Clinical and Genetic Diagnosis of Pheochromocytoma and Paraganglioma
Marina Yukina1, Ekaterina Troshina1, Dmitry Beltsevich2 and Nurana Nuralieva3*
1Department of Therapeutic Endocrinology, Endocrinology Research Centre, Moscow, Russian Federation
2Department of Surgery, Endocrinology Research Centre, Moscow, Russian Federation
3Institute of Professional Education of Doctors, Endocrinology Research Centre, Moscow, Russian Federation
- *Corresponding Author:
- Nurana Nuralieva
Institute of Professional Education of Doctors
Endocrinology Research Centre
Moscow, Russian Federation
Tel: 89160151017
E-mail: NNurana@yandex.ru
Received Date: 15 March 2017; Accepted Date: 05 April 2017; Published Date: 12 April 2017
Citation: Yukina M, Troshina E, Beltsevich D, et al. Clinical and Genetic Diagnosis of Pheochromocytoma and Paraganglioma. Endocrinol Res Metab. 2017, 1: 1.
Copyright: © 2017 Yukina M, et al. This is an open-access article distributed under the terms of the creative Commons attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Pheochromocytomas are rare tumors of the adrenal medulla and extra-adrenal sympathetic chromaffin tissues. This study investigates the clinical and genetic features of pheochromocytoma. Methods: We analyzed records of 167 patients diagnosed with pheochromocytomas. Patients were divided into three groups, as follows: group 1 – patients with multiple endocrine neoplasia type 2; group 2 – patients with von Hippel-Lindau Syndrome; group 3 – patients with sporadic pheochromocytoma. Findings: The average age at the time of initial diagnosis was 25 years in group 1, 18 years in group 2 and 47 years in group 3. The predominant secretion of epinephrine was associated with the multiple endocrine neoplasia type 2, the predominant secretion of norepinephrine was associated with von Hippel-Lindau syndrome and the mixed secretion was associated with sporadic pheochromocytoma. There was a positive relationship between the tumor sizes and excretion of methylated metanephrines in group 1. All tumors of this group were localized in adrenals (82% of pheochromocytomas were bilateral and 58% of pheochromocytomas were multifocal). In group 2 16.4% of patients had extraadrenal tumor localization, at 6.6% of patients had metastases. In groups 1 and 3 no metastases were found. Conclusion: These data suggest that genetic testing should be recommended in patients younger than 40 years, in patients with bilateral and multifocal tumors and in patients with family history of pheochromocytoma. The predominant production of norepinephrine makes the diagnosis of multiple endocrine neoplasia type 2 unlikely. In patients with multiple endocrine neoplasia type 2 and the predominant production of epinephrine the search for the metastases and extra-adrenal tumor localization is inappropriate.
Keywords
Catecholamine; Multiple endocrine neoplasia type 2; Paraganglioma; Pheochromocytoma; Von hippel-lindau syndrome
List of Abbreviations
MTC: Medullary Thyroid Cancer; MEN 2: Multiple Endocrine Neoplasia Type 2; SPCC: Sporadic pheochromocytoma; VHL: Von Hippel-Lindau Disease; FTP: Federal Target Program
Introduction
Recent data have clearly demonstrated, that hereditary cause of chromaffin tumors is much more prevalent (30-42% of patients) than previously thought (10% of patients) [1-3]. Hereditary pheochromocytomas are attributable to pathogenic variants in RET, VHL, NF1, SDHD, SDHC and SDHB. Some hereditary pheochromocytomas are associated with increased risk of malignancy and tumor recurrence. In such patients the general condition and prognosis of the disease are burdened by co-existing tumor pathology. Timely diagnosis of pheochromocytoma and concomitant syndromes determine the prognosis of disease, further tactics of treatment and observation of patients.
Researchers are still debating about the spectrum of genetic testing in patients with pheochromocytoma. Testing of all tumor susceptibility genes in all patients with pheochromocytoma is economically infeasible. In this regard, the determination of phenotypic characteristics of hereditary diseases (clinical picture, secretory and topical features of a tumor) plays an important role in planning for genetic testing.
Currently, there is no consensus regarding the volume of surgical intervention in patients with hereditary pheochromocytoma. Partial adrenalectomy is associated with a significantly increased risk of local tumor recurrence (in hereditary syndrome each chromaffin cell has a high tumor potential). The re-interventions are associated with a significantly increased risk of intra- and postoperative complications. On the other hand, the total bilateral adrenalectomy (in patients with bilateral pheochromocytoma) is associated with the necessity for lifelong regular corticosteroid therapy and leads to a significant deterioration in the quality of life [4].
According to the literature data, the detection rate of metastatic lesions in patients with pheochromocytoma varies within wide limits – from 3% to 36%. There is no clear understanding of malignant potential in Multiple endocrine neoplasia type 2 (MEN 2) – from 0% to 10% [5]. Thus, the determination of metastatic potential of different genotypic lesions is topical. The prediction of malignant potential will help to establish an adequate monitoring algorithm.
Currently, the expensive imaging methods with different radiation exposure are being used for the determination of lesion extent: computed tomography scan, magneticresonance imaging, positron emission tomography, 123Imetaiodobenzylguanidine scintigraphy and others. However, the indications for each method of topical diagnosis and scope of the examination in different genetic variants of pheochromocytoma remain unclear.
Thus, multilateral analysis of genetically determined pheochromocytomas is necessary to develop the optimum medical tactics of this category of patients. The patients have been examined and operated on in the period 1979 to 2010. The diagnosis of pheochromocytoma was histologically confirmed in all cases.
Materials and Methods
This study was a retrospective comparative study of 167 patients with pheochromocytoma managed in Endocrinology Research Centre (ERC). The patients have been examined and operated on in the period 1979 to 2010. The diagnosis of pheochromocytoma was histologically confirmed in all cases. Patients were divided into three groups, as follows: group 1 (n=66) – patients with multiple endocrine neoplasia (MEN) type 2 (group 1); group 2 (n=61) – patients with von Hippel- Lindau Syndrome; group 3 (n=40) – patients with sporadic pheochromocytoma. The diagnosis was confirmed genetically and/or clinically (if patients have at least two classical components of syndrome the diagnosis may be confirmed clinically without genetic research). The group 3 included patients with unilateral pheochromocytoma without burden family medical history or any diseases, associated with hereditary pheochromocytomasyndromes.
The histology research of postoperative material has been confirmed in the Department of Pathomorphology of ERC. The tissues were stained with hematoxylin and eosin. For cortex verification the staining by Sudan Black or Sudan III has been used. The diagnosis was formulated according to WHO International Histological Classification of Tumors in the 1983 edition.
The molecular genetic testing was conducted in different genetic laboratories, including Laboratory of Department of hereditary endocrinopathy of ERC. The patients' blood was collected in tubes with EDTA. The DNA was extracted from peripheral blood leukocytes using QIAMP DNA mini kit (QIAGEN, Hilden, Germany). RET (exons 10, 11 ø 16) and VHL genes were analyzed using PCR with following sequencing.
The 24-hour urinary metanephrine and normetanephrine excretion was measured in the Laboratory of hormonal assay of ERC by enzyme immunoassay using the commercial kits of the IBL company (Germany) for metanephrine and normetanephrine.The 24-hour urine was collected with preservative in cold mode. The following normal ranges of methylated catecholamine derivatives 24-hour excretion were accepted: 20-312 μg for metanephrine and 30-440 μg for normetanephrine. These normal reference ranges have been elaborated on a random sample of general population.
The statistical analysis of the results was performed using standard methods of statistical analysis (Statistica 6.0). Descriptive statistics was used to summarize and describe the obtained data. Results are presented as median and interquartile range (IQR) boundaries; minimum-maximum and standard deviation are given if necessary (± SD). The quantitative data in the groups were tested for normal distribution using the Shapiro-Wilk test, and then tested the hypothesis of equality of variances using the Levene’s test. As in all cases the distribution was different from normal, nonparametric methods used in data analysis. To test the statistical hypotheses in the analysis of unrelated groups, the Mann-Whitney test has been used for quantitative traits and the χ2 with Yates' correction has been used for the quality traits. The identification of the measure of linear relationship between parameters was performed using Spearman's rank correlation. Differences were accepted as statistically significant at p<0.05.
The investigation was in accordance with the ethical standards of the responsible committee on human experimentation and with the Helsinki Declaration.
Results
By gender, patients in our study were as follows: 38% males and 62% females (n=64 and n=103 respectively; р<0.00001). In the group of patients with MEN 2 (n=66) 36% were male and 64% were female (n=24 and n=42 accordingly; р=0.0017). In the group of patients with Von Hippel-Lindau Disease (n=61) 53% were male and 47% were female (n=32 and n=29 accordingly; р>0.05). In the group of patients with sporadic pheochromocytoma (n=40) 20% were male and 80% were female (n=8 and n=32 accordingly; р<0.00001).
Molecular genetic testing determined the mutation at codon 634 of exon 11 in most of patients with MEN 2 (n=36) and at codon 918 of exon 16 (n=12), which characterized by the most aggressive course of medullary thyroid cancer (MTC): 67% and 22% accordingly. Patients with mutation at codons 611 (n=1), 791 (n=2) and with deletion at codons 632-636 (n=2) were also identified in our research.
In the group of patients with Von Hippel-Lindau Disease molecular genetic testing has been conducted in 15 patients: 2 patients had mutations at codon 157, 2 patients – at codon 161, 2 patients – at codon 163, 1 patient – at codon 167, 1 patient – at codon 213. 7 patients with Von Hippel-Lindau Disease had no mutations, confirming diagnosis. It is known that the sensitivity of the method for determining VHL gene mutation can be less than 85%. Thus, diagnosis of this pathology in patients without genetic examination/ confirmation was based on combination of 2 and more features, associated with these syndromes [6].
All patients in group 1 have had medullary thyroid cancer in their history. The first clinical manifestation of medullary thyroid cancer (nodular goiter) in patient with mutation at codons 918 and 634 has been revealed at 12 years, in patient with deletion at codons 632-636 – at 17 years, in patient with mutation at codon 791 – at 44 years and in patient with mutation at codon 611– at 54 years. The median age at the moment of thyroidectomy was 24 years (n=66; min/max 4-65 years; SD ± 15.99 years). The preventive thyroidectomy was performed in 1 four-year-old patient (mutation at codon 634) – the histopathology did not reveal the medullary carcinoma; at the time of the study (10 years post-thyroidectomy) calcitonin level was within normal range.
In our study the primary hyperparathyroidism has been diagnosed in 4 patients with MEN, the median age of diagnosis was 30 years (min/max 22-37 ûõт; SD ± 6.95 years). All of patients had mutation at codon 634, which corresponds to other studies: primary hyperparathyroidism as part of MEN 2 is most often associated with mutation at codon 634 of RET [7]. Because of the mild course of disease, the surgical treatment has not been performed.
It is known, that cutaneous amyloidosis (lichenoid) may indicate the presence of a mutation at codon 634 of RET [8]. In our study one patient with skin changes, previously interpreted as psoriasis, had mutation at codon 634. The patient in this regard received different treatment, including cytostatics (methotrexate), without any positive effect. After histological confirmation of cutaneous amyloidosis the symptomatic treatment was prescribed. Thus, the correct diagnosis obviates the necessity for lifelong debilitating therapy with cytotoxic and immunosuppressive drugs in these patients.
Patients with Von Hippel-Lindau Disease besides pheochromocytoma also had the following comorbidities: erythrocytosis (n=26), retinal angiomatosis (n=25), central nervous system hemangioblastomas (n=23), polycystic (n=10) and kidney cancer (n=3), tumors of pancreas (n=12) and 1 patient had Brugada syndrome.
We analyzed the comorbidities and erythrocytes level in the other groups. In the group of MEN 2 the erythrocytosis was diagnosed in 2 patients (р<0.00001), and polycystic of kidney was diagnosed in 1 patient (p=0.003). In the group of sporadic pheochromocytoma erythrocytosis was diagnosed in 3 patients (р=0.001), polycystic of kidney was diagnosed in 1 patient (р=0.03). There were no other components, associated with Von Hippel-Lindau Disease, in groups 1 and 3.
The analysis of indications for primary diagnosis of pheochromocytoma in the group 1 demonstrated that in 50% of patients (n=33) pheochromocytoma has been suspected based on clinical symptoms, in 30% (n=20) – after the diagnosis of medullary thyroid cancer. In 11% of patients (n=7) examination was initiated after revealing the adrenal incidentaloma and in 9% (n=6) pheochromocytoma has been diagnosed based on known family history. The targeted interviewing identified the burdened family history in 44% (n=29) of patients.
In group 2 the 80% of pheochromocytomas (n=49) have been suspected based on clinical symptoms. In 15% of patients (n=9) examination was initiated after revealing the adrenal incidentaloma and 5% (n=3) of pheochromocytomas have been diagnosed based on known family history. The targeted interviewing identified the burdened family history in 29% (n=18) of patients.
In 65% patients of the group 3 pheochromocytoma has been suspected based on clinical symptoms. In 35% of patients examination was initiated after revealing the adrenal incidentaloma. These data confirm the significant detection rate of adrenal incidentaloma currently.
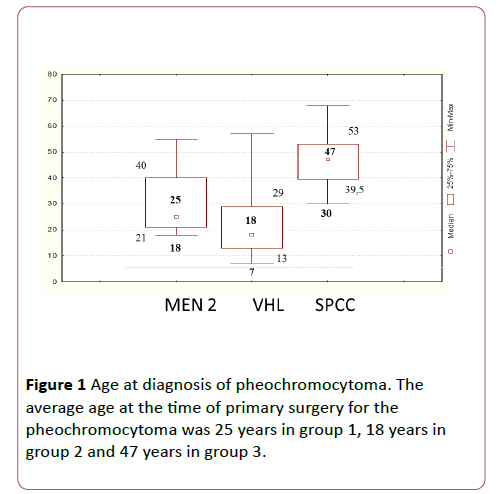
The age at primary surgical treatment of pheochromocytoma corresponded with the age at pheochromocytoma diagnosis verification. The median age at the time of primary surgery for the pheochromocytoma in patients with MEN 2 was 25 years (n=66; min/max 18-57 years; [21;40]; SD ± 11.6 years). The youngest age at surgery for the pheochromocytoma in patients of this group was 18 years.
The median age at the primary surgery for pheochromocytoma in patients with Von Hippel-Lindau Disease, was 18 years (n=61; min/max 7-57 years; [13;29]; SD ± 11.63 years). The youngest age at surgery for the pheochromocytoma in patients of this group was 7 years.
The median age at primary surgery for the pheochromocytoma in patients with sporadic pheochromocytoma was 47 years (n=40; min/max 30-68 years; [39.5;53]; SD ± 9.64 years). The youngest age at surgery for the pheochromocytoma in patients of this group was in 30 years (Figure 1).
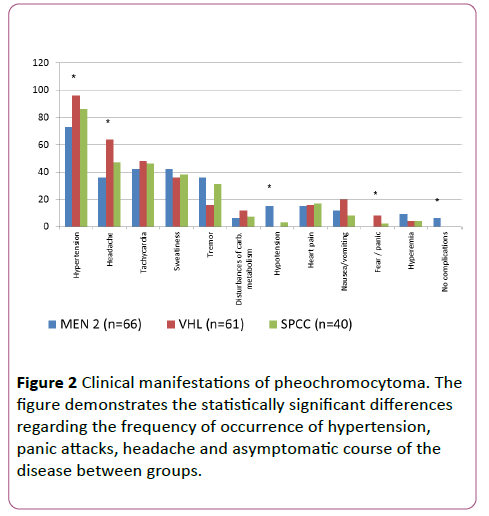
In our investigation we had the statistically significant differences regarding the frequency of occurrence of hypertension and panic attacks between groups. Hypertension and panic attacks have been more common in patients with Von Hippel-Lindau Disease. Headache has been often observed in patients with Von Hippel-Lindau Disease and sporadic pheochromocytoma. Episodes of hypotension or lack of any clinical symptoms are more common in patients with MEN 2 (Figure 2).
Analysis of patients with MEN 2 without clinical manifestations of pheochromocytoma demonstrated, that tumor size in that patients did not exceed 2 cm. We supposed that small tumors have a low secretory activity. For confirming this hypothesis we conducted correlation analysis between the tumor size and values of methylated catecholamines.
Analysis of methylated catecholamines excretion levels demonstrated, that patients from group 1 have predominantly epinephrine type of secretion (metanephrine type of excretion; it means, that in most cases metanephrine level exceeded normetanephrine level (82/18%; р<0.00001)). We also revealed, that in this group the metanephrine level, on the average, exceeded 6.6 times the upper limit of normal (average amplitude/multiplicity of exceeding the upper limit of normal in the group) (2285 μg/day), and the normetanephrine level exceeded 3.7 times the upper limit of normal (1628 μg/ day).
Patients of group 2 have predominantly norepinephrine type of secretion (normetanephrine type of excretion): in all cases (100%) the normetanephrine level exceeded the metanephrine level. We also revealed, that in patients of this group the metanephrine level, on the average, exceeded 1.04 times the upper limit of normal (358 μg/day), and the normetanephrine level exceeded 14.5 times the upper limit of normal (6389 μg/day).
Patients of the group 3 had no predominant type pf secretion (mixed type): patients had as adrenaline and noradrenaline type of secretion almost equally (52% and 48% respectively, р>0.05). Also, the metanephrine level, on the average, exceeded 8.3 times the upper limit of normal (2877 μg/day), and the normetanephrine level exceeded 9.3 times the upper limit of normal (4100 μg/day).
For determination the correlation between tumor size and level of secretion the analysis of the size of tumor nodule and tumor tissue has been conducted. Thus, in the group 1 the size of tumor nodule consisted 3 cm (ÃÂϛ) (n=140 [2; 4.5] min/max 0.7 -10; SD 1.71), in the group 2 – 3.3 cm (ÃÂϛ) (n=139[2.29; 5] min/max 1 -8; SD 1.73), in the group 3 – 4.5 cm (ÃÂϛ) (n=40[4; 5.5] min/max 2.5-12; SD 1.92). We obtained statistically significant differences between groups in the size of tumor node: between 1 and group 2s р=0.019, between 1 and group 3s р<0.0000001, between 2 and group 3s р=0.00018.
We estimated the size of tumor tissue (the sum of the diameters of the tumor nodules) for patients with multicentric variant of pheochromocyoma. The size of tumor tissue was 3.5 cm (ÃÂϛ) (n=17 [2; 6.7] min/max 1 -18.5; SD 4.71) in group 1, 6.75 cm (ÃÂϛ) (n=18 [4.5; 11.5] min/max 2 -20; SD 4.65) in group 2. There was no multicentric variant in group 3 (n=40), that’s why the size of tumor tissue corresponded to the tumor size – 4.5 cm (ÃÂϛ).
There were no statistically significant differences between the groups regarding size of tumor tissue: р ≥ 0.05. We determined the size of tumor tissue and then examined the correlation between methylated catecholamine derivatives levels and size of tumor (tumor tissue). The time difference between hormonal assay (methylated catecholamine derivatives levels) and determination the size of tumor did not exceed 17 days.
There were no correlation between the methylated catecholamine derivatives levels and size of tumor tissue in groups 2 and 3. In the first group we revealed positive correlation between the size of tumor tissue and excretion levels of metanephrine (r=0.77; p=0.0003), normetanephrine (r=0.75; p=0.0006).
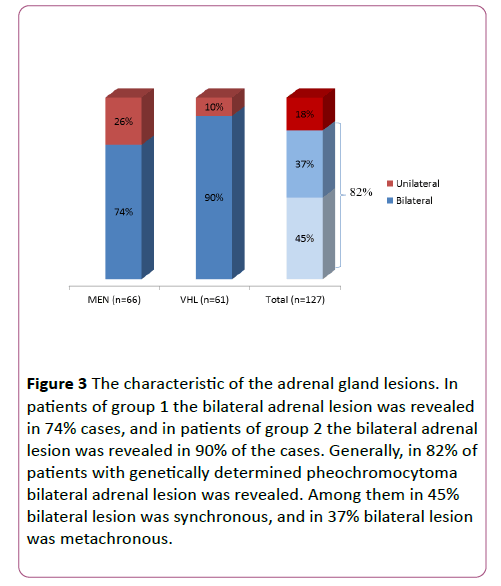
44% of patients (n=29) with MEN 2 had synchronous pheochromocytomas (bilateral adrenal lesion was initially diagnosed), and 30% of patients (n=20) had metachronous pheochromocytomas (after the surgical treatment of pheochromocytoma at one side, tumor in the other adrenal gland further developed). Generally, in group 1 bilateral adrenal lesion was revealed in 74% cases (n=49), and in 26% of patients (n=17) at the time of the study the unilateral adrenal lesion was diagnosed.
In patients with Von Hippel-Lindau Disease the bilateral adrenal lesion was revealed in 90% of the cases (n=55; 46% synchronous (n=28) and 44% metachronous (n=27)). 10% of patients (n=6) in this group had unilateral lesion.
Generally, in 82% of patients (n=104) with genetically determined pheochromocytoma bilateral adrenal lesion was revealed. Among them in 45% (n=57) bilateral lesion was synchronous, and in 37% (n=47) bilateral lesion was metachronous (Figure 3).
Figure 3: The characteristic of the adrenal gland lesions. In patients of group 1 the bilateral adrenal lesion was revealed in 74% cases, and in patients of group 2 the bilateral adrenal lesion was revealed in 90% of the cases. Generally, in 82% of patients with genetically determined pheochromocytoma bilateral adrenal lesion was revealed. Among them in 45% bilateral lesion was synchronous, and in 37% bilateral lesion was metachronous.
In our study in group 1 (n=66) none of the patients had extra-adrenal pheochromocytoma. In group 2 (n=61) extraadrenal location of pheochromocytoma (paraganglioma) was detected in 16.4% of patients (n=10): one patient had paraganglioma of the chest cavity and 9 patients had paragangliomas of the retroperitoneum.
According to WHO criteria, malignancy of tumor from chromaffin tissue is defined by the presence of metastases, but not by conventional morphological criteria [9]. No patient was found to have metastases of pheochromocytoma in groups 1 and 3 (n=66 and n=40). In group 2 (n=61) 4 patients (6.6%) had metastases of pheochromocytoma: to liver (n=2), skull bones (n=1) and the spine (n=1).
Histological examination of tumors in group 1 (n=66) revealed pheochromoblastoma in 20% of cases (n=13) and pheochromocytoma in 80% of cases. In group 2 (n=61) 31% of patients (n=19) had pheochromoblastoma and 69% of patients had pheochromocytoma. In group 3 (n=40) only one patient had pheochromoblastoma. The difference between group 3 and groups 1 and 2 was statistically significant (р=0.01 and р=0.0004 respectively).
It should be noted that in 3 patients with metastases of pheochromocytoma the primary tumor histologically has been interpreted as benign pheochromocytoma, and in 1 patient with verified metastatic process the primary tumor histologically has been interpreted as pheochromoblastoma. These data again highlight that there are no clear criteria of malignant pheochromocytoma.
Partial adrenalectomy for pheochromocytoma (resection of adrenal gland with tumor) has been done in group 1 to 5 patients (3 patients with mutation at codon 634, 1 patient with mutation at codon 918 and 1 patient without genetic study). All of patients had tumor recurrence at the operated side after 7 years (ÃÂϛ) (min/max 1-25 years; SD ± 9.69 years). One patient underwent 6 surgical interventions on the same adrenal gland. During the latter intervention peri - and postoperative complications occurred resulting in death of the patient. The main cause of complications is the pronounced scar process in the area of operations.
In group 2, 8 patients underwent partial adrenalectomy. All of them had tumor recurrence at the operated side. The median time of recurrence detection was 13 years (min/max 1-27 years; SD ± 9.34 years). 5 patients have been operated again without complications. 3 patients have had peri- and postoperative complications: abscess, lower lobe pneumonia, bleeding. Thus, 10% patients (n=13) with genetically determined pheochromocytoma (n=127) underwent partial adrenalectomy, then all of patients (100%) have had tumor recurrence at operated side after ~10 years (min/max 1-27 years; SD ± 9.16 years). 4 patients (more than 1/3 of all patients with recurrence) have had peri- and postoperative complications: pancreatic abscess, lower lobe pneumonia, bleeding. The main causes of complications are the pronounced scar and adhesions process in the area of operations.
To answer the question about the reason for such high number of recurrence we examined the nature of the lesions within the adrenal gland. In group 1 (n=66) multifocal lesion has been detected in 62% cases (n=41) and in group 2 (n=61) in 53% cases (n=32). Generally, multifocal lesion in genetically determined pheochromocytomas has been noted in 58% of cases. There were no statistically significant differences between 1 and 2 groups (р>0.05). In group 3 (n=40) there were no data for primary-multiple lesion.
Discussion
Genetically determined pheochromocytomas have laboratory and topical features. There is no doubt that the genetic testing is necessary for determination of the probability of occurrence of serious diseases, associated with hereditary pheochromocytomasyndromes, the time of their manifestation and the aggressiveness of their clinical course, the tactics of patients’ management and identification sick relatives.
Our data are comparable with data of other studies – pheochromocytoma occurs almost equally in both men and women, with a slight predominance of women [10].
Our study demonstrates the delayed diagnosis of medullary cancer and almost complete lack of "preventive thyroidectomy" practice in Russia in last decades. The identification of medullary cancer on manifest stadium means the high probability of metastasis [11]. In our opinion, the low frequency of hyperparathyroidism diagnosis may be due to surgical trauma of parathyroid glands during thyroidectomy performing for the medullary thyroid cancer.
Patients with Von Hippel-Lindau Disease significantly more often have erythrocytosis, retinal angiomatosis, central nervous system hemangioblastomas, polycystic and kidney cancer, tumors of pancreas and Brugada syndrome.
As mentioned above, not all patients in our study have been identified as having mutation, confirming the diagnosis of Von Hippel-Lindau Disease. This may be due to low sensitivity of method for determining VHL gene mutation status (falsenegative result), patient refusal or lack of possibility for testing (the molecular testing of Von Hippel-Lindau Disease has been introduced in Russia only since the mid-2000s). Thus, the diagnosis in patients without genetic examination was based on combination of 2 and more features, associated with this syndrome. In our study, the diagnosis «Von Hippel-Lindau Disease» was based on combination of pheochromocytoma and presence of retinal angiomatosis and/or central nervous system hemangioblastomas and/or kidney cancer and/or tumors of pancreas. The erythrocytosis, polycystic of pancreas and kidneys were not in themselves grounds for the Von Hippel-Lindau Disease diagnosis due to their frequent occurrence in a general population. On the contrary, there are few data about combination of rare Brugada syndrome, which characterized by frequent episodes of polytope ventricular tachycardia and syncope, and Von Hippel-Lindau Disease in the literature. In this connection, the combination of this syndrome with pheochromocytoma, in our opinion, is not enough for positive diagnosis without genetic confirming, and further study of this issue is necessary. Generally, the presence of the listed above comorbidities in patient should orient the medical research in relation to the pheochromocytoma and Von Hippel-Lindau Disease identification.
The diagnosis process of pheochromocytoma (both in patients with MEN 2 and patients with Von Hippel-Lindau Disease) in most cases was initiated because of patients’ complaints. Primary detection of medullary thyroid cancer also contributes to the early diagnosis of pheochromocytoma in MEN 2 patients. Generally, pheochromocytoma was detected during routine examination based on a known family history only in 7% (n=9) of patients with genetically determined syndromes, while targeted survey about relative’s diseases allows to suspect pheochromocytoma in 37% (n=47) of patients. The presented data confirm the importance of informing the first-degree relatives of patients with genetically determined syndromes about necessity of examination.
It is known, that the average age of pheochromocytoma manifestation in population of patients without genetic examination is 40-50 years [12]. According to our data, genetically determined pheochromocytomas are more common in young people, while sporadic pheochromocytomas are more common in people aged over 39 years. For this reason, we consider that it is necessary to exclude genetic causes of pheochromocytoma in patients younger than 40 years of age.
Pheochromocytoma is detected significantly earlier in patients with MEN 2 than in patients with sporadic pheochromocytoma (р>0.0000001). Pheochromocytoma is detected significantly earlier in patients with Von Hippel- Lindau Disease (49% - in the childhood), than in patients with MEN 2 (р=0.000004) and patients with sporadic pheochromocytoma (р>0.0000001). The high frequency of genetic cause of disease in children (according to the literature it reaches 40% [13]) highlights the potential importance of genetic studies in pediatric patients with this type of tumors. Thus, in our opinion, RET-mutation carriers and patients with Von Hippel-Lindau Disease should be screened for pheochromocytoma annually. Screening should begin no later than 18 years of age in RET-mutation carriers and no later than 7 years of age in patients with Von Hippel-Lindau Disease.
It is known that the symptoms of pheochromocytoma are diverse. The most common clinical symptoms of disease (classic triad) include headache attacks, excessive sweating and palpitation (40% - 80% of patients). Hypertension is detected in more than 90% of patients (new onset or worsening of pre-existing hypertension; hypertension is often paroxysmal in nature). All of these symptoms are not always present, may be produced by many other clinical conditions and are not diagnostically significant [14].
The differences between clinical symptoms are due to features of diseases’ pathogenesis. It is known that tumors in MEN 2 produce phenylethanolamine-N-methyltransferase (enzyme that converts norepinephrine into epinephrine), while in tumors in Von Hippel-Lindau Disease hypoxia activates angiogenesis. Tumors in MEN 2 secrete predominantly epinephrine in the background, while in paroxysmal mode they secrete epinephrine and norepinephrine. Pheochromocytoma in patients with Von Hippel-Lindau Disease in the absence of the above-mentioned enzyme has more constant norepinephrine catecholamine profile [15]. Tumors in MEN 2 have smaller size of catecholamine stores and more intensive intratumoral metabolism (intratumoral inactivation due to methylation) compared with tumors in Von Hippel-Lindau Disease. These features explain the low clinical activity of small size tumors. The differences in secretion of norepinephrine and epinephrine in these two types of tumors and the direct effect of catecholamines on alpha and betaadrenergic receptors determine the differences in the clinical picture of syndromes [15,16].
The hypertension in Von Hippel-Lindau Disease occurs more frequently due to constant cathecholamine (norepinephrine) profile. In MEN 2 high blood pressure is not always fixed, and even hypotension may be diagnosed, due to paroxysmal cathecholamine secretion. Headache accompanies hypertension, which, respectively, occurs more often in group 2. Norepinephrine type of secretion, possibly, also plays role in more frequent occurrence of this symptom due to reduction of cerebral blood flow. Also, hyperactivation of the sympathetic nervous system and exactly norepinephrine release is the cause of panic attacks in patients with norepinephrine type of tumor secretion (patients with Von Hippel-Lindau Disease).
Pheochromocytoma as part of MEN 2 is characterized by epinephrine type of secretion, pheochromocytoma as part of Von Hippel-Lindau Disease is characterized by norepinephrine type of secretion, and sporadic pheochromocytoma is characterized by mixed type of secretion. When comparing the presented groups the following tendency can be observed: patients with MEN 2 are characterized by low-amplitude increased normetanephrine level and medium-amplitude increased metanephrine level. Patients with Von Hippel-Lindau Disease are characterized by high-amplitude increased normetanephrine level and low-amplitude increased metanephrine level. Patients with sporadic pheochromocytoma are characterized by high-amplitude increased metanephrine and normetanephrine levels regarding the upper limit of normal.
Secretory feature of the tumor may determine the diagnostic concept and tactics of further examination of the patients. Isolated secretion of norepinephrine may suppose the Von Hippel-Lindau Disease. In patients with predominant epinephrine secretion there is a high probability of the MEN 2. In these patients it is necessary to determine RÕâ gene mutation status and examine for a MTC.
The maximum tumor size was observed in patients with sporadic pheochromocytoma. Probably, the earlier diagnosis of pheochromocytoma (at the stage of small tumor size) in patients with genetically determined pheochromocytoma is due to curation of patients with a known family history and with MTC. The curation contributes to the survey for pheochromocytoma. Generally, our data are consistent with other author’s data: the average tumor size in general population of patients with pheochromocytoma is 3-5 cm [17].
In patients with MEN 2, the smaller the tumor, the smaller the level of methylated catecholamine. Therefore, in patients with MEN 2 the adrenal tumor with any increase of catecholamine levels (including the gray-zone elevation) should be regarded as pheochromocytoma, without conducting confirming tests.
Genetically determined forms of pheochromocytoma may be associated with bilateral tumors. Thus, after the unilateral adrenal surgical removal, it is important to follow-up, in order to detect pheochromocytoma of the other adrenal gland. Patients are followed with once a year urine catecholamines.
Pheochromocytoma in patients with MEN 2 is exclusively located in the adrenal gland. In this regard, in patients with MEN 2 (but not in the patients with noradrenaline type of secretion) it is permitted to conduct imaging tests to locate a possible tumor only within the abdomen. Searching for extraadrenal pheochromocytoma using scintigraphy or other imaging tests in patients with MEN 2 is inappropriate.
The risk of malignancy in patients with genetic syndromes is low and malignant pheochromocytoma is not associated with MEN 2. In our opinion, searching the metastases of pheochromocytoma in patients with MEN 2 is inappropriate. There are no clear criteria of malignant pheochromocytoma. In this regard, further research in this direction is necessary.
The hereditary forms of pheochromocytoma are characterized by multicentric lesion, suggesting that the progression of primary-multiple process from the residue of adrenal medulla is the cause of 100% local recurrence of pheochromocytoma after partial adrenalectomy. In this regard, it is appropriate to recommend the radical operative treatment (adrenalectomy with tumor) to all patients with genetically determined pheochromocytoma.
Generally, we studied the clinical, laboratory and topical features of chromaffin tumor. Our data allows optimizing approaches to diagnosis and treatment of the most severe genetically determined forms of pheochromocytoma. These facts are reflected in the relevant conclusions.
Conclusion
Genetically determined pheochromocytomas have laboratory and topical features, requiring a differentiated approach to diagnosis and treatment.
The age of onset for genetically determined pheochromocytoma is usually before 40 years.
The pheochromocytoma as part of MEN 2 is characterized by epinephrine type of secretion, and the pheochromocytoma as part of Von Hippel-Lindau Disease is characterized by norepinephrine type of secretion.
In patients with MEN 2 we founded the positive correlation between tumor size and level of methylated catecholamine derivatives excretion. False-negative results of laboratory diagnosis of pheochromocytoma in MEN 2 may be due to a low activity of small tumors.
In patients with MEN 2 and Von Hippel-Lindau Disease the bilateral adrenal lesion has been detected in 82% of cases (synchronous or metachronous), and MEN 2 is not associated with malignant or extra-adrenal lesion.
The 100% local tumor recurrence after partial adrenalectomy in patients with MEN 2 and Von Hippel-Lindau Disease is due to multicentric nature of the tumor within the adrenal gland.
Acknowledgements
We wish to acknowledge the academician of Russian Academy of Sciences, President of the Russian Association of endocrinologists, Director of the Endocrinology Research Centre Dedov I.I., as well as the academician of Russian Academy of Sciences, Director of the Institute of clinical endocrinology of the Endocrinology Research Centre Melnichenko G.A.
Funding
The article was supported by the FTP «Research and scientific-pedagogical personnel of innovative Russia» for 2009 - 2013 years (activity 1.2.1 – I queue), theme of scientific research: «Optimization the methods for diagnosis and treatment of neuroendocrine tumors».
Competing Interests
The authors declare no potential conflicts of interest with respect to research, authorship and/or publication of this article.
References
- Martins R, Bugalho MJ (2014) Paragangliomas/Pheochromocytomas: Clinically oriented genetic testing. Int J Endocrinol1: 794187.
- Lefebvre M, Foulkes WD (2014)Pheochromocytoma and paraganglioma syndromes: genetics and management update. CurrOncol21:e8-17.
- Benn DE, Gimenez-Roqueplo AP, Reilly JR, Bertherat J, Burgess J, et al. (2006) Clinical presentation and penetrance of pheochromocytoma/paraganglioma syndromes. J ClinEndocrinolMetab91:790– 836.
- DeLellis RA, Lloyd RV, Heitz PU, Eng C (2004) WHO classification of tumors. pathology and genetics of tumours of endocrine organs. IARC Press,Lyon.pp: 147-150
- Eisenhofer G, Walther MM, Huynh TT, Li ST, Bornstein SR, et al. (2001) Pheochromocytomas in von Hippel-Lindau syndrome and multiple endocrine neoplasia type 2 display distinct biochemical and clinical phenotypes. J ClinEndocrinolMetab86:1999 -2008.
- Graff JW (2009) VHL // Family Forum, Newsletter of the VHL Family Alliance and the Cancer Research Fund.
- Klingler HC, Klingler PJ, Martin JK, Smallridge RC, Smith SL, et al.(2001)Pheochromocytoma. Urology 57:1025-1032.
- Kloos RT, Eng C, Evans DB, Francis GL, Gagel RF, et al. (2009) Medullary thyroid cancer: management guidelines of the American Thyroid Association. Thyroid 19:565-612.
- Karagiannis A, Mikhailidis DP, Athyros VG, Harsoulis F (2007)Pheochromocytoma: An update on genetics and management. EndocrRelat Cancer 14:935-956.
- Frank-Raue K, Machens A, Scheuba C, Niederle B, Dralle H,et al. (2008) Difference in the development of medullary thyroid carcinoma among carriers of RET mutations in codon 790 and 791. Clinical endocrinology 69:259-263.
- Jiménez C, Cote G, Arnold A, Gagel RF (2006)Should patients with apparently sporadic pheochromocytomas or paragangliomas be screened for hereditary syndromes? J ClinEndocrinolMetab91:2851–2858.
- Manger WM (2005)The vagaries of pheochromocytomas. Am J Hypertens18:1266-1270.
- Kantorovich V, Pacak K (2010)Pheochromocytoma and paraganglioma. Prog Brain Res 182:343-373.
- Pacak K, Lenders JWM,Eisenhofer G (2007) Pheochromocytoma: Diagnosis, localization and treatment. Catecholamines and adrenergic receptors.Blackwell,Malden, MA.pp: 41-71.
- Pacak K, Lenders JWM,Eisenhofer G (2007)Pheochromocytoma: Diagnosis, localization and treatment: Introduction. Blackwell,Malden, MA.pp: 1-2.
- Pacak K, Linehan WM, Eisenhofer G, Walther MM, Goldstein DS (2001) Recent advances in genetics, diagnosis, localization, and treatment of pheochromocytoma. Ann Intern Med134:315-329.
- Szinnai G, Meier C, Komminoth P, Zumsteg UW (2003) Review of multiple endocrine neoplasia type 2A in children: Ther apeutic results of early thyroidectomy and prognostic value of codon analysis. Pediatrics111:132-139.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences