A Rare Presentation of a Rare Disease - Primary Hyperparathyroidism Presenting as Polyarthritis - A Case Report
Dushantha Madegedara*, Asela Rasika Bandara, Rathnayake RMDHM and Samadara Nakandala
Respiratory Unit 2, Teaching Hospital, Kandy, Sri Lanka
- *Corresponding Author:
- Dushantha Madegedara
Consultant Respiratory Physician
Respiratory Unit 2, Teaching Hospital
Kandy, Sri Lanka
Tel: +94 812 222 261
E-mail: dmadegedara@yahoo.com
Received Date: 03 January 2018; Accepted Date: 12 March 2018; Published Date: 19 March 2018
Citation: Madegedara D, Bandara AR, Rathnayake RMDHM, Nakandala S (2018) A Rare Presentation of a Rare Disease - Primary Hyperparathyroidism Presenting as Polyarthritis - A Case Report. Endocrinol Res Metab Vol. 2 No 1:8.
Copyright: © 2018 Madegedara D, et al. This is an open-access article distributed under the terms of the creative Commons attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Primary hyperparathyroidism is due to inappropriate over secretion of parathyroid hormone by parathyroid glands. It is often diagnosed by routine biochemical screening. Advance disease can cause multiple complications involving renal, musculoskeletal, gastrointestinal and neuropsychiatric systems. Polyarthritis is a rare presentation of primary hyperparathyroidism. Chest pain and dyspnoea are two common symptoms of various pathological conditions found in respiratory units. Detailed analysis of clinical and investigation findings is utmost important to arrive at the proper diagnosis.We report a 45 year old female who had presented with arthritis involving multiple large and small joints for three years. She had been diagnosed as sero-negative rheumatoid arthritis and commenced on disease modifying anti-rheumatic drugs. She presented to us with non-specific chest pain and shortness of breath associated with poorly controlled joint pain and found to have severe hypercalcaemia with multiple lytic lesions and a pathological fracture. The diagnosis of rheumatoid arthritis was revised and excluded, and arthritis was recognized as the presenting feature of primary hyperparathyroidism following extensive evaluation. This case illustrates a rare presentation of a rare disease. The diagnosis of primary hyperparathyroidism is often delayed due to non-specific nature of symptoms in places without routine biochemical screening. Articular manifestations can occasionally be the presenting complains of patients with primary hyperparathyroidism. It may mimic many common conditions with arthritis. Hence, a thorough history combined with clinical examination is utmost important for physicians to arrive at proper diagnosis.
Keywords
Hyperparathyroidism; Polyarthritis; Rheumatoid arthritis; Pathological fracture
List of Abbreviations
PTH: Parathyroid Hormone; PHPT: Primary Hyperparathyroidism; DMARDs: Disease Modifying Anti-rheumatic Drugs
Introduction
Parathyroid hormone (PTH) secreted by four parathyroid glands is the principal regulator of calcium homeostasis [1]. Primary hyperparathyroidism (PHPT) is defined as hypercalcaemia with elevated or inappropriately normal PTH levels due to over activity of one or more parathyroid glands. It commonly occurs after the age of 50 years with female predominating three to four fold [2].
Solitary parathyroid adenomas are responsible for 85% of cases of PHPT. The majority of the rest is due to hyperfunction of multiple glands in the form of adenomas or hyperplasia, while <1% of cases are related to parathyroid carcinomas [3]. Though PHPT is usually a sporadic disease, familial hyperparathyroid syndromes such as multiple endocrine neoplasia I and IIA, are diagnosed in <5% of cases [4].
Primary hyperparathyroidism is diagnosed early and asymptomatic stage in countries with routine biochemical screening compared to resource poor setting, where it is more likely to present with complications [2]. Even though many patients complain of fatigue, memory loss, lack of concentration, depression, myalgia and gastroesophageal reflux, non-specific nature of symptoms hinders the diagnosis of PHPT at early stage [5]. Advanced PHPT can present with renal, musculoskeletal, gastrointestinal, neuromuscular and psychiatric manifestation.
Increased bone turn over leading to reduced bone mineral density, osteoporosis and ostitis fibrosa cystica are well recognized skeletal complications of PHPT. Arthralgia and arthritis have been described in PHPT due to gout, pseudogout, juxta-articular erosison, traumatic tenosynovitis, periarthritis, and pericapsular calcification [6]. But, arthritis simulating rheumatoid arthritis as the presenting feature of PHPT has been reported in literature only rarely [7-10].
We describe a case of PHPT presented predominantly with articular manifestations which was misdiagnosed as rheumatoid arthritis resulting in many complications of advanced disease.
Case Presentation
45 year old Sri Lankan Sinhalese female presented with 3 year history of multiple joint pain and swelling. Pain began at right hip joint and subsequently involved bilateral knees, left shoulder, left elbow and multiple small joints of hands in an asymmetrical distribution. Pain was sometimes associated with joint swelling, but there was no redness. She also had noticed morning stiffness of hands lasting for approximately 15 minutes. She had consulted rheumatology department initially with these symptoms. Investigations done during initial evaluation showed sedimentation rate- 35 mm, leucocytes count- 8800/mm3, hemoglobin- 12.4 g/dl, platelet- 305,000/mm3, and negative rheumatoid factor. Based on these, she was diagnosed with sero-negative rheumatoid arthritis and started on treatment with Methotrexate 10 mg weekly, sulfasalazine 500 mg thrice daily, and non-steroidal anti-inflammatory drugs. But it failed to achieve a significant improvement of her symptoms.
Later on, she developed a mechanical type lower backache, which impaired her quality of life significantly. Her illness was not associated with alopecia, photosensitivity, oral ulcerations, Reynaud’s phenomena, thickening of skin, dry eyes or dry mouth suggestive of other autoimmune rheumatological diseases. But she had noticed generalized muscle pain and proximal muscle weakness.
She developed right sided renal calculi 1.5 years before the current evaluation, which was complicated with single episode of urinary tract infection. She was not investigated further seeking for aetiology of renal calculi at this situation. As the disease progressed, she noticed bone pain and lumps involving bilateral tibia 1.5 years ago. On inquiry she revealed polyuria, nocturia, polydipsia, constipation and symptoms of gastroesophageal reflux disease for last 2 years.
She presented to our unit with non-specific chest pain and shortness of breath for two months duration.
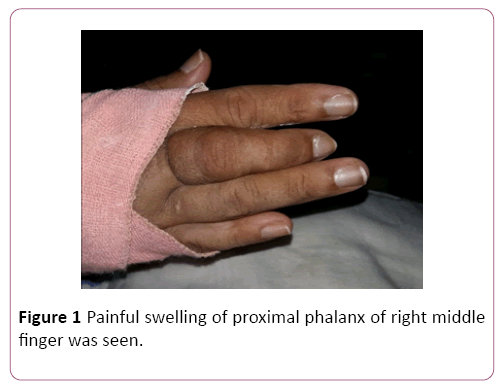
An examination on current admission revealed averagely built female in distress due to joint and bone pain. Painful swelling of proximal phalanx of right middle finger was seen (Figure 1). Additionally, there were multiple bony lumps on anterior aspect of bilateral tibia with induration of overlying skin. Her left elbow was swollen and tender with reduced range of movements. But, no significant swelling or tenderness was noticed at other joints. Even though right middle finger was shorten, typical deformities of rheumatoid arthritis was no found in hands.
The examination of cardiovascular, respiratory, neurological systems, abdomen and thyroid was within normal limits.
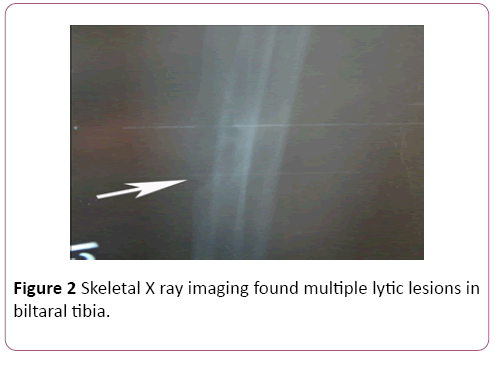
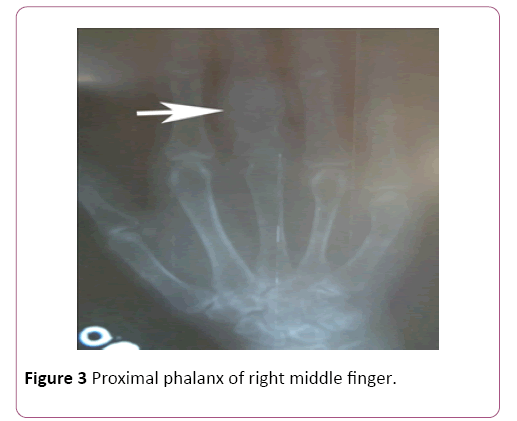
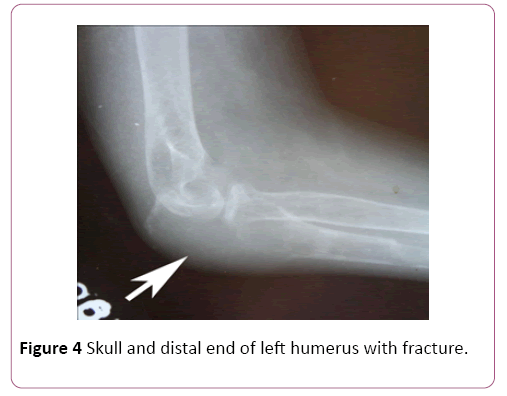
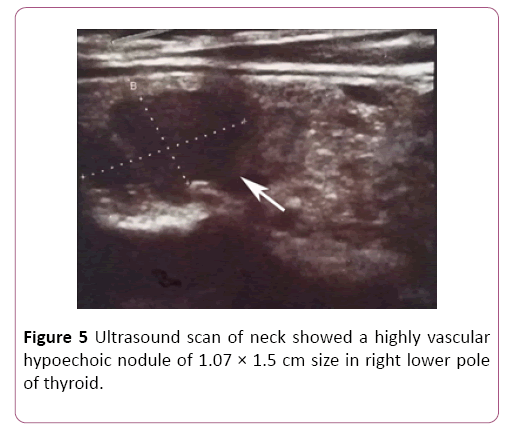
Basic investigations done at index admission including full blood count, urine full report, renal function tests, serum electrolytes, sedimentation rate, C-reactive protein, lactate dehygrogenase levels were normal. However her corrected serum calcium level was markedly elevated to 3.47 mmol/l. Other investigation results were as follows; Serum phosphate 0.76 mmol/l (1.12-1.45), and alkaline phosphatase 1045 U/l, Serum parathyroid hormone level 1461 pg/ml (6-80). Skeletal X ray imaging found multiple lytic lesions in biltaral tibia (Figure 2), proximal phalanx of right middle finger (Figure 3), skull and distal end of left humerus with fracture (Figure 4), but failed to identify condrocalcinosis or subarticular erosions. Bone mineral density assessed by dual energy x-ray absorptiometry revealed severe osteoporosis with T scores of -9.4, -5.2, and -5.1 at distal radius, lumbar spine and femur neck respectively. Ultrasound scan of neck showed a highly vascular hypoechoic nodule of 1.07 × 1.5 cm size in right lower pole of thyroid (Figure 5). Tecnetium thyroid scintigraphy revealed hypofunctioning nodule at right lower pole of thyroid.
Further investigations revealed normal angiotensin converting enzyme level, bone marrow examination, ANA, rheumatoid factor titer, echocardiogram and high resolution computed tomography of chest.
Surgical exploration of neck found enlarged right parathyroid gland, which is histologically confirmed as an adenoma.
Following surgery, her serum calcium normalized with calcium replacement following a brief period of severe hypocalcemia and hypomagnesemia and she noticed a significant improvement of her joint symptoms without use of disease modifying anti-rheumatic drugs (DMARDs) or analgesics.
Discussion
Hyperparathyroidism is known to associate with multiple articular manifestations including gout, pseudogout, juxtaarticular erosison, traumatic tenosynovitis, periarthritis, and pericapsular calcification [6]. A study by Helliwell showed arthritis in 11% including two cases of erosive arthritis in patients with hyperparathyroidism [7]. PHPT presenting as arthritis had been described in few case reports [8-11].
Due to lack of typical clinical features, primary hyperparathyroidism is often undiagnosed or misdiagnosed, especially in resource poor setting. Hence clinicians should have a high degree of suspicion for alterative diagnosis at the beginning and during follow up especially when the initial diagnosis is doubtful.
Our patient had presented with multiple large and small joint arthritis. She did not fulfill American rheumatology criteria 1987 for diagnosis of rheumatoid arthritis. But diagnosis of sero-negative rheumatoid arthritis might have been made clinically. But, the lack of typical joint distribution of rheumatoid arthritis together with insignificant morning stiffness, absence of typical deformities, minimally elevated ESR, negative rheumatoid factor and poor response to DMARDs make the diagnosis of rheumatoid arthritis unlikely.
Furthermore the concurrent development of nephrolithiasis in a young woman might have directed an alert physician towards the diagnosis of PHPT. It highlights the importance of revising the initial diagnosis during the follow up when atypical manifestations developed.
PHPT can occasionally co-exist with inflammatory arthritis like rheumatoid arthritis [12]. Radiographical features are helpful to differentiate both, in addition to clinical and biochemical features. PHPT cuases osteoporosis and pathological fractures. Even though PHPT can cause bone erosion, they are mostly shaggy in appearance and distributed in the radiocarpal, radioulnar, metacarpophalangeal and distal interphalangeal joints, in contrast to predominate proximal interphalangeal joint involvement of rheumatoid arthritis [12]. Our patient had severe osteoporosis and multiple lytic lesions which are typical of PHPT.
Conclusion
PHPT is a rare endocrine disorder. The absence of typical clinical features often delays the diagnosis at early stage in places without routine biochemical screening, till complication occurs. This is further obscured when this rare disease presented with rare manifestations. To avoid misdiagnosis or under diagnosis, and serious unwanted effects of inappropriate medications, clinicians should be alert for an alternative diagnosis by atypical manifestations to the given diagnosis even during the follow up. Detailed history, thorough clinical examination and directed investigation are the tools to achieve this goal. This case illustrates an atypical presentation of primary hyperparathyroidism with polyarthritis, misdiagnosed as rheumatoid arthritis due poor utilization of clinical tools.
Consent
Written informed consent was obtained from the patient for publication of this case report and accompanying images. A copy of the written consent is available for review by the Editor-in-Chief of this journal.
Competing Interest
The authors declare that they have no competing interest.
Authors’ Contribution
DM and SN made the clinical diagnosis and supervised the manuscript drafting. ARB drafted the first manuscript, reviewed the literature and involved in direct management of the patient. DM and SN supervised the manuscript drafting. RMDHMR helps writing and literature survey. All authors read and approved the final manuscript.
Authors’ Information
DM (MBBS, MD, FRCP, FCCP) and SN (MBBS, MD) are Consultant and Resident respiratory physicians at Teaching hospital-Kandy. ARB (MBBS, MD) is a senior registrar in respiratory medicine, RMDHMR is research Assistant, Respiratory Unit 2, at Teaching hospital–Kandy.
References
- MacKenzie-Feder J, Sirrs S, Anderson D, Sharif J, Khan A (2011)Primary hyperparathyroidism: An overview. Int J Endocrinol.
- Khan AA, Hanley DA, Rizzoli R, Bollerslev J, Young JE, et al. (2017) Primary hyperparathyroidism: review and recommendations on evaluation, diagnosis, and management. A Canadian and international consensus. Osteoporos Int 28:1-19.
- Marx SJ (2000)Hyperparathyroid and hypoparathyroid disorders. N Eng J Med 343:1863-1875.
- Pepe J, Cipriani C, Pilotto R, De Lucia F, Castro C, et al. (2011) Sporadic and hereditary primary hyperparathyroidism. J Endocrinol Invest 34:40-44.
- Madkhali T, Alhefdhi A, Chen H, Elfenbein D (2016) Primary hyperparathyroidism. Ulus Cerrahi Derg 32: 58-66.
- Mihai R, Farndon JR (2000) Parathyroid disease and calcium metabolism. Br J Anaesth 85:29-43.
- Helliwell M (1983) Rheumatic symptoms in primary hyperparathyroidism. Postgrad Med J59: 236-240.
- Bywaters EG, Dixon AJ, Scott JT (1963) Joint lesions of hyperparathyroidism. Ann Rheum Dis 22: 171-187.
- Zvaifler NJ, Reefe WE, Black RL (1962) Articular manifestations in primary hyperparathyroidism. Arthritis Rheum 5:237-249
- Lipson RL, Williams LE (1968) The connective tissue disorder of hyperparathyroidism. Arthritis Rhuem 11:198-205
- Duraywish AA (2016) Chronic unclassified polyarthritis: A rare presentation of primary hyperparathyroidism. Med J Cairo Univ 84:265-269.
- Salari M, Aboutorabi RB, Rezaieyazdi Z (2015)Hypercalcemia and lytic bone lesions masquerading inflammatory arthritis. Arch Iran Med 18:720-723.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences