ISSN : 2576-3911
Integrative Journal of Global Health
Challenges Affecting Health Referral Systems in Low-and Middle-Income Countries: A Systematic Literature Review
Mildred Nakayuki*1 Hasifah K. Namatovu1 Annabella H.D Basaza1
Department of Information Technology. Makerere University, Kampala, Uganda.
- *Corresponding Author:
- Nakayuki M
Department of Information Technology. Makerere University, Kampala, Uganda
Tel:0701662622
E-mail: mildrednakayuki@gmail.com, mildredcax@gmail.com
Received Date: July 25, 2021; Accepted Date: October 6, 2021; Published Date: October 15, 2021
Citation: Nakayuki M, Challenges Affecting Health Referral Systems in Low-And Middle Income Countries: A Systematic Literature Review, J of Glob Health, Vol: 5 No: 4.
Abstract
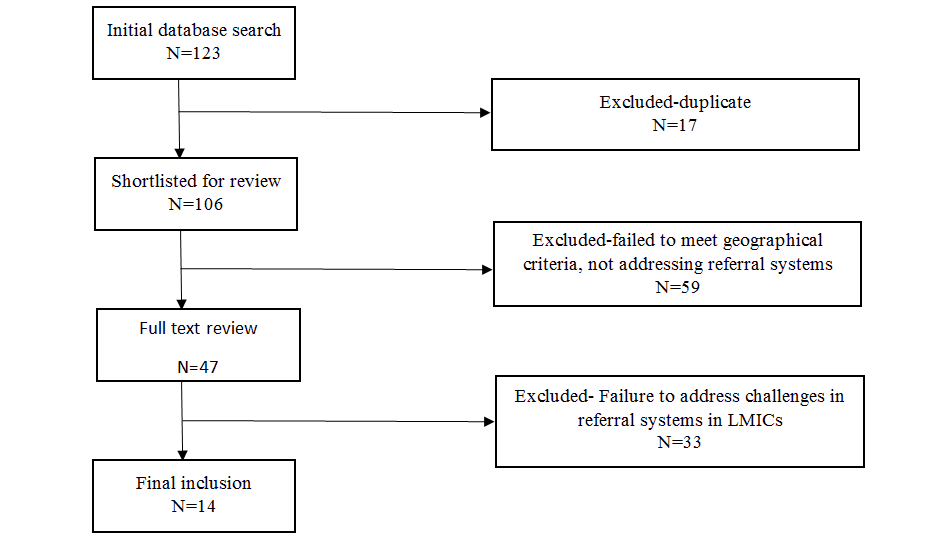
Low and middle-income countries are still facing challenges of dysfunctional referral systems which have impaired health service provision. This review aimed at investigating these challenges to understand their nature, cause, and the impacts they have on health service provision. Database search was made in Google scholar, ACM Library, PubMed health, and BMC public health, and a total of 123 papers were generated. Only 14 fit the inclusion criteria. Inclusion criteria included studies that were both quantitative and qualitative addressing challenges facing referral systems or health referral systems, studies describing the barriers to effective referral systems, and studies describing factors that affect referral systems. The review only included studies conducted in LMICs and included literature between January 2010 and February 2021. Results revealed that human resource and financial constraints, non-compliance, and communication are the key challenges affecting referral systems in LMICs. Countries that are facing these challenges need to overhaul the system and improve end-to-end communication between hospitals, improve capacity specifically in referral and emergency units, and sensitizing patients on the adherence to emergency protocols.
Keywords
Challenges, health, referral systems, low- and middle-income countries
Introduction
Referral systems play a major role in managing the patient flow from primary to secondary health units with resources beyond those available where health care was initially sought. This is crucial in any healthcare system since it plays a vital role in the management of diseases and promotes health outcomes (Gupta, Talati, Bhattacharya, & Singh, 2017). Efficient referral systems provide access to treatment and skills by coordinating different levels of healthcare through appropriate referral levels that promote health and well-being of lives (Singh, Doyle, Campbell, Mathew, & Murthy, 2016). A referral is defined as a process in which a health worker at a health system level that has insufficient resources (medications, equipment, skills) to manage a clinical condition seeks assistance from a better facility or with different resources in the same or higher level to help or take over the management of the client's case (Alaro, 2016). Patient referral involves certain criteria followed (Griffin, Nate, Rivard, Christianson, & Dusek, 2016), and beyond this, other factors influence a referral system to ensure its effectiveness [1,2].
An effective referral system is essential to save lives and ensure quality and continued health care across the various levels of health services (Give et al., 2019). This ensures a close relationship between all levels of the health system and helps to ensure patients receive the best possible health care (Afolaranmi et al., 2018). For successful referral, there must be geographical access to referral care facilities, availability of referral services, trained staff to provide quality care, affordable services, essential drugs, supplies, and equipment (Kamau, Osuga & Njuguna, 2017).
The World Health Organisation (WHO) in 2015 defined a global strategy for people-centered integrated health services to change the way health services are managed and delivered. The enjoyment of the highest attainable standard of health is one of the fundamental rights of every human being (WHO, 2006). The third sustainable development goal (SDG) is to ensure good health and well-being to increase life expectancy (Suzan & Coulibaly, 2018). This involves the existence of a well-functioning referral system that allows continuity of care across the different tiers of health (Kamau, Osuga & Njuguna, 2017)). However, referral systems in many low-and middle-income countries are weak and often challenged with systemic inefficiencies (Pittalis, Brugha, & Gajewski, 2019). These challenges affect the health system since the referral of patients from lower levels of healthcare to higher levels is identified as an integral component of the health care delivery system (Daniels & Abuosi, 2020) [3,4].
Health services in Uganda are provided under a four-tier healthcare system consisting of primary, secondary, tertiary, and quaternary with Regional Referral Hospitals (RRH) being major contributors to essential clinical health care because they provide specialist clinical services (Muwanga, 2015). Hospital services are provided by public, private not-for-profit 4, and private health institutions with a variance in the degree of specialization between hospitals. The public health facilities are divided into three groups which are general hospitals, regional referral hospitals, and national referral hospitals according to the level of services available and their responsibilities (MoH, 2010). National referral hospitals offer highly specialized medical and surgical services, advanced diagnostic services, advanced research, and training for medical doctors, nurses, and paramedical officers. Regional hospitals provide referral services and supportive supervision to the district level hospitals within each health zone which include specialized medical and surgical care, basic research, and training of nurses and paramedical officers (Lukwago & Tumwesigye, 2014). The delivery system of the health sector includes the national referral hospitals followed by regional referral hospitals to which district hospitals refer. There is a district health care delivery system with hospitals comprising of health center IVs, IIIs, IIs, and village health teams (Mujasi, Asbu, & Puig-Junoy, 2016). Lower level (level II) health centers provide preventive, promotive, outpatient curative services, and emergency maternal deliveries. Mid-level (level III) primary care facility provides all level II services plus inpatient, maternity, and laboratory services. The higher level (level IV) primary care facility provides all level II and III services, in addition to this, it provides emergency surgery, blood transfusion, laboratory services and supervises levels III and II (Lukwago & Tumwesigye, 2014). The regional referral hospitals provide all district-level services plus specialized services (MoH, 2014), the national referral hospital on the other hand provides all services provided by regional referral hospitals.
Referral services in Uganda require a patient to be referred to the next higher level in case their health condition cannot be handled at the current level of health service (Lukwago & Tumwesigye, 2014). However, this is not very effective due to the challenges faced by the referral mechanism such as poor road networks, self-referrals, lack of referral forms, limited emergency medicines, and supplies including blood for transfusion at the referral facility (MoH, Makerere University School of Public Health & Health Systems 20/20, 2012). Health facilities use various methods of referral such as a paper process referral, this is where a referral letter is written for the patient that is presented to the next referred hospital though it has limitations such as inadequate information, lost or misplaced paper records among others (Omotosho, Adegbola & Adebo, 2016) [5,6,7].
Some of the challenges in health referral systems in LMICs include noncompliance with referrals (Ilboudo, Chou & Huang, 2012), delays in referral completion which can result in delayed treatment and poor health outcomes (Peterson et al., 2004), high numbers of self-referrals (Amoah & Phillips, 2017) weak health information systems to capture referral data (Naseriasl, Janati, Amini, & Adham, 2018), and poor transport arrangements for emergency referrals (Hussein, Kanguru, Astin, & Munjanja, 2012). These challenges limit the functionality and efficiency of the referral systems. Therefore, the purpose of this review was to unravel the challenges affecting health referral systems in low and middle-income countries to understand their nature, cause and the impacts they have on health service provision [8,9].
Methodology
A systematic review of literature for studies conducted with referral systems in LMIC was done to understand the challenges affecting referral systems. This was guided by Preferred reporting items for systematic reviews and meta-analyses(PRISMA) (Moher, Liberati, Tetzlaff, & Altman, 2009). This review was conducted between January and April 2021. The searches were made in google scholar, ACM Library, PubMed health, and BMC public health for studies conducted between 2010 and 2021. Ten years is sufficient to inform us of issues affecting referral systems. The search terms used in this study include “health AND referral systems”, “health OR referral systems”, “challenges OR barriers”, “factors OR determinants”, “Uganda OR LMIC”, “health referrals OR referrals”.
The study selection criteria included both quantitative and qualitative studies addressing challenges affecting referral systems or health referral systems, studies describing barriers to effective referral systems, conducted in English, and describe factors that affect referral systems. The review only included studies conducted in LMICs. The exclusion criteria included studies not related to health referral systems, were published before 2010 and in languages other than English. Also, studies in high-income countries were not considered.
Data were extracted from the selected articles by the authors following the inclusion criteria checklist. This checklist was drafted by the authors and a data extraction form was developed which included: the author(s) name, year of publication, country, study design, sample size, study title, and the challenges identified as illustrated in Table 1. The results of the search outputs were managed using the reference manager software Mendeley, which also supported the identification and removal of duplicates to keep accurate records of the review process. The authors initially reviewed all titles and abstracts of the studies identified through the search strategy. Data and insights were not uniformly reported and were thus extracted variously from the background material, description of methods, reported results, and interpretative reflections in the discussion section of different articles reviewed in order to extract the challenges facing referral systems. one hundred and twenty-three articles were identified from the database search and only 14 articles met the inclusion criteria of this study. All articles were reviewed by all authors independently to ensure consistency. All authors unanimously shared their findings after independently reviewing the articles in order to ascertain whether the requirements were addressed. The rigor used in the selection and analysis of the articles was to a certain extent eliminate bias [10,11].
Data Review and Synthesis
Independent selections were merged and compared and 17 studies that were duplicates were removed. The authors independently reviewed the abstracts (where available) of the short-listed articles against more explicit inclusion criteria which required a description of the geographical location of the study (e.g. the country where the study was conducted), and the specific health system addressed by the study. Finally, 14 studies met the inclusion criteria as illustrated in Figure 1 below.
Results
The fourteen studies used a variety of study methods which included cross-sectional, qualitative, quantitative, and mixed methods. Four studies used a cross-sectional approach while nine studies approached the field with a qualitative approach. One study mixed their research design using both qualitative and quantitative methods. Studies were of various sizes and used between 8 and 684 participants. The largest sample size came from a research study in Ethiopia with 684 participants (Beyene, Berhanu, Hailu, Tadele & Åke, 2020). The articles were analyzed and summarized as in Table 1 below.
| Author and year | Study tittle | Study design/method | Challenges identified | Sample size/ Country |
|---|---|---|---|---|
| (Kamau, Osuga & Njuguna, 2017) | Challenges Facing Implementation of Referral System for Quality Health Care Services In Kiambu County, Kenya | Cross-sectional study methods | Poor infrastructure limiting timely access to health care, the capacity of health care workers, lack of effective information transfer and Financial resources | 271/Kenya |
| (Daniels & Abuosi, 2020) | Improving emergency obstetric referral systems in low and middle income countries: a qualitative study in a tertiary health facility in Ghana | Qualitative method | Communication barriers, poor referral transportation system, health infrastructure, and human resource issues | 89/ Ghana |
| (Amoah & Phillips, 2017) | Strengthening the Referral System through Social Capital: A Qualitative Inquiry in Ghana | Qualitative deductive methods | Limited health personnel, poor transportation, poor communication infrastructure, and finance issues | 79/ Ghana |
| (Cardoso & Long, 2019) | Strengthening referral pathways for children and adolescents affected by sexual violence | qualitative methods | failure to receive the correct documentation about the patients, failure to make referrals correctly, financial costs, limited staff capacity. | 199/ Kenya and Uganda |
| (Brondani et al., 2016) | Challenges of referral and counter-referral in health care in the workers’ perspective | qualitative methods | lack of communication between health workers, lack of knowledge regarding the services, lack of continuing education, absence of feedback from the services to which the service user was referred, and the lack of responsible professionals involved in health care | 8/ Brazil |
| Eskandari, Abbaszadeh & Borhani, 2013 | Barriers of referral system to health care provision in rural societies in Iran | qualitative study methods | The referral system is far from the ideal state, lack of adequate governmental referral system, lack of connection between different levels of the referral system, self-referential or bypassing the referral system, and insufficient knowledge about the referral system | 26/ Iran |
| (Beyene, Berhanu, Hailu, Tadele & Åke, 2020) | Insufficient referral practices of sick children in Ethiopia shown in a cross-sectional survey | cross-sectional study methods | Lack of referral logistics, missing referral forms, Limited transportation and ambulances, and lack of feedback on the referred cases from higher levels | 684/ Ethiopia |
| (Nango, Mwangi & Oluoch, 2019) | Determinants of a functional referral system in Kisumu county, Kenya patients’ perspective | cross-sectional study methods | congestion of patients at the health facilities, limited resources to deal with the voluminous patients, slow rate of service delivery to the patients | 338/ Kenya |
| (Macintyre et al., 2011) | Barriers to Referral in Swaziland: Perceptions from Providers and Clients of a System under Stress | cross-sectional study methods | Poverty, lack of transport, quality of health care, long lines or congestion at the referral sites, client‘s perception of poor care, lack of good communication in the system, lack of providers at the referral site, long waiting lines at referral sites, Lack of client understanding and lack of confidentiality | 254/ Malawi |
| (Chitsa, 2019) | Factors Affecting the Provision of Referral Services at the Primary Level of Health Care in Zomba District in Malawi | qualitative study methods | Lack of transport facilities, poor road network, Lack of public secondary level of care facility, communication challenges, delay and non-compliance with the referral process, shortage of skilled health care providers, equipment, and drugs | 34/ Malawi |
| (Give et al., 2019) | Strengthening referral systems in community health programs: a qualitative study in two rural districts of Maputo Province, Mozambique | qualitative study methods | Some patients do not receive preferential treatment as expected, Patient failure to take up referral and demotivation among health care providers. | 30/ Mozambique |
| (Demissie, 2020) | Implementation and Challenges of Referral System in Public Health Centers of Addis Ababa, Ethiopia,2019 | Mixed-methods | Lack of information and inadequate consultation, unnecessary referral for drug/ laboratory examination, incomplete referral form, poor coordination and communication between health centers and the receiving hospital, reluctance, and poor staff motivation. | 22/ Ethiopia |
| (Naseriasl, Janati, Amini & Adham, 2018) | Referral system in rural Iran: improvement proposals | qualitative study methods | insufficient communication between primary health care providers and specialists | 74/ Iran |
| (Oduro-mensah, Agyepong, Frimpong, Zweekhorst & Vanotoo, 2021) | Implementation of a referral and expert advice call Center for Maternal and Newborn Care in the resource-constrained health system context of the Greater Accra region of Ghana | qualitative study methods | inadequacy of human resources, unavailability of referral beds, poor health infrastructure, lack of recurrent financing, and emergency referral transportation | 372/ Ghana |
Table1: Challenges facing health referral systems reviewed from related studies.
Discussion
The review revealed that referral systems in LMICs continue to face challenges that affect health outcomes. These challenges vary from one country to another. The authors unanimously agreed to thematize the findings. After a rigorous process (that also involved an expert who was not an author), the authors concluded with four themes, namely, human resource constraints, financial constraints, non-compliance issues, and communication challenges as illustrated below in table 2.
| Theme | Challenges |
|---|---|
| Human resource constraints | Lack of staff motivation, limited capacity of healthcare providers, and poor health care provided. |
| Financial constraints | Poor infrastructures and financial issues |
| Non-compliance | Non-compliance to the referral system and congestion of patients |
| Communication challenges | Limited patient details, lack of coordination, and poor communication |
Table2: Categorization of the challenges affecting referral systems.
Human resource constraints. The inadequacy of human resources in the referral units has been identified as a challenge to referral systems in LMIC. Patients do not receive preferential treatment as expected and others fail to take up the referral. The existence of limited human resources among health care providers affects the quality of health care provided (Oduro-mensah et al., 2021). This affects the quality of services offered due to the inadequate staff. The availability of human resources such as skilled health care providers enables the provision of high-quality services. Some health care providers at the referral sites are demotivated which affects their professional competence and affects the referral systems (Give et al., 2019). Lack of motivation among the existing health workforce like doctors, nurses, laboratory technicians results in a delay to offer service and absenteeism which has dire consequences to the referral system. Ensuring health care providers are skilled, available in required numbers, and motivated improves the level of commitment and health outcomes [12,13].
Financial constraints. Several studies cited limited funds as a challenge affecting the operation of the referral system. Limited finances affect health service delivery (Amoah & Phillips, 2017; Cardoso & Long, 2019) With limited financial resources, procuring equipment, medicines, and supplies essential in health service delivery is hard. Costs associated with getting better health infrastructures in places such as roads and ambulances are inadequate which limits timely access to health care (Kamau, Osuga & Njuguna, 2017). This results in system inefficiency since the equipment is limited to handle the available referred patients [14,15].
Non-compliance. Failure to comply with the existing referral system by the patients such as self-referential or bypassing affects the referral process. Some patients don’t get referral services on the same day as referred and a few referrals do not continue to the next level of health care hence consequently affecting the referral system (Chitsa, 2019). This results in poor planning for the patients at the referral facilities. There might be limited resources to deal with the voluminous patients at a given health facility (Nango, Mwangi & Oluoch, 2019). For cases where patients do not follow referral as recommended by the referring provider, congestion and long queues become eminent.
Communication challenge. Lack of communication between referring physicians and specialists hinders the sharing of patient information across the different health units. Referral systems in LMICs continue to face challenges of poor communication between health workers across various levels of health (Brondani et al., 2016; Chitsa, 2019; Daniels & Abuosi, 2020; Demissie, 2020; Macintyre et al., 2011). Poor coordination and linkage between the health centers affect the delivery of continuous care (Demissie, 2020). This is very vital in the referral process because it creates a link for continued care from one level to another. Limited communication affects the sharing of patient details. Failure to receive the correct documentation about the patients affects the service offered at the next healthcare level (Cardoso & Long, 2019). This is because the referral forms that accompany the patient has limited details which may be imperative for the following level of treatment. Effective communication integrates specialist’s recommendations appropriately understandable to the patient and consistent with the patient’s healthcare needs at all referral levels [16,17].
The implication of the study
The knowledge obtained from this review is essential in informing policy and highlighting the hurdles that health facilities face in their day-to-day execution of activities. Upon this discovery, health institutions will formulate policy frameworks to govern the referral process.
The knowledge will enable health facilities to improve referral services by addressing the challenges that the review points out. These findings will also enable users to get informed of the challenges in the referral process hence helping them comply with the referral process [18].
Limitation of the study
This study is limited to only challenges affecting health referral systems in low and middle income countries. The findings and the implications of the study were based on this information obtained from the selected articles in the LMIC.
Recommendation and Conclusion
Future research should delve into contextual barriers affecting referral systems in LMIC’s. This Attention should be given to the challenges affecting healthcare providers who are key players in the referral process. In conclusion, referral systems in LMIC are not so effective to deliver good health due to challenges they face, and addressing them would enable good health services rendered.
References
- Afolaranmi, T. O., Hassan, Z. I., Filibus, D. I., Al-mansur, U. A., Lagi, L. A., Kumbak, F. D., … Chirdan, O. O. (2018). Referral Systemâ?¯: An Assessment of Primary Health Care Centres in Plateau State , North Central Nigeria. World Journal of Research and Review, 6(1), 82–86.
- Alaro, N. L. (2016). Effective functional referral system. Academia.Edu, 20.
- Amoah, P. A., & Phillips, D. R. (2017). Strengthening the referral system through Social Capital: A qualitative inquiry in Ghana. Healthcare, 5(4), 80.
- Beyene, H., Berhanu, D., Hailu, D., Tadele, H., & Åke, L. (2020). Insufficient referral practices of sick children in Ethiopia shown in a cross-sectional survey. (October 2019), 1867–1874.
- Brondani, J. E., Leal, F. Z., Potter, C., Marion, R., Noal, C., & Perrando, S. (2016). Challenges of referral and counter-referral in health care in the workers’ perspective. 21(1), 1–8.
- Cardoso, I. de B., & Long, S. (2019). Strengthening referral pathways for children and adolescents affected by sexual violence.
- Chitsa, B. (2019). Factors Affecting the Provision of Referral Services at the Primary Level of Health Care in Zomba District in Malawi. Texila International Journal of Public Health, 1–12.
- Daniels, A. A., & Abuosi, A. (2020). Improving emergency obstetric referral systems in low and middle income countriesâ?¯: a qualitative study in a tertiary health facility in Ghana. 3, 1–10.
- Demissie, T. M. (2020). Implementation and Challenges of Referral System in Public Health Centers of Addis Ababa , Ethiopia , 2019. (June).
- Eskandari, M., Abbaszadeh, A., & Borhani, F. (2013). Barriers of referral system to health care provision in rural societies in iran. Journal of Caring Sciences, 2(3), 229–22936.
- Give, C., Ndima, S., Steege, R., Ormel, H., McCollum, R., Theobald, S., … Sidat, M. (2019). Strengthening referral systems in community health programs: A qualitative study in two rural districts of Maputo Province, Mozambique. BMC Health Services Research, 19(1), 1–11.
- Griffin, K. H., Nate, K. C., Rivard, R. L., Christianson, J. B., & Dusek, J. A. (2016). Referrals to integrative medicine in a tertiary hospitalâ?¯: fi ndings from electronic health record data and qualitative interviews.
- Gupta, A. K., Talati, S., Bhattacharya, S., & Singh, A. (2017). Health System Strengthening-Focussing on Referralsâ?¯: An Analysis from India. 2(4), 2–4.
- Hussein, J., Kanguru, L., Astin, M., & Munjanja, S. (2012). The Effectiveness of emergency obstetric referral interventions in developing country settingsâ?¯: A systematic review. 9(7). Ilboudo, T. P., Chou, Y., & Huang, N. (2012). Compliance with referral for curative care in rural Burkina Faso. (May 2011), 256–264.
- Kamau, K. J., Onyango-osuga, B., & Njuguna, S. (2017). Challenges facing implementation of referral system for quality health care services in Kiambu County , Kenya. IMedPub Journals, 4(1).
- Kamau, K. J., Osuga, B. O., & Njuguna, S. (2017). Challenges Facing Implementation Of Referral System For Quality Health Care Services In Kiambu County, Kenya. Health Systems and Policy Research, 04(01), 1–8.
- Lukwago, A., & Tumwesigye, E. (2014). The Uganda Hospital and Health Centre IV Census Survey. 224.
- Macintyre, K. C. E., Megan Littrell, Hotchkiss, D. R., Mndzebele, S., Rejoice Nkambule, Malima, B., … Kemerer, V. (2011). Barriers to Referral in Swazilandâ?¯: Perceptions from Providers and Clients of a System under Stress Barriers to Referral in Swazilandâ?¯: Perceptions from Providers and Clients of a System under Stress. World Medical & Health Policy.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences