A case report of probable Covid 19 in a patient with known Hereditary Angioedema
Dr Dale Ventour*
Lecturer and Honorary Consultant in Anesthesia and Intensive Care, University of the West Indies, Trinidad, West Indies
*Corresponding Author:
- Dr Dale Ventour
Lecturer and Honorary Consultant in Anesthesia and Intensive Care, University of the West Indies, Trinidad, West Indies
Tel: 1-868-662-4030
E-mail: dale.ventour@sta.uwi.edu
Received date: October 1, 2020; Accepted date: August 21, 2021; Published date: August 31, 2021
Citation: Dr Dale Ventour (2021) A case report of probable Covid 19 in a patient with known Hereditary Angioedema.J Immuno Immnofther 4:1
Abstract
This is a case of stridor exacerbated by Hereditary Angioedema in a 77-year-old patient who had stable, well controlled disease prior to this presentation. His clinical features were highly suggestive of Covid 19 as his symptoms manifested during the Covid 19 pandemic. The author postulated a link between the proinflammatory state of Covid 19 and the inflammatory state of Hereditary Angioedema. His first nasopharyngeal swab was negative but the post mortem swab and his clinical history was strongly suggestive of Covid 19.
Keywords
Hereditary Angioedema, Covid 19, cytokine storm
Summary
This is a Covid-19 case who presented with stridor secondary to an exacerbation of Hereditary Angioedema. The patient had an exaggerated hemodynamic response 7 hours after presentation despite treatment with corticosteroids. A nasopharyngeal RT-PCR test done initially was negative but a post mortem test was positive and the CXR and clinical picture was strongly suggestive of Covid 19.
Introduction
Hereditary Angioedema type 1 is an autosomal dominant condition (estimated 1 in 50,000), as a result of C1 esterase inhibitor deficiency. The permeability seen in this condition is secondary to the effects of Kallikrein and bradykinin activating B2 receptors with dissolution of adherents making vascular permeability possible [1].
This patient was diagnosed during puberty and has a daughter affected albeit with mild symptoms, a grandson with more severe symptoms and it seems as if there was variable penetrance within this family. He had stable disease with approximately 1 attack per year varying from moderate abdominal pains to laryngeal edema. He was maintained with glucocorticoids and administered antihistamines and epinephrine with exacerbations. Even though this is not an effective management of Hereditary Angioedema the patient’s symptoms would abate and he was usually discharged after 12-24 hours, suggesting a histaminergic origin to his condition. His exacerbations were usually stress related but not on this occasion.
Case
The patient was a seventy-seven (77) year old, known to have Hereditary Angioedema and hypertension. He presented with stridor which started 4 hours prior to presentation. He usually had 1 attack every 2 years associated with stress or fatigue and attends his local A & E where he received steroids, epinephrine if there is stridor, anti-histamines and is usually discharged home. These therapies while not conventional or effective were used multiple times in the past with good effect in this patient. On this occasion, he was in respiratory distress with Saturations of 75% on a 15L non-rebreathe mask. His blood pressure was 75mmHg systolic, pulse 114 beats per minute after receiving two (2) lots of epinephrine 0·5 mg Intramuscularly. Oral intubation was attempted which was very difficult as there was marked laryngeal edema and a Grade 4 Cormack & Lehane view. Intubation was successful on the second attempt with capnography and auscultation. The anesthetist was wearing a N95 mask, gown and gloves, no visor was available.He was transferred to the Critical Care for invasive monitoring, stabilization and possible extubating in 72 hours with a diagnosis of Stridor secondary to Angioedema.
There was no recent travel contact and he was residing with his daughter and grandson. At this time in Trinidad we were starting to manage “local” or limited community spread of Covid-19. The other members of the household reported no respiratory symptoms but the patient was making short trips to the local stores and supermarkets.
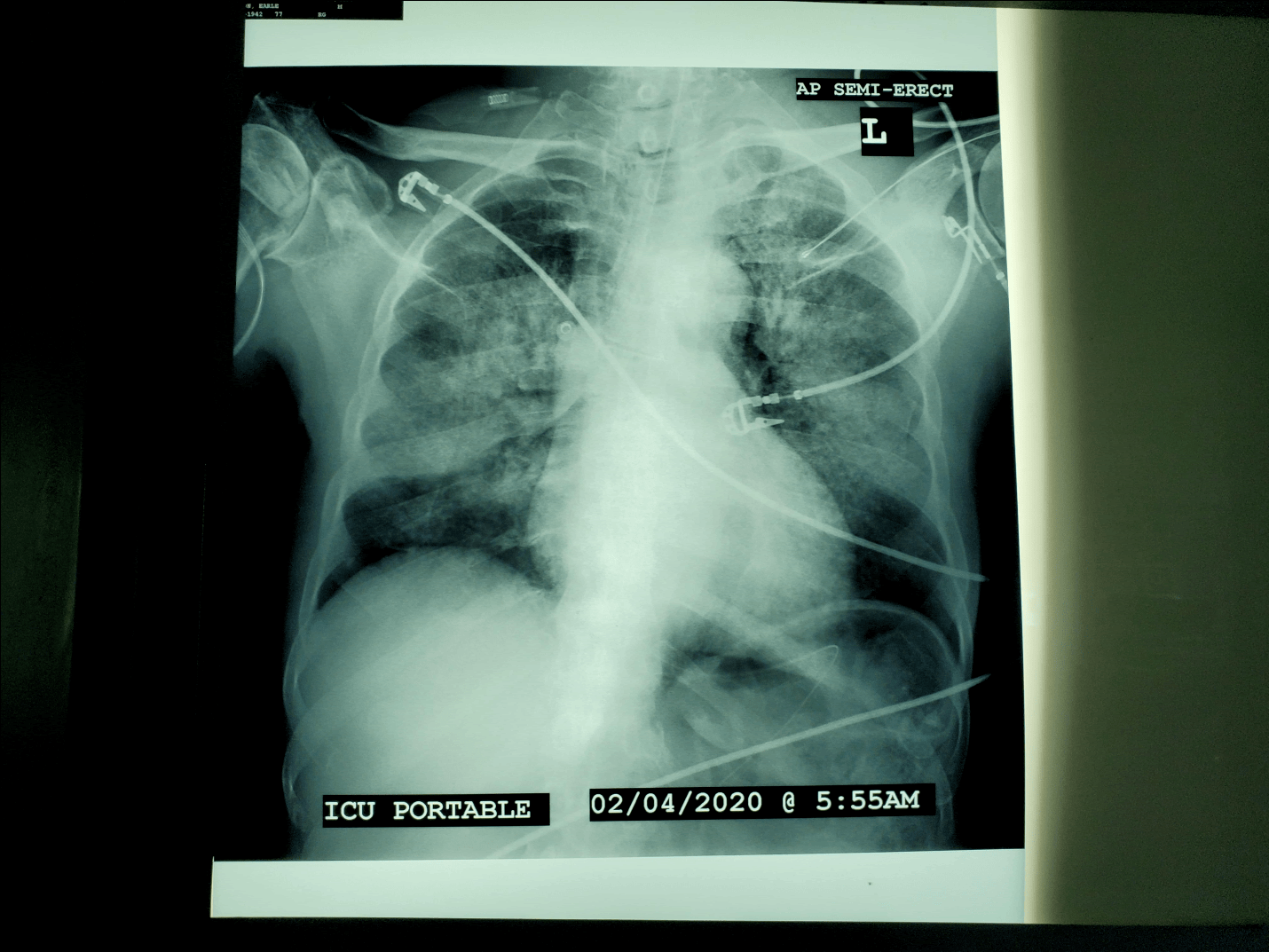
An arterial line, catheter, naso-gastric tube and peripheral cannulas were inserted at this time. He remained on SIMV/ Volume control ventilation with tidal volumes 400 ml, FIO2 0·4, peep 5cmH20, achieving PaO2 100mmHg.He required a metaraminol infusion to maintain Mean arterial pressures > 60mmHg.He was treated with Tranexamic acid one (1) gram TDS, Dexamethasone 8mg BD and given 4 units FFP, Oseltamivir 75mg BD, azithromycin 500mg OD. Results: HIV antibody ELISA negative Influenza A & B negative NT-pro BNP 150 pg./ml Troponin I 0·022 ng/ml (0-0·08) Creatinine 2·02 mg/dl (0·7-1·5) Urea 74mg/dl (16-43) PT 25 sec (28-35) WBC 3·9 Lymphocyte 0·76 (0·9-1·2) After 4 hours, a chest X-ray was ordered and is showed below (Figure 1). He proceeded to deteriorate necessitating a central line for norepinephrine and increases in his FiO2 0.8 to achieve PaO2 of 55mmHG. He continued to be hypotensive, spiked a temperature but remained hypotensive despite both epinephrine and norepinephrine infusions.His echo revealed global hyperkinesia and an underfilled right ventricle but was unresponsive to fluid boluses. He unfortunately had a cardiac arrest 1 hour later and was unsuccessfully resuscitated. His initialnasopharyngeal swabfor Covid-19 via RT-PCR was negative. Under the circumstances, the patient had an expedited burial according to the national Covid burial policy.
Discussion
This case shows an elderly, hypertensive patient with stable Hereditary Angioedema who rapidly deteriorated with Covid 19. In a case series by Ai T et al. [2] the sensitivity of CT scan is greater than 95% with a false negative rate of RT-PCR of 38%. The sensitivity of CXR and clinical history has not been compared to RT-PCR for Covid but this patient exhibited such a massive cytokine storm with a normal echocardiogram and Troponin. Negative pressure pulmonary edema is a differential but the patient’s FIO2 did not improve with positive end expiratory pressure but progressively worsened. I did not find any case of Hereditary Angioedema progressing rapidly to an ARDS picture with inotropic resistant shock.
If an initial Bronchoalveolar Lavage was taken after intubation would that have resulted in a positive RT-PCR?Case reports such as Cheun et al, 2020 have found that patients with strong clinical suspicion and two negative swabs when intubated was diagnosed by a BAL. This was supported by Hauge et al who also diagnosed a patient from BAL after testing negative from a nasopharyngeal swab, the swab was taken within 3 days of illness but the patient had already stopped ‘shedding’ in her upper respiratory tract.
The differentials for this patient were: Negative pressure pulmonary edema, Atypical pneumonia, Non-Covid viral pneumonia, Heart failure with preserved ejection fraction and ARDS secondary to Hereditary Angioedema.
The patient had a normal white blood cell count, was afebrile which made the likelihood of a bacterial infection very unlikely. A viral infection cannot be entirely ruled out as his swabs for influenza was negative (a full respiratory panel was not done). The continued deterioration despite positive end expiratory pressure, worsening hemodynamic instability with escalating inotropes over 4 hours and the normal NT-pro BNP all make the differentials less likely. The patient only received one 4mg dose of Dexamethasone for the marked laryngeal edema yet still continued to deteriorate despite maximal organ support. Hereditary Angioedema is a pro-inflammatory state as a result of C1 esterase inhibitor deficiency, with high levels of bradykinin which account for most of the clinical effects of the condition. It is proposed that the inflammatory state caused by Covid was the precipitant in this case which triggered this massive cascade in this patient and led to his unfortunate demise. There need to be a high index of suspicion in patients presenting with proinflammatory conditions and whether we should be pulsing with high dose steroids in the first instance to ameliorate the overall inflammatory process.
The Dexamethasone was continued to aid with the laryngeal edema and there was some evidence at this time (Early march) that steroids may help in critically unwell patients with Covid 19. It is also worth noting that C1 INH concentrate (icatibant) is not available in Trinidad but the use of this inhibitor in Covid 19 patients is unknown.
There is no conflict of interest by the author Dr Ventour
References
- Kaplan AP, Joseph K (2017) Pathogenesis of hereditary angioedema: the role of the bradykinin-forming cascade. Immunol Allergy Clin North Am 37:513-525.
- Ai T (2020) Correlation of Chest CT and RT-PCR Testing in Corona virus Disease 2019 (COVID-19) in China: A Report of 1014 Cases Radiology.
- Correlation of Chest CT and RT-PCR Testing in Corona virus Disease 2019 (COVID-19) in China: A Report of 1014 Cases
- V Chuen, H Said, J Shell et al. (2020) Diagnosis of COVID-19 by Bronchoalveolar Lavage after Two Negative Nasopharyngeal Swabs Canadian Journal of general internal medicine.
- MT Hauge, E Nilsen, T Nordseth et al. (2020) Acute respiratory distress syndrome in a patient with COVID-19 and negative nasopharyngeal swabs - Tidsskrift for Den norske tidsskriftet.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences