Abstract
A 77-Year-Old Man with Heparin-Induced in the Aldosterone Suppression Causing Hyperkalemia
Anticoagulation with heparin infrequently causes elevated serum potassium via a reduction in the number and affinity of adrenal angiotensin II receptors, causing reversible aldosterone suppression, thereby leading to enhanced sodium excretion and hyperkalemia. Case Report: A 77 year-old man presented with productive cough and shortness of breath and was subsequently found to have non-ST-elevation myocardial infarction and concomitant symptomatic COVID-19 infection, for which he was started on a high-dose unfractionated heparin infusion. A gradual increase in serum potassium followed, with a subsequent return to a normal potassium level after stopping treatment with heparin. An evaluation for hemolysis was unrevealing, and the patient was not on any other medications known to cause hyperkalemia. On day 6, heparin was restarted owing to a high suspicion of pulmonary embolism. There was a subsequent increase in serum potassium level, which was followed by a return to baseline after discontinuation of heparin, thereby confirming the suspected diagnosis. Conclusions: Acute increases in serum potassium levels in hospitalized patients can result in weakness, paralysis, conduction abnormalities, and cardiac arrhythmias that, if left untreated, can result in serious morbidity and potentially death in a short period of time. As this clinical entity is infrequently encountered in clinical practice, it can easily be overlooked by clinicians. The prompt exclusion of alternative causes of acutely elevated serum potassium levels and the identification of heparin administration as an easily reversible trigger is imperative and can potentially be life-saving.
Author(s): Jonathan Kovacs
Abstract | Full-Text | PDF
Share This Article
Google Scholar citation report
Citations : 22
International Journal for Case Reports received 22 citations as per Google Scholar report
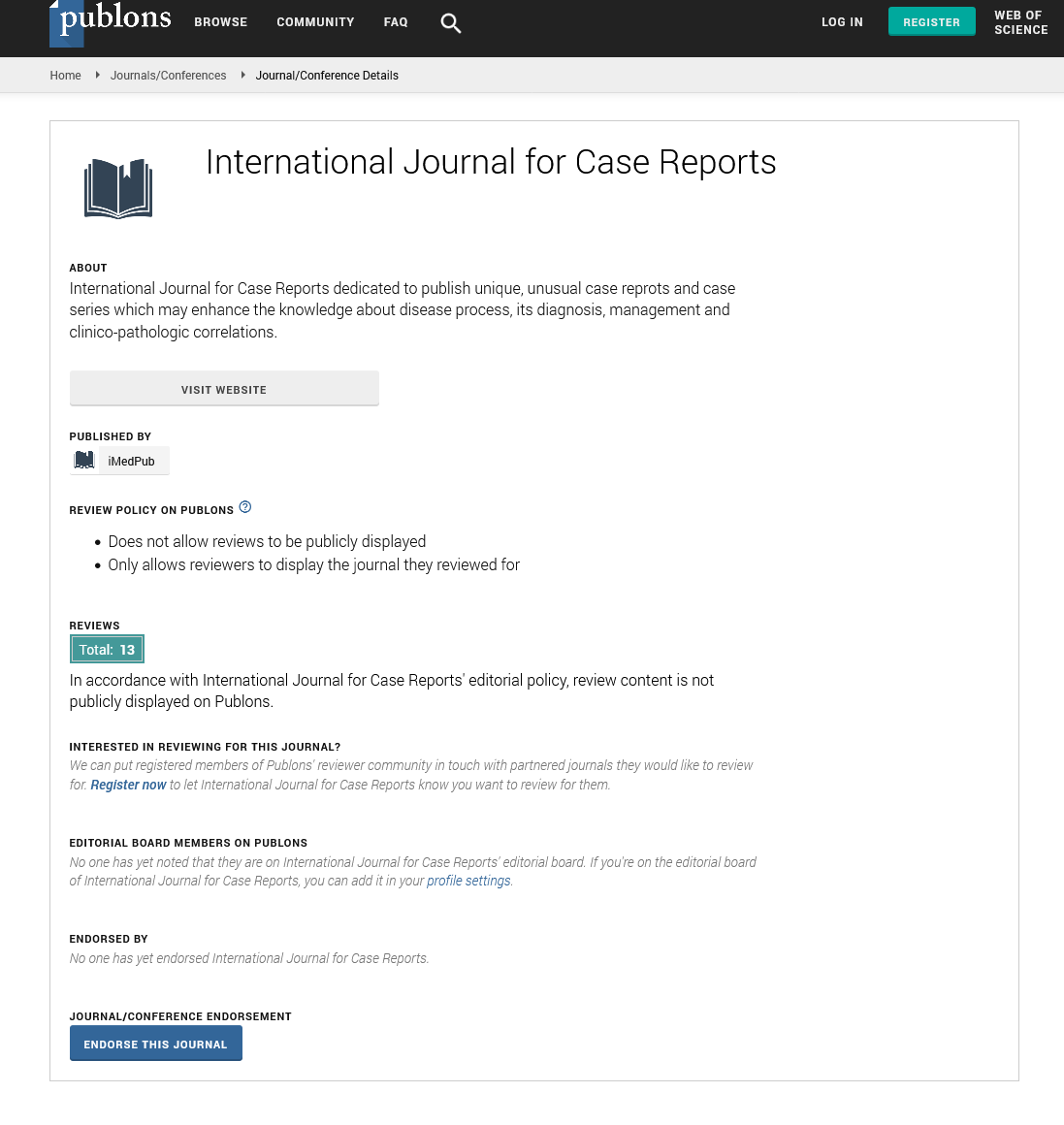
International Journal for Case Reports peer review process verified at publons
Abstracted/Indexed in
- Google Scholar
- Publons
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences