolutely urgent. Of these chest wounds, 40% will die at the scene of the accident, 30% in the first few hours and less than 10% will reach hospital alive [1]. The survival rate of patients varies in the literature from 19% to 73% [2] and depends on several factors. In Africa, given the shortage of human resources and healthcare equipment, few publications have been reported. In Togo, the first case of a heart sore resulting from a play accident was described in 2013 in a child [3]. We report a new case of heart injury occurring in the school playground with the aim of reviewing the literature and defining prognostic factors for successful management of these injuries.
Case Report
It was a boy of 14 years old primary school pupil who, during a fight at the 9.20 am recess, suffered a left hemithoracic wound caused by scissors brought back by a classmate. He immediately experienced severe chest pain, difficulty breathing and agitation. The school's teaching staffs were quickly alerted. The patient, accompanied by a teacher, was immediately referred at 10 am to the nearest University Hospital by non-medical transport.
On admission to the surgical emergency department at around 11 am, the first doctor seen noted the following:
- Altered general condition.
- Agitation with obnubilation and intolerable supine position (orthopnoea).
- Haemodynamic instability with arterial hypotension at 80/40 mmHg; regular tachycardia at 120 ppm with SpO at 95% on room air.
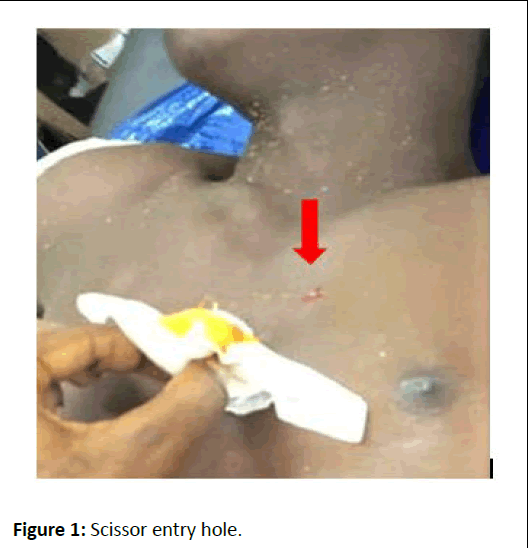
- On inspection, there was a thoracic wound in the 2 left intercostal space 2 cm from the sternum (Figure 1), muffled heart sounds (Figure 2).
- Pulmonary auscultation revealed a vesicular murmur that was well transmitted in both lung fields; there were no rules.
- Sphincter relaxation was also noted, with the emission of feces and urine as evidence of the vagal reaction, testifying to the severity of the lesion.
Figure 1: Scissor entry hole.
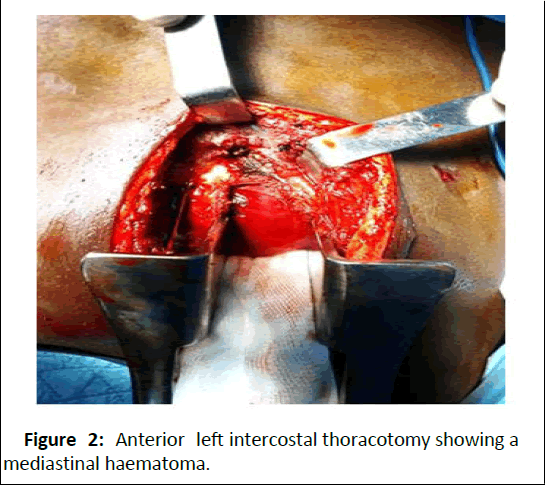
Figure 2: Anterior left intercostal thoracotomy showing a mediastinal haematoma.
The patient was immediately given emergency life-saving and resuscitation measures, including a slight proclivity position, multiparametric monitoring, high-concentration oxygen therapy by mask, two large-bore peripheral venous lines and urinary catheterisation. Vascular filling with 1 litre of crystalloid and 500 ml of macromolecules and noradrenaline by electric syringe improved systolic blood pressure to 110 mmHg. However, haemodynamic instability led to suspicion of a cardiac wound complicated by cardiac tamponade. An exploratory thoracotomy was performed as a matter of urgency.
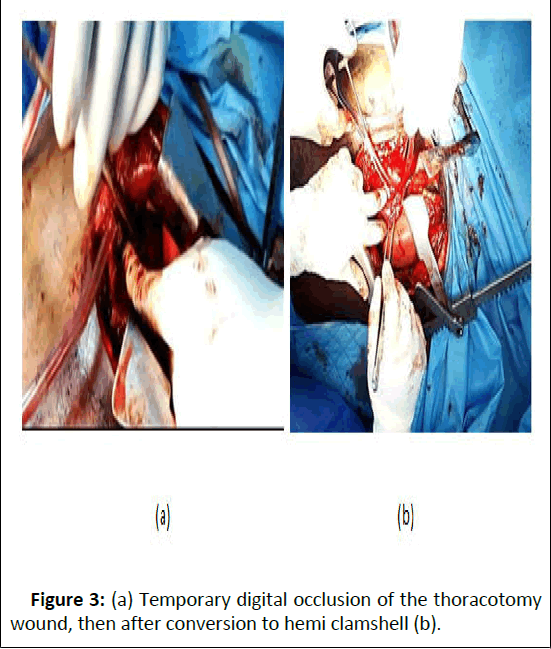
The patient was admitted to the operating theatre at 12:00. A left anterior thoracotomy was performed through the 4th left intercostal space (Figure 3). The operation was performed under total intravenous general anaesthesia with ketamine, propofol, fentanyl and rocuronium in titration with orotracheal intubation. After opening the pericardium, we evacuated approximately 400 CC of blackish blood. A wound measuring approximately 0.5 cm at the base of the left ventricle with a jet of blood was observed. The surgeon temporarily occluded the wound with his index finger. A hemiclamshell conversion (Figure 4) was performed with suspension of the pericardium.
Figure 3: (a) Temporary digital occlusion of the thoracotomy wound, then after conversion to hemi clamshell (b).
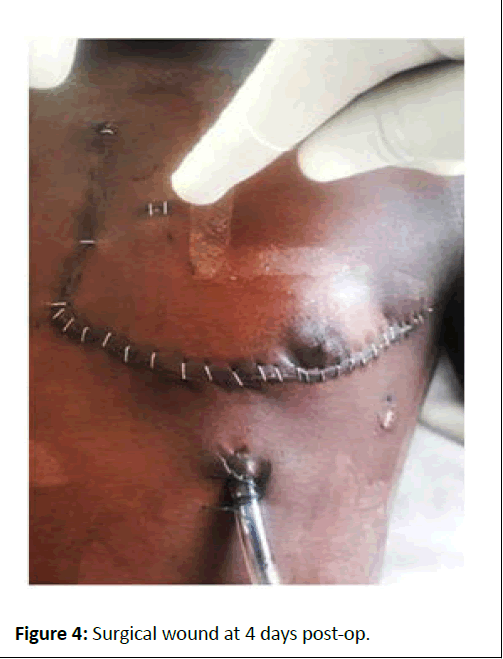
Figure 4: Surgical wound at 4 days post-op.
Stitches applied to a pericardial patch made it difficult to achieve haemostasis. Partial closure of the pericardium with a pleuropericardial window was performed, followed by double drainage of the pericardium and pleura, closure of the sternum with 4 steel wire stitches and closure of the thoracotomy. There was minimal pericardial effusion with the pericardial and pleural drains in place. The initial post-operative laboratory work-up showed cardiac enzymes CPK elevated to 20 N and Troponin to 6 N; hyperkalaemia of 6.7 was detected and rapidly corrected, with a gradual return to normal limits without recourse to dialysis. The post-operative chest X-ray showed no cardiomegaly or haemothorax, and the second cardiac ultrasound check showed no left ventricular dysfunction, a healthy septum and a healthy aortic valve. The rapid regression of the few metabolic disorders enabled the patient to be weaned off ventilation and extubated on the 3rd day in intensive care. On postoperative day 4 (Figure 4), he was transferred to the surgical ward, where he continued to receive antibiotic therapy, multimodal analgesia and electrolyte balance, with resumption of oral feeding. The drains were removed on postoperative day 5 and the patient was discharged on postoperative day 7; he was reviewed on postoperative day 14 and 30 with a satisfactory clinical, radiological, ultrasound and biological re-evaluation.
Results and Discussion
Injury to the heart is an extreme medical and surgical emergency, rapidly threatening a patient's vital prognosis. Approximately 20% of all patients who die from chest trauma do so as a result of cardiac injury. Half of those with cardiac injuries die on the spot and a further 33% die during initial transport or on arrival at A and E. Of patients who reach hospital alive, 63% survive until discharge [4]. Patients' chances of survival depend essentially on the speed of management, which depends on the existence of a management protocol [5]. In our case and that of Gnassingbe, et al., these DCPs occurred in children as a result of intentional injury and a play accident respectively [3]. In their series, Goz, et al., found an average age of 12.94 ± 3.52 years, with a preponderance of penetrating injuries in play accidents involving incisive/penetrating tools [6].
This highlights the need for parents to be informed and educated about blunt and dangerous objects in the play and living environment in early childhood, and also the importance of parental control over societal phenomena, particularly violent games and films. The responsibility of teachers in schools can also be engaged. The prognosis for DCP depends on a number of factors reported in the Ivatury classification [7], modified by the Bogota classification [2]. It is a race against time, because the prognosis depends essentially on the speed of diagnosis and management. The dogma of considering "any wound in the cardiac area as a heart wound until proven otherwise" makes it possible to implement rapid management, especially in countries with limited resources. Therefore, on admission, all patients presenting with haemodynamic shock should immediately benefit from damage control resuscitation measures according to Advanced Trauma Life Support (ATLS) [4]. Damage control surgery in cardiac trauma must therefore be taught to general surgeons in order to give the rare patients arriving alive at hospital a chance of survival. Patients with haemodynamic stability may benefit from imaging studies as shown in Table 1, as the classic Beck's triad clinical presentation (muffled heart sounds, jugular engorgement and hypotension) suggestive of cardiac tamponade is only found in 10% to 30% of confirmed cases [8,9]. With this in mind, the test of choice for diagnosing impending cardiac tamponade is thoracic ultrasound, which has a sensitivity of 79%, a specificity of 92% and a negative predictive value of 95% [10].
Fast echography is now a must in emergency departments in hospitals with limited resources. In the absence of an ultrasound scan, an aggressive surgical approach should be adopted, involving a diagnostic pericardial window with rapid conversion to thoracotomy or sternotomy if the surgeon finds a blood flow. The choice of approach varies during conversion. For example, a median sternotomy allows better exposure of mediastinal structures, but access is longer than that of an anterolateral thoracotomy. As a general rule, if the injury is located between the nipples, a median sternotomy is the best approach to the mediastinal structures; however, if the injury is located laterally to the nipples, a right or left anterolateral thoracotomy is preferable [11]. Finally, in hospitals with limited resources such as ours; damage control resuscitation and surgery, fast echography and the pericardial window must be taught to general surgeons. The success of rescue thoracotomies or sternotomies also depends on the formation of a surgical, emergency and intensive care anaesthesia team.
| Â CShest X-ray | Â Cardiac ultasonography | Attitude |
|---|---|---|
| Negative | Negative | Monitored surveillance, repeat examination in 3-6 hours. |
| Positive | Negative | Drainage pleural. |
| Negative | Positive | Sub-xiphoid pericardial drainage. |
| Positive | Positive | VATS pericardial window, open surgery based on clinical judgment and pericardial window results. |
Table 1: Therapeutic attitude guided by chest X-ray and cardiac ultrasound in haemodynamically stable patients.
Conclusion
Heart wounds are extremely urgent situations with an appalling prognosis. However, this prognosis can be improved by rapid management of patients through rapid recognition of these injuries, medical transport, control of damage control in intensive care and surgery, availability of fast ultrasound and a minimum of equipment essential for cardiac and thoracic surgery in operating theatres in countries with limited resources.
Financial Support and Sponsorship
Nil.
Conflicts of Interest
There are no conflicts of interest.
Ethical Consideration
The patient has given his or her consent for his or her observation to be submitted anonymously.
References
- Campbell NC, Thomson SR, Muckart DJ, Meumann CM, van Middelkoop I, et al. (1997) Review of 1198 cases of penetrating cardiac trauma. J Br Surg 84:1737-1740
[Google Scholar] [PubMed]
- Pulido JA, Reyes M, Enriquez J, Padilla L, Perez C, et al. (2022) Predicting mortality in penetrating cardiac trauma in developing countries through a new classification: Validation of the Bogota classification. Health Sci Rep 5:e915
[Crossref] [Google Scholar] [PubMed]
- Gnassingbe K, Simlawo K, Egbohou P, Noumedem NB, Mama AW, et al. (2013) Cardiac injury in child managed successfully in underprivileged hospital of Africa. World J Pediatr Cong 305-307
[Crossref] [Google Scholar] [PubMed]
- Hadad GA, Ordonez CA, Parra MW, Caicedo Y (2021) Damage control in penetrating cardiac trauma. Colomb Med 52:e4034519
- Lee A, Hameed M, Kaminsky M, Chad G (2023) Penetrating cardiac trauma. Surg Open Sci 11:45â??55
- Goz M, Cakir O, Eren MN (2010) Penetrating cardiac trauma in children. Turk J Emerg Surg 16:220-224
[Google Scholar] [PubMed]
- Ivatury RR, Rohman M, Steichen FM, Gunduz Y, Nallathambi M, et al. (1987) Penetrating cardiac injuries: Twenty-year experience. Am Surg 53:310-317
[Google Scholar] [PubMed]
- Hadad GA, Garcia AF, Serna JJ, Herrera MA, Morales M, et al. (2020) The role of ultrasound for detecting occult penetrating cardiac wounds in hemodynamically stable patients. World J Surg 44:1673-1680
[Crossref] [Google Scholar] [PubMed]
- Ariyarajah V, Spodick DH (2007) Cardiac tamponade revisited: A postmortem look at a cautionary case. Tex Heart Inst J 34:347
[Google Scholar] [PubMed]
- Vinck EE, Angel EP, Barrios RV, Martinez SI, Arias CA, et al. (2021) Video-assisted thoracoscopy for penetrating cardiac box injury in stable patients. Braz J Cardiovasc Surg 36:550-556
[Crossref] [Google Scholar] [PubMed]
- Nicol AJ (2018) Cardiac hemorrhage: Treatment of the bleeding heart. Treatment of ongoing hemorrhage: The art and craft of stopping severe bleeding. 2018:67-80
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences