ISSN : 2574-2825
Journal of Nursing and Health Studies
Challenges and Priorities of Nursing Profession and Services in Uganda: A Mixed Methods Study for Strategic Planning
Sam A Okuonzi1, Joseph Mwizerwa2, Michael Lyavala3, Joan Kabayambi3, Tony Mpanga3, Irene Atuhairwe4 and Agnes Bakucandia5
1Hospital Management Board, Arua Regional Referral Hospital, Arua, Uganda
2Department of Nursing, Aga Khan University, Kampala, Uganda
3Nursing Consultancy Group, Kampala, Uganda
4Seed Global Health, Kampala, Uganda
5Department of Nursing, Ministry of Health, Kampala, Uganda
- *Corresponding Author:
- Sam A Okuonzi
Hospital Management Board,
Arua Regional Referral Hospital, Arua,
Uganda,
E-mail: sokuonzi@gmail.com
Received date: November 02, 2023, Manuscript No. IPJNHS-23-18090; Editor assigned date: November 06, 2023, PreQC No. IPJNHS-23-18090 (PQ); Reviewed date: November 20, 2023, QC No. IPJNHS-23-18090; Revised date: November 27, 2023, Manuscript No. IPJNHS-23-18090 (R); Published date: December 04, 2023, DOI: 10.36648/2574-2825.8.6.101
Citation: Okuonzi SA, Mwizerwa J, Lyavala M, Kabayambi J, Mpanga T, et al. (2023) Challenges and Priorities of Nursing Profession and Services in Uganda: A Mixed Methods Study for Strategic Planning. J Nurs Health Stud Vol.8 No.6:101.
Abstract
Introduction: Nurses and midwives make up the majority of health workforce. Nursing services are needed in all settings throughout an individual’s life. Uganda has had no strategic direction for developing nursing and midwifery services. This study was done between August 1, 2021 and March 31, 2022 to understand the context and experiences of nurses and midwives for strategic planning of nursing in the country. Specifically, the objectives were to identify the challenges, strengths and opportunities and priorities for strategic planning.
Methodology: Three methods were used: A survey of views from nurses and midwives key informant interviews, and focus group discussions.
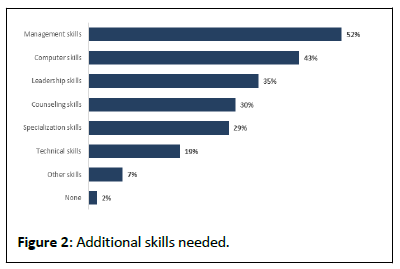
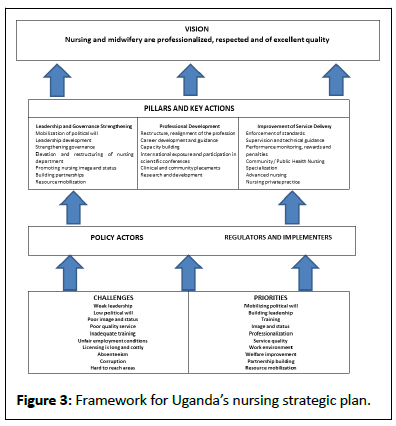
Findings and discussion: Considerable progress has been made to establish nursing and midwifery institutions, training and services, but major challenges remain. Fortyseven percent of nurses were found to be certificate holders, 45% had diploma, 7% had a bachelor’s degree and 1% had a master’s degree. Most nurses did not practice at their level of training. Seventy-three percent of nurses are motivated by love for work and people, but over 80% are discouraged by the low salary. In addition to nursing skills, nurses need skills in management, leadership, computer science, counseling and various specialized fields. The challenges in nursing include weak leadership and governance, low political will, poor nursing image and status, poor quality nursing services, inadequate training, unfair employment conditions, long and costly licensing, absenteeism, extortion of money from patients and lack of nurses in hard-to-reach areas. The priorities are grouped under leadership and governance, training and professionalization, and service delivery.
Conclusion: There is need to mobilize political will, develop nursing leadership, elevate the nursing profession and promote nursing status and image in society. The nursing profession has to be aligned with the equivalent health cadres. International and regional bench-marking is required for comparability. Research led and done by nurses about nursing has to become a key element in the profession. Qualification and service standards have to be reviewed, matched and enforced. The quality of services and the performance of nurses should be monitored and supervised regularly. Public health nursing ought to be revitalized for primary health care to support universal health coverage. Special arrangements and incentives need to be made to attract nurses to remote and hard-to-reach areas. In addition, specialization, advanced nursing, and private nursing ought to be promoted and bench-marked internationally and matched with other health sector professions.
Keywords
Nursing; Midwifery; Challenges; Priorities; Service delivery; Professionalization; Strategic planning
Abbreviations
ADHO: Assistant District Health Officer; AGNMU: Association of Graduate Nurses and Midwives’ Unions; APN: Advanced Practice Nurses; CHN: Community Health Nurse; COVID-19: Corona Virus Disease of 2019; ICT: Information and Communication Technology; MOES: Ministry of Education and Sports; MOH: Ministry of Health; MPS: Ministry of Public Service; NGO: Non-Government Organization; ODK: Open Data Kit; PhD: Philosophia Doctorate (Doctor of Philosophy); PHN: Public Health Nurse; SPSS: Statistical Package for the Social Sciences; UHC: Uganda Health Coverage; UNMC: Uganda Nurses and Midwives’ Council; UNMEB: Uganda Nurses and Midwives Examination Board; WHO: World Health Organization.
Introduction
Background
Nurses and midwives constitute 50%-90% of human resources for health in most countries [1]. They spend about 95% of their time with patients. Nursing services are needed in all settings throughout an individual’s life. Nursing and midwifery services are regarded as critical for the attainment of Universal Health Coverage (UHC) and health-related Sustainable Development Goals (SDGs). At the same time, nurses are in high demand in developed countries, where there is a net migration from poor countries in Africa to richer countries [2]. Global and national health systems are dynamic with new challenges and solutions constantly emerging [3]. Nursing and midwifery face serious and unique challenges globally, but especially in Africa.
Uganda has had no policy or strategic direction to develop nursing and midwifery [4]. There are numerous challenges being experienced by nurses and midwives which have not been systematically studied or recorded. Uganda’s ministry of health (MOH desired a strategic plan for the improvement of nursing and midwifery. The study was done between August 1, 2021 and March 31, 2022. The purpose of this study was to understand and document the current context and experiences of nurses and midwives as a basis for strategic planning. The objectives of the study were to: (1) Identify challenges faced by nurses and midwives; (2) Explore existing strengths and opportunities for improving nursing and midwifery; (3) Identify priorities for strategic planning.
Origin and evolution of nursing
The word “nurse” is from the Latin word “nutrire”, meaning to suckle, referring to wet-nurse. In 16th century nursing attained its modern meaning of a person who cares for the infirm [5,6]. From around 2000 BC the word “nurse” was associated with the care of the sick, the helpless, the very young, the injured and the disabled. The profession started as a desire to keep people healthy and comfortable, by providing care and assistance. Florence nightingale (1843-1950) is widely recognized as the person who greatly contributed to modern nursing and midwifery through the promotion of training and patient care [6].
Modern nursing services started in Uganda under British colonial medical services with a midwifery training center established in 1919 [4,6,7]. The first native midwives graduated in 1935. In 1958, Uganda Nurses and Midwives Council was formed to regulate training, regulation and establishment of standards of practice. In 1961, registered nursing and midwifery training started at Mulago School of Nursing and Midwifery. In 1967, registered nursing and midwifery was established at Mengo Mission Hospital. In 1960 mental health nursing had started in Butabika Mental Hospital.
From 1970s to 1990s several courses were introduced for nursing and midwifery tutors, including administration, public health nursing, anesthesia and ophthalmic nursing [8]. A multipurpose nurse cadre was created to deliver what were defined as essential health packages for different health care levels. This led to the creation of the formalized comprehensive nurse cadre for basic promotive, preventive, curative, rehabilitative services at lower-level units. In 1993, a bachelor’s degree course in nursing was introduced.
Uganda’s nursing scheme of services
Nursing and midwifery functions in Uganda include: “advocacy, disease prevention, health promotion, health education, counseling, treatment and care, coordination and collaboration, research and leadership and management” [9,10]. Because of the many changes in the health sector, the content of training of nurses has been revised and nursing cadres redesignated with new titles. Professional growth for nurses and midwives is through upgrading through further training, continuous professional development and continuous ethical and moral training to foster acceptable attitude towards clients and colleagues. Currently, the recognized nursing and midwifery qualifications in Uganda are: Certificate (enrolled), diploma (registered), higher diploma (specialist), bachelors in nursing or midwifery, post-graduate diploma (specialist) and masters in nursing or midwifery [10].
The model nurse
WHO is promoting a new nurse cadre based on a four-year competency-based prototype curriculum, particularly for the Africa region [11-13]. The idea is to create a one-nurse cadre who is competent in nursing and midwifery. It also attempts to solve the variation in course content across countries, the lack of balance between theory and practice and the lack of a standard guide for clinical training. Also, the approach is attempting to overcome the lack of teaching materials, linking training to specific competencies, the lack of well-qualified nursing teachers and to improve nurses’ performance in an environment of weak regulation. The curriculum covers disease prevention, health promotion, illness treatment and rehabilitation. The vision of the model nurse project is to produce a nurse to improve the health outcomes of individuals, families, groups, communities through quality, culturally sensitive and evidence-based nursing and midwifery.
The course has 35 modules over a period of four years. The subjects include: ICT, sociology, anatomy and physiology, microbiology and parasitology, fundamentals of nursing, community health, pharmacology, medical and surgical nursing, mental health nursing and health service management. It is based on the concepts of nursing process; health care system; PHC; ethical values, professionalism and advocacy and evidencebased practice. Other competencies include: Inter-personal relations, communication skills, professionalism, ethical and legal practice, teamwork and collaboration, accountability, evidence based practice, quality improvement, safety, patient-centered care, health promotion, system-based approach, integrating science into practice, integrating clinical knowledge and skills in patient care and leadership.
Justification for a certificate nurse or midwife
The model nurse and midwife project and other efforts have attempted to replace the certificate nurse with a higher caliber nurse. The draft of Uganda Nursing and Midwifery Policy 2018 specifically recommended that the certificate nurse be phased out [4]. But the ministries of health and education have argued that the certificate nurse is the most available and capable front line cadre in contact with patients and communities. Their role and competence should only be further augmented.
The new curriculum for a certificate in nursing uses Competence-Based Education and Training (CBET) principles [14]. These principles include: Learning through training; teaching based on acquiring skills in a practical and systematic manner; learning step-by-step; prior learning as well as learning on the job. CBET reduces the cost of training, improves access and relevance. The key challenge in health sector is the rapidly changing nature of skills demanded of a variety of cadres. The certificate nurse has a clear pathway for professional growth: They can do a diploma, or go straight for a bachelor’s degree and proceed to masters and PhD.
Diploma nursing and midwifery direct from school
In Uganda, the well-known advanced nurse is the diploma nurse. Students enter training direct from school (after Advanced-level certificate of education) and have a larger and deeper coverage of subjects than the certificate nurse [15]. The subjects include: Anatomy and physiology, body systems, fundamentals of nursing, sociology, psychology, basic computer science, guidance and counseling. Other subjects include microbiology, personal communication, medical nursing, pharmacology, surgical nursing, pediatric nursing, PHC, palliative care, disaster management, tropical medicine and common diseases. The other subjects are: Gynecology, reproductive health, mental health and mental health nursing, applied research, teaching methodology and health services management. They are prepared as care-givers, leaders, managers, teachers and researchers. They have open way for advancement to bachelors, masters and doctorate.
Advanced practice nursing: A curriculum framework has been proposed for Advanced Practice Nursing (APN) in sub-Saharan Africa [16]. APN is well legislated already in use in developed countries to cater for underserved and rural populations. Initiatives for advanced practice nursing have started in developing countries such as Kenya [17]. The nurses undergo higher and comprehensive training and learning. The knowledge domains skills and competences they acquire are in Table 1.
| S.No. | Knowledge Domains | Skills |
|---|---|---|
| 1 | Nursing leadership | Health care governance |
| Leadership | ||
| Management | ||
| Advocacy | ||
| Resource management | ||
| 2 | Quality practice | Quality care delivery |
| Continuous Professional Development | ||
| 3 | Ethico-legal practice | Ethos |
| Legal aspects | ||
| Clinical teaching | ||
| 4 | Education and research | Community education |
| Research and publication | ||
| History taking | ||
| Physical education | ||
| Lab test interpretation | ||
| Diagnosis in area of specialization | ||
| 5 | Advanced Nursing Practice | Prescription of treatment |
| Admit patients | ||
| Discharge, refer | ||
| Comprehensive management of patients | ||
| 6 | Attitudes and values | Patient and family centered care and cultural sensitivity |
Table 1: Knowledge domains and skills of APN.
The training of APN requires teachers at doctorate level with a strong practical experience. It requires experiential learning, problem-solving, adult-oriented, critical thinking and ability to apply concepts to practical situations. The APN comprehends the health system. They can plan, execute and evaluate health care services. The APN can teach evidence-based, culturally sensitive, quality and cost-effective health care. They can propose, conduct and synthesize research findings for evidencebased cost-effective health care. The curriculum is context specific and responds to the health care needs of the community, especially children and mothers. Training for the same has commenced in Kenya at Aga Khan University [17].
Public health nurse and primary health care
Public or Community Health Nursing plays a big role in primary health cares and is critical for the attainment of universal health coverage. Public Health Nurses (PHN) have the potential can meet health care needs of various population groups in a variety of community settings. World Health Organization (WHO) conducted a study between 2010 and 2014 which examined the status of PHN/CHNs in 22 countries [18]. Thirteen of the countries were experiencing a critical shortage of health workers. Challenges identified were: Limited availability of career opportunities; poor worker retention; low recognition for PHN/CHNs; inadequate and unfavorable working conditions and environment; absence of educational standards; varying educational entry-level requirements for CHN programs and a lack of consensus on the scope of practice for CHNs.
Public health nursing is defined as the practice of promoting and protecting the health of populations using knowledge from nursing, social and public health sciences. It focuses on population health, with the goal of promoting health, preventing disease and disability and rehabilitation. Globally PHN/CHN is classified as a specialty area in nursing because of its focus and scope. In Uganda, the training of public health nurses (or health visitors) started in 1965 at certificate level, which was then referred to as “assistant health visitors”. However, this cadre was phased out when their only training institution was closed down to pave way for the establishment of Mbarara University of Science and Technology (MUST). The PHN cadre is established in Uganda’s public service. But there is currently little effort to promote the cadre.
Public Health Nursing offices at the Ministry of Health are vacant, nonfunctional or occupied by clinical nurses. The current scheme of service for the nursing and midwifery cadre is geared to only clinical nursing and midwifery but not for PHN/CHN. And yet there are established senior positions Public Health Nursing Officers requiring a master’s in public health nursing. Currently, there is not even a bachelor’s level course for PHN. Among the functions of the PHN/CHN should be to train, supervise and coordinate Community Health Workers, including VHTs. PHN/CHN is the professional link between the Community and the health facility.
Private nurse practice
Private practice for nurses is varied and mostly at experimental stages. A study of psychiatric nursing practitioners identified three common themes in the needs of the nurses: Personal competences, professional competences and communication skills [19]. The study concluded that a private nurse practice needs additional competencies in service delivery and benefits immensely from supportive supervision. Professional competences required include supervision expertise, specialized expertise and involvement in research [20]. Personal competences include: Assertiveness and authoritativeness, emotional intelligence, flexibility, holistic and broad world view. Communication skills needed by a private nurse practitioner include systematic questioning, effective feedback and listening skills.
Other studies have identified three models of private nursing practice [21-23]. These models are:
• Collaborative model between a nurse practitioner and a physician
• Community-based, nurse-led health clinics or health centers, mainly for children and mothers
• Reimbursement based on national health financing systems, applied mainly in Medicare in USA and Tele-health programs of Australia.
The acceptance of private nurse practice is mixed among physicians. The study concludes that nurses must be more involved in national and international health policy-making, there is need to educate physicians and engaging with doctors more effectively.
Experiences shared by private nurse practitioners are wideranging. Some authors identify the development of personal environment, understanding stress emotions and self-care strategies as important [24,25]. It requires self-improvement through education and research. Another private nurse practice experience concludes that private nursing practice is a “leap of faith” [26]. Private nursing practice can be daunting initially, but rewarding eventually [27]. The experiences with private midwives indicate that they enjoy a good level of autonomy but are still restricted by law in employing other midwives and to prescribing only a limited range of medicines. There are other structural barriers that need to be addressed to open private practice reasonably wider.
Policy and work environment
Nurses and midwives work in a national health system, which is itself an integral part of the national economy. National health services are guided by national health policies and strategic plans. It is noted that human resource for health is expensive, inefficient and unresponsive. The health staffing level was at 57%, with a high rate of attrition. There were not enough incentives to attract staff to hard-to-reach areas. A human resource crisis in Uganda’s health sector has been characterized as leadership deficit, poor motivation, low performance, lack of integrity and poor ethical conduct. Other problems have been identified as poor stewardship, a competitive environment for health workers and corruption.
A recent evaluation of the sector shows progress was made in only 7 (18%) of the 42 performance indicators. There was no progress in 57% of the indicators and 26% of the indicators were not assessed. Uganda’s health work force density is 1.6 per 1000 population, which is far short of WHO recommended minimum density of 4.45 per 1000. Although the latest national health staffing level stands at 74% on paper, in reality, due to authorized absenteeism it is at 38% [28]. The vision of the government for health sector human resource is “equitable access to quality health services provided by competent, motivated and supported staff” [29]. The mission of the plan is to “build resilient and responsive human resource for health”.
However, these policies do not address the unique issues and challenges of nursing and midwifery profession and services. WHO developed the Global Strategic Directions for Strengthening Nursing and Midwifery, which urges countries to adopt evidencebased national plans that can facilitate nurses and midwives to provide high impact services and with low-cost interventions [1]. The strategy urges countries to embrace people-centered nursing care under four themes:
• Education, competence and motivation
• Policy, leadership and governance
• Capacity-building through partnerships and
• Mobilizing political will
Table 2 presents a summary of the WHO’s proposed strategic directions for strengthening nursing and midwifery.
| Themes | Strategies | Actions |
|---|---|---|
| Theme I Educated, competent and motivated |
Plan for and invest in education and regulation and conducive work environment | Plan and cost |
| Prepare guidelines on licensure, education and service delivery | ||
| Theme II Policy, leadership, management and governance |
Involve nursing and midwifery leaders in policy development, health system management and in research | Raise the level of involvement of nurses and midwives |
| Engage nurses in policy decision-making | ||
| Support and invest in regulation | ||
| Set practice standards | ||
| Set a system to collect data on nurses and midwives | ||
| Theme III Partnership and continuous professional development |
Align national health policy and workforce plans through TWG on education and practice | |
| Delineate, monitor and evaluate roles, functions and responsibilities of nursing workforce | Involve nurses in policy development | |
| Theme IV Mobilizing political will |
Mobilize political support for nurses at the highest political level and within civil society | Align nursing with UHC and SGDs |
| Build multi-sectoral groups to support nurses and midwives | ||
| Increase access to NGOs and private sector | ||
| Update training curricula | ||
| Make advocacy plan to target policy-makers and key organizations |
Table 2: Strategic directions for nursing and midwifery.
Uganda’s nursing and midwifery policy
The first ever attempt to have a policy specifically on nursing and midwifery in Uganda has not been adopted by the government [4]. The document points out the problems of unclear scope of work, weak institutions, inequitable nurses’ representation in the health sector leadership and weak leadership within the profession. It notes that most skilled health workers are urban based and the less skilled are in rural areas. It also notes that staffing numbers are based on the facility level rather than on workload. There are no national nurse-patient ratios, no work scope and no standards of service. And that the work environment of nurses and midwives is unsuitable and unsafe. Above all, that the remuneration of nurses is extremely low.
Other problems listed include: Graduate and post-graduate training are not recognized in the recruitment of nurses and midwives. Graduates of comprehensive nursing program are not recognized in public service. Nurses perform far above their job description but remain under-paid. There are no guidelines in writing patients’ case notes and files. Nurses and midwives tend to be promoted more in administrative work rather than in the professional ladder. There is no professional development plan for nurses and midwives. Nurses and midwives face stiff difficulties with getting scholarships for post-graduate training.
The policy document notes the proliferation of training institutions of doubtful quality and relevance. These institutions are often over-crowded and their capacity is often not assessed. There are wide variations in entry requirements and course content in these institutions. There are no mechanisms to assess the competences of the graduates of these training institutions. Internationally, specialization of nursing and midwives is after a bachelor’s degree, but in Uganda, it is unclear. Development partners have taken lead in designing training course contents without consulting the consumers of the services. In most cases, students and tutors are at the same level of training. This contravenes the general principle of education which requires that a teacher is professionally a step above the student. Research is the cornerstone for evidence-based practice, but no attention is paid to it in policy and practice. There is lack of capacity among nurses and midwives to do research. Research is not planned for or funded.
The document notes that nurses and midwives suffer from low social esteem and poor image and status. Nurses and midwives are front line workers and the face the public’s wrath and outrage of a broken health system. The poor professional image has been perpetuated by the historical female dominance of the profession. Society and the media have continued to cast the profession with belittling image. The terms of employment of nurses and midwives are unattractive with low pay. It also notes that there are increasing cases of unprofessional conduct among nurses and midwives. Nurses’ uniforms are not standardized; there is often no distinction between unskilled attendants and qualified nursing staff.
The document notes that whereas the nurses and midwives act of 1996 enabled the creation of Nurses and Midwives Council to “provide for regulation, training, registration, enrollment and discipline of nurses and midwives of all categories and other matters connected to the profession”, it is unclear how the council gets involved in the education and training of nurses and midwives. There is lack of scope and standards of practice. The Act has been overtaken by population growth, advancement in technology and gaps in nursing services.
Materials and Methods
Three methods were used in the study:
Key informant interviews
Key informants were commissioners at the MOH, training institution tutors, district health managers, directors and heads of department of ministries of health and education. Consent was sought from all respondents and those who declined were not interviewed. A nation-wide representation of the four regions (Central, East, North and West) was ensured. Altogether 43 key informants were interviewed.
Survey of views from nurses and midwives
A structured questionnaire that was administered to sampled nurses and midwives across the districts under study. Altogether 230 respondents were reached with 228 consenting to be interviewed. A district with a regional hospital was chosen in each of four regions of Uganda. Different health facilities and respondents were jointly identified by a District Health Officer (DHO) and director of the regional referral hospital, who had been alerted by MOH through a letter. The central region had additional national institutions where respondents were also drawn. These institutions included: MOH, national referral hospitals, Health Service Commission, Uganda Nurses and Midwives’ Council, Uganda Nurses and Midwives Union and Uganda National Health Care Consumers Organization.
The questionnaire was digitally designed and uploaded online using Kobo Collect tool, which is an ODK based mobile application. Prior to the field survey, a pilot was conducted in two health facilities, one public and one private health facility. Evans Morris’ hyper-geometric formula for small populations was used to derive sample size to eliminate selection bias. Data management (cleaning and transformation) was done using excel spreadsheet and analysis using SPSS version 22.
Focus group discussions
Two FGDs were held, one being through zoom conferencing to conform to COVID-19 regulations. One FDG was for eight Assistant District Health Officers (ADHO is a nurse or a midwife assigned to be in charge of maternal and child-health services in a district) and Uganda General Nurses and Midwives Union (UGNMU). Another one for Uganda Nursing and Midwifery Examination Board (UNMEB) members which was physical at their offices under COVID-19 regulations. FDGs also served as validation of the correctness of submissions in the study report.
Results and Discussion
Number and distribution of respondents surveyed
A total of 280 nurses and midwives were targeted, 230 consented and 228 (82%) were interviewed. Two respondents declined the interview, citing tight work schedule and lengthy interviews. 47% were certificate holders, 45% had diploma, 7% had a bachelor’s degree and 1% had a master’s degree. Fiftythree percent were from public facilities, 30% from not-forprofit health facilities and 17% from the private sector. Twenty percent (46) of the respondents were male and 80% (182) were female. See details in Table 3.
| Central | Eastern | Northern | Western | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| Type of facility (n=230) | ||||||||||
| NRH | 3 | 1% | 0 | 0% | 0 | 0% | 0 | 0% | 3 | 1% |
| RRH | 16 | 7% | 19 | 8% | 13 | 6% | 12 | 5% | 60 | 26% |
| Gen Hosp | 23 | 10% | 26 | 11% | 20 | 9% | 10 | 4% | 79 | 34% |
| HC IV | 4 | 2% | 11 | 5% | 6 | 3% | 5 | 2% | 26 | 11% |
| HCIII | 5 | 2% | 6 | 3% | 0 | 0% | 3 | 1% | 14 | 6% |
| Nurse Training School | 0 | 0% | 12 | 5% | 0 | 0% | 4 | 2% | 16 | 7% |
| Private Clinic | 0 | 0% | 11 | 5% | 9 | 4% | 2 | 1% | 22 | 10% |
| University | 10 | 4% | 0 | 0% | 0 | 0% | 0 | 0% | 10 | 4% |
| Total | 61 | 27% | 85 | 37% | 48 | 21% | 36 | 16% | 230 | 100% |
| Ownership (n=230) | ||||||||||
| Government | 28 | 12% | 54 | 23% | 19 | 8% | 21 | 9% | 122 | 53% |
| PFP | 10 | 4% | 12 | 5% | 15 | 7% | 3 | 1% | 40 | 17% |
| PNFP | 23 | 10% | 19 | 8% | 14 | 6% | 12 | 5% | 68 | 30% |
| Total | 61 | 27% | 85 | 37% | 48 | 21% | 36 | 16% | 230 | 100% |
| Gender (n=228) | ||||||||||
| Female | 51 | 22% | 69 | 30% | 31 | 14% | 31 | 14% | 182 | 80% |
| Male | 10 | 4% | 16 | 7% | 15 | 7% | 5 | 2% | 46 | 20% |
| Total | 61 | 27% | 85 | 37% | 46 | 20% | 36 | 16% | 228 | 100% |
| Age (n=228) | ||||||||||
| Average | 37 | 34 | 33 | 34 | 35 | |||||
| Max age | 59 | 64 | 54 | 54 | 64 | |||||
| Min age | 23 | 20 | 21 | 23 | 20 | |||||
| Level of training (n=228) | ||||||||||
| Certificate | 13 | 6% | 47 | 21% | 30 | 13% | 17 | 7% | 107 | 47% |
| Diploma | 41 | 18% | 29 | 13% | 15 | 7% | 18 | 8% | 103 | 45% |
| Degree | 7 | 3% | 8 | 4% | 1 | 0% | 1 | 0% | 17 | 7% |
| Masters | 0 | 0% | 1 | 0.40% | 0 | 0% | 0 | 0% | 1 | 0.40% |
| Total | 61 | 27% | 85 | 37% | 46 | 20% | 36 | 16% | 228 | 100% |
Table 3: Demographics of respondents per region.
Designations and titles
A total of 19 designations of nursing cadre were interviewed. All respondents have an official designation but there was an overlap of titles between old nomenclature and the new. From the survey, the bulk of nursing workforce is enrolled midwives at 27%, enrolled nurses at 22% and nursing officer at 17%. But there is lack of clarity on the following titles: “Double trained”, “a comprehensive nurse” and “a senior and principal nurse”. Table 4 shows official designations.
| S. No. | Designation | Number | % Age |
|---|---|---|---|
| 1 | Midwife | 61 | 27% |
| 2 | Enrolled Nurse | 51 | 22% |
| 3 | Nursing Officer | 38 | 17% |
| 4 | Enrolled midwife | 21 | 9% |
| 5 | Registered Nurse | 12 | 5% |
| 6 | Nursing Assistant | 10 | 4% |
| 7 | Comprehensive nurse | 9 | 4% |
| 8 | Assistant Nursing Officer | 6 | 3% |
| 9 | Double | 4 | 2% |
| 10 | Senior Nursing Officers | 4 | 2% |
| 11 | Registered midwife | 3 | 1.30% |
| 12 | Intern nurse | 2 | 0.90% |
| 13 | Assistant Nursing Officer Midwifery | 1 | 0.40% |
| 14 | Assistant health tutor | 1 | 0.40% |
| 15 | Clinical instructor nursing | 1 | 0.40% |
| 16 | Double trained but appointed as a senior (Registered nurse/midwife) | 1 | 0.40% |
| 17 | Enrolled Comprehensive nurse | 1 | 0.40% |
| 18 | Principal Nursing Officers | 1 | 0.40% |
| 19 | Midwifery Clinical instructor | 1 | 0.40% |
Table 4: Official designations of respondents.
Appointments and promotions
43% percent of newly recruited nurses and midwives are promoted within 2 years of service, 23% between 3 to 5 years of service and 34% after 5 years (Table 5). The average duration of service of a nurse or midwife was found to be 10 years, ranging from 1 to 39 years (Table 6). Most nurses do not practice at their level of training.
| Total | Central | Eastern | Northern | Western | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| 1-2yrs | 24 | 43% | 4 | 7% | 7 | 13% | 6 | 11% | 7 | 13% |
| 3-5yrs | 13 | 23% | 10 | 18% | 1 | 2% | 1 | 2% | 1 | 2% |
| Over 5yrs | 19 | 34% | 9 | 16% | 5 | 9% | 5 | 9% | 0 | 0% |
Table 5: Proportion of respondents not promoted before and after 5 years.
| Average | Max | Min | Standard Deviation | |
|---|---|---|---|---|
| Central | 13 | 33 | 0 | 8 |
| Eastern | 11 | 39 | 1 | 9 |
| Northern | 9 | 29 | 0 | 8 |
| Western | 8 | 31 | 1 | 7 |
| National | 10 | 39 | 0 | 9 |
Table 6: Number of years spend before promotion.
A member of the Heath Service Commission said, “Many nurses have upgraded but they are still working as enrolled nurses, because the structure doesn’t allow it (promotion)”. A midwife said, “The challenge and puzzle in our profession is that the majority of us are diploma holders but we are still appointed as enrolled (certificate) nurses.”
Human resource planning is decentralized, which complicates a nation-wide coordinated process of promotions. The staffs of a hospital or district who go on long study leave continue getting salary, in effect blocking recruitment and promotions of others.
A member of the Health Service Commission said, “If Kyegegwa district allows its nurses to go for training, they (those nurses) will continue earning salary but will not be delivering services. But Kyegegwa will have no money to recruit or to promote other staff in their place.”
Training and professional development
From the survey, 47% of respondents were certificate nurses and midwives, 45% diploma, 7% bachelors and 1% with masters (Figure 1).
It roughly represents the makeup of the nursing work force in the country. Most of them (75%) said their training was adequate and 95% reported that it was relevant. But they still said they needed more skills in management, leadership, computer science, counseling and various specialized ields (Figure 2). A good proportion of nurses and midwives (57%) had recently undergone short courses in COVID-19 management, immunization, HIV prevention and management, neonatal care, integrated child care and management, first aid and family planning. These courses were funded and conducted by NGOs and bilateral organizations.
The nursing profession faces challenges in progressing to the top. Respondents were unclear about the criteria for promotions. They demanded for explicit criteria for professional progression. A midwife who left government and trained to doctorate level and now teaches midwifery at a university said, “I cannot explain government criteria of professional development of nurses. I took over twenty years in government service but I left without being promoted. The rest of my colleagues I qualified with in 1990s are still there at the same level.”
Whether one progresses or not in the nursing and midwifery profession is mostly personal initiative, not through a planned talent development program of the government. A senior lecturer said, “I started as a midwife in 1987 in Mulago School of Nursing and Midwifery. Then I upgraded to a bachelor’s midwife from one university. A ter that I did a master’s in midwifery and women’s health at another university. I’m now (2022) pursuing a PhD.”
In rare cases there is need to upgrade urgently through further training to ill posts that have fallen vacant. This has been noted by many respondents. A respondent said, “The supervisor is upgrading because both the senior and principal nursing officer posts have fallen vacant.”
The pathway of progression in the profession is a big challenge. A respondent from Uganda Nurses and Midwives Council has said, “It is good that we now have PhDs. But they will not be used because the career path is too long. Imagine you pursue a certi icate for two and a half years; you wait to be promoted, get a job to get experience. So now you go for a diploma for four years, then you go through lengthy registration and start looking for a job. At the end of the day nurses retire or die without using their degrees.”
A respondent was of the view that for the nursing education to be streamlined, all nursing curricula need to be revised and said, “Before we even train, we need to revise the curricula because you ind certi icate, diploma, bachelor, masters and whatnot; but what is the difference in the content of these curricula?”
Licensing of nurses and midwives
A respondent explained that the council has five functions:
• To accredit nurse training institutions
• To validate students minimum entry requirements
• To visit areas of practice to see whether they comply with the minimum professional standards
• To renew licenses of nurses and midwives every three years
• To enroll and register nurses and midwives
There is a huge backlog of nurses and midwives with expired or no licenses, with some continuing to practice. A respondent from the council explained, “We find many nurses whose licenses have expired but they are working. So usually, we encourage them to go and renew, we tell them to go to their nearest satellite centre.”
Nurses and midwives view the Uganda Nurses and Midwives’ Council (UNMC) as a “stumbling block” because of its long process of registration and licensing and the charges involved. A respondent said, “Our number two challenge is the council. It charges a stamp tax which has been raised to Shs 100,000. And you need even more money for verification, licensing and renewal of all certificates. You certify like five papers: School certificates, professional certificates, licenses from the councils. People line up and get sick”.
This problem was confirmed by a respondent from UNMC, “Our work (in the council) depends on how fast UNMEB is able to process exam results because we can’t do without the results. Also, it depends on how fast you are able to get your certificate and (exam) results slip. At times, we allow schools to give you a testimonial and if it’s urgent you book for an interview. If you delay to book with us, you will definitely delay (to get a license). People spend two years because they did not book. At times students have debts of school fees. They are not given their UNMEB (Uganda Nurses and Midwives’ Examination Board) documents, so they can even spend five years without a license”.
Quality of nursing services
Regarding public outcry about poor nursing standards, a respondent explained that this was due to:
• Overwhelming student numbers which make it difficult to do proper training
• The transition from student to nurse is poor and
• Certificate and diploma nurses do not do internship, which is only done by graduate nurses
A respondent at UNMC explained that poor quality nursing due to poor training, and in particular inadequate transition from class to the practical clinical work. She said, “The greatest challenge of (nursing) quality is the training. The number of students is overwhelming in schools. You can have like 600 students in a class. How do you provide clinical guidance? Parents are desperate to train their children. When students come out of the training and get jobs, they meet challenges in their practice. Another thing is that, transitioning of a nurse from the class to the clinicals is not done at all.”
Supervision
Different organizations, programs and agencies carry out supervision of nurses and midwives. But each entity caters for only a specific aspect of health care. It is not clear how the supervision is coordinated to see if all aspects are covered. Supervisors of nurses by level are presented in Table 7 below. A respondent said, “District officials sometimes check on the services we offer. The ministry also carries out supervision. Different teams come at different intervals checking different things. Every month we tend to have a team that comes to see how we offer health services.”
| Rank | Number | % |
|---|---|---|
| Senior nursing officer | 77 | 35% |
| Principal nursing officer | 31 | 14% |
| Medical doctor | 29 | 13% |
| In-charge | 15 | 7% |
| Nursing officer | 15 | 7% |
| Assistant nursing officer | 7 | 3% |
| Clinical officer | 7 | 3% |
| Registered nurse | 6 | 3% |
| Tutor | 6 | 3% |
| Registered midwifery/set mother | 4 | 2% |
| Chief nursing officer | 3 | 1% |
| Director | 3 | 1% |
| District health officer | 3 | 1% |
| Hospital administrator | 3 | 1% |
| Lab technician | 2 | 1% |
| Senior midwife | 3 | 1% |
| Ward in charge | 2 | 1% |
Table 7: Ranks of supervisors.
The issues that come up during supervision include bribery, inside trading, poor attendance of duty and lack of leadership at departmental level and extortion of money from patients. Other issues are poor supervision, poor quality of services, time management, lack of protective gear, infection control, late coming, poor documentation of records, stock-outs, low staffing levels, poor attitude to work, poor remuneration, poor patient management, gaps in knowledge and skills, COVID-19 and confidentiality.
Motivation to work
From the survey, 73% of respondents said they were motivated to work. Of these, the most highly motivated were 31% and moderately motivated 57%, making a total of 88%. The factors motivating nurses and midwives included: Love for people and profession 81%, money and benefits 53% and prestige 13%. Motivating factors were the provided accommodation, allowances, functional medical equipment, taking good care of a patient, having all the necessary drugs and sundries, lunch allowance, appreciation from patients, positive outcome of patient care, heading a department, good environment to work and presents and gifts (Table 8). A big was de-motivator found to be the unfair and low salary. A respondent said, “I would be greatly motivated if I was paid at my qualification. But we are paid at a lower qualification.”
| Motivating Factor | Number of respondents | % |
|---|---|---|
| Love for profession | 135 | 81% |
| Love for people | 89 | 53% |
| The money and other benefits I get | 36 | 22% |
| Prestige that comes with the profession | 22 | 13% |
| Other | 31 | 19% |
| Promotion | 4 | 2% |
| Appreciation | 6 | 4% |
| Teamwork | 5 | 3% |
Table 8: Motivating factors.
Key demotivating factors (Table 9) were: Low salary (53%), lack of appreciation (11%), lack of promotion (17%), delayed salary (8%) and heavy workload (4%). Other demotivating factors were: Lack of accommodation, “I don’t like the profession”, “I don’t like people” and “I want to do something else”.
| De-motivating factors | Number of respondents | % |
|---|---|---|
| Salary and other benefits are too low | 120 | 53% |
| Lack of appreciation | 24 | 11% |
| Lack of promotion | 21 | 9% |
| Delayed salary | 19 | 8% |
| None | 13 | 6% |
| Workload | 10 | 4% |
| Lack of accommodation | 6 | 3% |
| Don’t like the profession | 3 | 1% |
| Don’t like people | 2 | 1% |
| I want to do something else | 3 | 1% |
Table 9: Demotivating factors.
Hard-to-reach areas
A hard-to-reach area was variously defined as “distant from home or Kampala (capital city)”, a place with difficult or few means of transport and where there are no good schools for the children of the nursing staff. Other definitions included absence of amenities such as running water, electricity, telephone networks and internet. Lack of banks to access salaries, hostile communities, cultural shock and communities that reject public health out-reach services were regarded as hard-to-reach areas. In the Table 10 for nurses who said they were in hard-to-reach areas. Suggested solutions for attracting staff to such areas were: A bigger basic pay, hard-to-reach allowance, provision of means of transport, guaranteed accommodation and support for income generating enterprises or side jobs.
| Central | Eastern | Northern | Western | Total | % | |
|---|---|---|---|---|---|---|
| No | 46 | 67 | 39 | 26 | 178 | 78% |
| Yes | 15 | 18 | 7 | 10 | 50 | 22% |
| Total | 61 | 85 | 48 | 36 | 228 | 100% |
Table 10: Are you working in a hard to reach area? Results by region of the country.
Absenteeism
About 61% of all staff was on “leave”, which in reality is absenteeism. The reasons for absenteeism include: Taking children back to school, going to the bank, having patients at home, attending burials of relatives or friends, having sick parents at home and other emergencies. Other reasons included long distances from home to the place of work, attending to do their own businesses to augment their meagre salary and low morale to work. Absenteeism is a public sector nuisance, which was not found among nurses and midwives working in private facilities. Arrangements often made by nurses and midwives to try and rectify their absence from work include asking a working colleague to stand in, asking a colleague not on duty to stand in, or asking the supervisor to find a person to cover their duty.
Integrity and ethical conduct
About 68% of respondents agreed that they had received gifts or inducements to provide a service (Table 11).
| Central | Eastern | Northern | Western | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | 20 | 9% | 22 | 10% | 14 | 6% | 16 | 7% | 72 | 32% |
| Yes | 41 | 18% | 63 | 28% | 32 | 14% | 20 | 9% | 156 | 68% |
| Total | 61 | 27% | 85 | 37% | 46 | 20% | 36 | 16% | 228 | 100% |
Table 11: Have you received gifts or inducements for work? Results by region.
Thirty-one percent said they did something they were not sure about and did not consult or seek for assistance (Table 12). These actions included misdiagnosis, connecting a patient to a nebulizer, neonate resuscitation and catheterization. About 13% of respondents reported they actually injured patients and even caused death. These grievous actions included billing a caretaker after the death of a patient, death of a baby, shouting at a patient, being rude to a patient and having a misunderstanding with a client. A respondent said, “The first patient I lost was a baby in Mulago Hospital. I started asking myself, what did I do or not do? What could we have done? I have not forgotten that baby”.
| Central | Eastern | Northern | Western | Total | ||||||
|---|---|---|---|---|---|---|---|---|---|---|
| No | 43 | 19% | 59 | 26% | 32 | 14% | 22 | 10% | 156 | 68% |
| Yes | 18 | 8% | 26 | 11% | 14 | 6% | 14 | 6% | 72 | 32% |
| Total | 61 | 27% | 85 | 37% | 46 | 20% | 36 | 16% | 228 | 100% |
Table 12: Did you do anything you were not sure about? Results by region.
Corruption, extortion and bribery
Corruption as understood in Uganda is obtaining or achieving something using illegal or criminal means. Bribery is a form of corruption where someone willingly pays you for a service or product which is supposed to be free or at a lower price. Extortion is forcing somebody to pay you for a service which should be free or at a lower cost. Among health workers, including nurses and midwives, corruption, bribery and extortion have become institutionalized method or practice at work. These methods are used in all aspects: To get a recommendation for promotion, to get appointment in public service, to get study leave, to get admitted into training or further studies, to get medicine, to get a bed in the ward, to get anything. The practice is so common that it is now done openly. Patients and students in training see what goes on and they take it to be normal practice of health service delivery.
One respondent had this to say, “We hear there is scholarship at the nurses’ union but when you try to apply for it you will get tired. The one who calls himself president will tell you, if you have (Shillings) two million I will fix your name”.
Another respondent complained, “We teach nursing students and we sign the log books. Our pay comes to the administration but it does not reach us. One time we completely refused to sign the books. They told us that the money has first to go to the consolidated account. It is now four years and we have not seen the money”.
Another respondent revealed, “I found a man waiting around and asked him, what is the problem? He told me the doctor has taken my “Shilling” 200,000 for an operation but my wife has delivered normally on her own. I want my money back”.
Yet another respondent said, “A medical officer was doing ward-round and nurses guided him, ‘doctor you have jumped a bed’. This man (doctor) had jumped that bed intentionally because that patient had refused to give him money”.
Welfare of nurses and midwives
Respondents observed that nurses face physical and mental challenges as a result of their work. A respondent said, "At times they push beds; at times the equipment does not roll. I did a study in Mulago Hospital on the musculo-skeletal conditions among nurses. A number of nurses had backache because of lifting things".
Regarding the welfare of nurses, a respondent said, “The other thing which is rarely talked about is the care of the carer. When a health worker falls sick or has health challenges, who cares for them?”
Performance of nurses and midwives
A self-assessment of own performance showed that 57% scored themselves as performing “very well” and 42% as “well”. And 46% said they were recognized for their good performance. The recognition included words of praise, money, a certificate, a medal and promotion. They recommended that in the future good performers could be rewarded with further training, material things and recognized as national heroes. But to build up for good performance, apart from creating a supportive environment (such equipment, supplies, utilities and motivated staff), there is need to recognize the staff’s effort, give them respect and support and mentor them. A respondent said, “Determinants of nursing performance should include three things:
• Do you recognize people’s efforts?
• Do you give them the respect they deserve?
• Do you reach out to them in form of support supervision and mentorship?
Challenges
The study brings out challenges faced by nurses and midwives, the strengths, opportunities and special considerations in nursing and midwifery, and priorities for planning.
Inadequate number of working nurses and midwives in the face of their overproduction is an existential paradox. Despite a large number of nurses and midwives known to be out of work, unemployed or doing petty trade, the number employed in health units is very low and inadequate. Official figures of the MOH put staffing levels at about 57% [30-32]. In addition, employment conditions are unfair and difficult and do not measure up to the public service standing orders [33]. Nurses and midwives are underpaid relative to comparable health workers. Their benefits are too low to meet basic needs. Their work is not well appreciated. Often, they are overworked in a situation of heavy workload and few staff. Most of them are not promoted throughout their career and retire at the level of the very first appointment. Even those who endeavor to study to attain higher skills are not recognized or rewarded through appreciable increase in salary.
Poor public image and status and belittlement of nurses and midwives are a major challenge. The public has a poor image of nurses and midwives and accord it low status. This is reinforced by the low pay and poor work conditions that they are subjected to both in the government and the private sector.
The quality of nursing and midwifery services has got worse over recent years. This is attributed to poor quality nursing arising from sub-standard training. Classes are almost always overcrowded and effective learning is almost impossible. Entry requirements into the nursing schools are low in some of the schools. There is a very limited exposure of students to practical clinical work. Those who finish theoretical training do not go through internship. There is no transition from a student to a nurse. In addition, when they start work, they lack the basic skills of modern life, which include skills of management, computing, leadership. Most specialized nursing positions are unoccupied. Absenteeism among nurses and midwives is high at about 61%. Absenteeism has become a “normal” practice. The commonest reason for absenteeism is “looking for something to meet the ends”. This often means looking for extra cash for basic needs in the face of miserable salary and working benefits. Late coming to work is very common. Poor time management is another challenge common among all health workers.
Corruption, bribery and extortion are the unofficial methods of work. These methods include getting a recommendation for promotion, an appointment in public service, a study leave, admitted into training or for further studies, medicines for patients, admission bed in the ward for patients, and almost anything else. The practice is so common that it is done openly. Patients and students in training see what goes on and they take it to be normal practice of health service delivery. Human resource management and planning have been decentralized to districts and hospitals. They are not well coordinated, harmonized, directed and controlled centrally for equitable national distribution. Licensing is a huge frustration for nurses who want to practice. There are numerous and exorbitant charges levied on processing, registration and licensing. The processing of a license takes too long, from several months to years. The nursing license office is constantly over-crowded. However, this situation is now being addressed.
Nurses and midwives are not prepared for harsh realities of life in rural and hard-to-reach areas. There are no provisions for motivation and incentivize to those who could be attracted to go and work those areas. Nurses and midwives have described such places as geographically difficult and places that lack infrastructure, amenities and social services. The difficult areas include where communities are hostile, illiterate or not cooperative. Some communities are known to reject modern health care. Supervision of nurses is fragmented by project and different centers of authority. Supervisors do not meet to compare notes or take joint action to address the issues that they find on their supervisory visits. Inadequacy of funding also means that there are many gaps in the coverage of supervision. Nurses and midwives suffer both physical and mental trauma from work. Back pain and injury are common among nurses and midwives due mainly to pushing non-rolling trolleys and equipment and lifting heavy equipment. Moreover, those who fall sick or injured are not assured of prompt and good health care as there is no program or system to help them.
Nursing and midwifery are subsumed into health services. Not much effort has been put to develop the profession and service. Due to the low status the public and leaders have always accorded to nursing and midwifery, there has also been limited political good will to address matters of the profession. Nursing and midwifery professionals are hardly appointed in high health sector leadership positions, where political and resource allocation decisions are made. The health sector leadership is dominated by doctors and yet nurses and midwives constitute 60% of the health workforce.
Strengths and opportunities
The nursing profession constitutes up to 90% of all health workforce in Uganda [4]. The pillar of health care everywhere is nursing. The evidence of nurses who love people and their work is positive and strength in the profession. In Uganda the key institutions and regulations on nursing are in place. These only need better enforcement. The new leadership at the ministry of health is forward looking and positive. The education level of entry into nursing schools has greatly increased. Also, nurses are now more educated than before in terms of masters and doctorate degrees. The overall policy environment is positive, which include national development plans and health sector policies and strategic plans. International initiatives have also been embraced by the government. These include SGDs, UHC and WHO’s directions for the development of nursing and midwifery as a profession. The WHO is mobilizing for stronger leadership and governance, partnership and research in nursing and midwifery. Above all, the WHO initiative is to mobilize political will, without which not much can be done to improve the circumstances of nurses and midwives and their profession. Much progress has been made in building institutions for the governance and stewardship of nursing and midwifery. The creation of the department of nursing and midwifery at the MOH was a key step. The other institutions include a council for licensing, a board for nursing examinations, a union for nurses’ welfare and several other nurses’ organizations. A number of positive initiatives have been made that will go a long way in improving nursing and midwifery. These include the digitalization and regionalization of licensing and registration, restructuring of regional hospitals and salary review and rationalization. A high percentage of nursing staff have a positive attitude. They are motivated by love for people and for the profession. This attitude should be built upon to strengthen the nursing and midwifery profession. The determination of nurses and midwives to seek further training, as evidenced by the increasing trend of graduate nursing education, is a positive trend.
Specific considerations
Policy, laws and regulations: Changes will be required in the laws and policies to implement the desired direction and reforms in the nursing profession and services. A tentative list of policies and laws is suggested below. Table 13 below is a preliminary indication of policies, laws and regulatory guidelines.
| Policy | Guidelines | Laws |
|---|---|---|
| Nursing and Midwifery National Policy | Guide on continuous professional development and supervision | - |
| Advanced nursing education | Work environment guidelines | - |
| Private nursing practice | Guide on nursing specialization Nursing career guidance Guide on recognizing and rewarding performance |
Private Nursing Practice Law and Regulations |
| Partnership with organizations | Guide from the existing partnership law | Apply existing partnership laws |
| Nurse training and education policy | Nursing career guidance | - |
| Nursing research policy | Guide national nursing research agenda and program | - |
| Nursing ethics and integrity policy | To be specified and defined | - |
| Nursing welfare policy | To be specified and defined | - |
| Public/community health nursing policy | To be specified and defined | - |
Table 13: Possible policies, guidelines and laws.
A tentative research agenda in nursing and midwifery: The following are tentative areas/topics of interest in nursing research: (a) Addressing inequality in nursing services; (b) Quality improvement; (c) UHC and nursing; (d) Building a global nursing practice; (e) Evidence of outcomes of different cadres and levels of nursing care (user-friendliness, patient safety, risk management, access to care, co-ordination of services, health care utilization and cost-effectiveness of nursing care and (f) Health care delivery systems.
Career pathway and profession’s structure: Nurses and midwives should advance right from the onset of their qualification to the highest level within ten years. Just like it is for other professions, so it should be for nurses and midwives. This requires career guidance and restructuring of the training and education of nurses and their employment. It will be important to tell young nurses the possible career pathways at the start of their career. These pathways could possibly be: Clinic career, research, teaching and training, specialization, advanced nurse practice and private nursing practice.
Justification for certificate nurse or midwife: The model nurse and midwife project and other efforts have attempted to replace the certificate nurse with a higher caliber nurse. The nursing professionals have suggested that the certificate nurse be phased out and be replaced with diploma and graduate nurses. But the ministries of health and education have strongly argued for the retention of the certificate nurse because it is the “working nursing cadre” in Uganda. They argue that the certificate nurse is the most available and capable front-line cadre in contact with patients and communities. Their role and competence should only be further augmented. The new curriculum for certificate in nursing uses Competence-Based Education and Training (CBET) principles. These principles include: Learning through training; teaching based on acquiring skills in a practical and systematic manner; learning step-by-step; prior learning as well as learning on the job. CBET reduces the cost of training, improves access and relevance. The key challenge in health sector is the rapidly changing nature of skills demanded of a variety of cadres. A certificate nurse should be facilitated to grow from certificate level to diploma to bachelor’s degree, and proceed to master’s and doctorate.
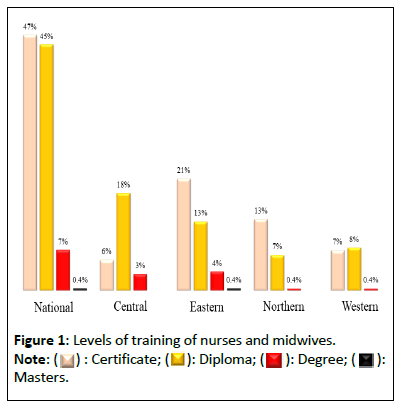
Strategic planning: The purpose of this study was to inform strategic planning. A strategic plan was developed. All issues and demands in nursing and midwifery that require to be addressed fall under 3 categories: 1) Leadership and governance; (2) Professional development and (3) Service delivery. Figure 1 provides a framework of the strategic plan consisting of the key challenges, priorities, strategic actions and the vision. The MOH is charged with the overall leadership and policy guidance, supervision and monitoring and evaluation. The MOES is responsible for the education and training of nurses and midwives. The UNMC is responsible for the development and enforcement of nursing and midwifery professional standards. MPS is charged with defining the cadres of nurses and midwives and with developing their schemes of work.
Priority areas and actions: Three broad areas of focus and corresponding actions have been delineated. First is leadership and governance of nursing profession and services. This requires leadership placements and development, particularly at the higher levels. It requires that a nursing and midwifery governance review be undertaken and recommendations therefrom implemented. There is need for a deliberate effort to mobilize political will to deal with the issues of nurses and midwives. In particular, it requires political will and assertion to address the poor image and low status of the nursing profession. It requires a public campaign and advocacy, as well as raising the nurses’ profile in leadership and society.
Second, professional development will require a review and restructuring of the entire nursing and midwifery profession, including the training and career development, continuous professional development guidelines and a deliberate focus on nursing research. Third, service delivery will require a review, harmonization and enforcement of training and service standards. A well-coordinated, comprehensive and regular supervision system has to be put in place to ensure quality nursing care. Public health nursing needs to be revived through training and deployment. A framework for the nursing strategic plan is in Figure 3.
Conclusion
The growth of nursing and midwifery as a profession has been stunted by numerous challenges. There is widespread but mistaken mindset about nursing being a low-level service to support doctors. Yet nursing is a science-based modern profession. Many countries have already developed nursing as a distinct profession, service and discipline. This study is a step in the right direction to provide evidence for planning the nursing profession and services.
Author Contributions
All listed organizations and persons contributed in the study and manuscript writing. SO conceived the paper and wrote earlier drafts. ML, JK and TM analyzed data and reviewed the report. JM, IA, AB reviewed the drafts.
Funding
The study was funded by Seed Global Health based in Uganda, Kampala and commissioned by the Ministry of Health, Government of Uganda.
Competing Interests
None declared.
Ethical Consideration
This study was done during the COVID-19 pandemic. The approval for the study was given by an ethics/technical committee of the Ministry of Health under reference number ADM.79/260/01, dated September 10, 2021. Further permission for the study was also granted by local authorities where the study was done. The study involved only nurses and nursing administrators, all of whom gave their consent to provide information. No information is attributed to any specific person or persons.
Public Contribution
No patients were involved in this study. Only nurses and midwives and nursing administrators such as professional associations, councils and boards were interviewed, or voluntarily provided information.
References
- WHO (2016) Global strategic directions for strengthening nursing and midwifery 2016-2020.
- WHO (2009) WHO global code of practice on international recruitment of health personnel.
- Steurs L, Vande PR, Delputte S, Orbie J (2018) The global health policies of the EU and its member states: A common vision? Int J Health Policy Manag 7: 433-442.
[Crossref], [Google Scholar], [Indexed]
- MOH (2018) The first Uganda national nursing and midwifery policy.
- Peterson J, Pearce PF, Ferguson LA, Langford CA (2016) Understanding scoping reviews: Definition, purpose and process. J Am Assoc Nurse Pract 29: 12-16.
[Crossref], [Google Scholar], [Indexed]
- Cunie J, Chiarella M, Buckley T (2013) An investigation of the international literature on nurse practitioner private models. Int Nurs Rev 60: 435-447.
[Crossref], [Google Scholar], [Indexed]
- Luke Chapter 10: verses 25-37 in The Holy Bible New International Version 2008 Zondervan NIV Study Bible
- MOPS (2017) Schemes of service for the nursing and midwifery cadre.
- MOH (2020) Review and restructuring of regional referral hospitals.
- MOH (2020) Human resources for health strategic plan 2020-2030.
- WHO (2016) Three-year regional prototype competence-based pre-service midwifery curriculum for Africa.
- WHO (2016) Four-year integrated nursing and midwifery competence-based prototype curriculum for the Africa region (2016).
- MOES (2019) Business, technical, vocational education and training.
- MOES (2018) Semester content outline for diploma nursing direct.
- Christnuls CD, Amstrong SI (2020) The curriculum framework for advanced practice nursing in Sub-Saharan Africa: A multi-method study. BMJ Open 10: e035580.
[Crossref], [Google Scholar], [Indexed]
- Shaibu S, Niliranga E, Eunice P, Gladys M, Rachel K, et al. (2020) Introduction of an advanced practice nurse program in Kenya: A new era in nursing education. Aga Khan University.
- WHO (2017) Enhancing the role of community health nursing for universal health coverage.
- Temane A, Poggenpoe M, Myburgh CPH (2014) Advanced psychiatric nurse practitioner ideas and needs for supervision in private practice. Curationis 37: 1161.
[Crossref], [Google Scholar], [Indexed]
- Wilson A, Averis A, Walsh K (2004) The scope of private practice nursing in an Australian sample. Public Health Nurs 21: 488-494.
[Crossref], [Google Scholar], [Indexed]
- Bany P (2001) Perspectives on private practice.
- Shaw-Battisa J, Annette F, Barbara B, Blanche S, Deborah W, et al. (2011) Obstetrician and nurse-midwife collaboration: Successful public health and private practice partnership. Obstet Gynecol 118: 663-672.
[Crossref], [Google Scholar], [Indexed]
- Wayne G (2023) Theories and theorists: The definitive guide for nurses of nursing. Nurseslabs.
- Boersema GC (2018) 10th Biennial Society of Private Nurse Practitioners Conference, 2018: Guiding the future of nursing practice. Conference Report
- Buppert C (1996) Nurse practitioner private practice: Three pitfalls to avoid. Nurse Pract 21: 32-34.
[Google Scholar], [Indexed]
- Casterle BD, Izumi S, Nelda S G, Denhaerynck K (2008) Nurses’ responses to ethical dilemmas in nursing practice: Met-analysis. J Adv Nurs 63: 540-549.
[Crossref], [Google Scholar], [Indexed]
- MOH (2019) Concept paper for strategic plan for nursing and midwifery services.
- GOU (2020) National development plan III 2020-2025.
- MOH (2015) Health sector development plan 2015-2020.
- MOH (2019) Annual health sector performance report financial year 2019-2020.
- NRM (2020) National resistance movement party manifesto 2021-2026.
- GOU (2010) Uganda vision 2040.
- MOPS (2015) Uganda government public service standing orders 2021 edition.
- MOH (2023) Strategic plan 2020-2025.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences
 Masters.
Masters.