The Role of Neuromodulation Techniques for Management of Back Pain Based on Scientific Evidence
Enrique Latorre Marques*
Department of Anesthesiology, "Miguel Servet" Hospital, School of Medicine, University of Zaragoza, Spain
- Corresponding Author:
- Enrique Latorre Marques
Head of Pain Clinic, Department of Anesthesiology
"Miguel Servet" Hospital, School of Medicine
University of Zaragoza, Spain
Tel: +976 76 53 00
E-mail: elatorrem@salud.aragon.es, elatorremarques@yahoo.es
Received date: April 11, 2018; Accepted date: April 27, 2018; Published date: May 09, 2018
Citation: Marques EL (2018) The Role of Neuromodulation Techniques for Management of Back Pain Based on Scientific Evidence. J Anaesthesiol Crit Care Vol.1 No.2:9
Abstract
Background: Low back pain (LBP) is characterized for its prevalence, great variability, high rates of disability and costs. Chronic Low Back Pain (CLBP) has excessive rate of surgery. Evidence based studies demonstrates only few techniques are cost-effective and many others dangerous. CLBP may originate in dysfunctional nociceptive processing within the central nervous system for that Neuromodulation offers emergent possibilities. Neuromodulation is reversible, adjustable, less invasive avoiding surgery and providing functional recovery. The cost is significantly lower and Quality of life clearly better than conventional pain therapy. The International Association for the study of pain (IASP) and the Special Interest Group on Neuromodulation (SIGN) is the leading forum for science to design therapeutic algorithms for back and neuropathic pain.
Objectives: This Comprehensive Review explains concepts, epidemiology, cost, indications and types of Neuromodulation on management of LBP and radiating pain.
Methods: A comprehensive review of literature: Clinical Guidelines, IASP sources, SIGN policies, focused on chronic low back pain (CLBP) and Failed Back Surgery Syndrome (FBSS). Also we include one big Meta-Analysis where were reviewed all Clinical Practice Guidelines (CPG), 871 Systematic Reviews, Randomized control trials (RCT´) and Prevention studies for COST B13 Program, literature reviews Searching in the Cochrane Library, Medline, Embase and other electronic databases.
Results: Neuromodulation offers good and promising results in patients with CLBP and radiated intractable pain. RCTs demonstrated the efficacy without important side effects. Technological advances and clinical evidences continue to expand new modalities. IASP SIGN coordinate efforts including therapeutic algorithms based on scientific evidence.
Conclusion: Neuromodulation is a safe, minimally invasive and reversible technique to relieve back and radiated pain when conservative management has failed, avoiding surgery and opioids. It is included in CLBP algorithms of management adopted by National Health Systems of European Union from 2005.
Keywords
Neuromodulation; Chronic low back pain; Failed back surgery syndrome; Neuropathic pain
Introduction
Low back pain (LBP) is one of the most prevalent disease for clinical management because multiple factors. There is great variability in its management, especially in developed countries, which excessive indication of surgery increases the risk of iatrogenic and healthcare cost. LBP is a leading health and socioeconomic problem. Also the trend of rising Chronic Low Back Pain (CLBP) prevalence is associated with high rates of disability. Neurostimulation devices developed in the 60s of past century, was implanted at the first time for treatment of pain in the failed back surgery syndrome (FBSS) and complex regional pain syndromes (CRPS) in USA. Neuromodulation can be an effective therapy for patients suffering back and radiated pain which there is no other alternative therapy having several advantages compared with re-operation: 1) NE provides a screening trial can predict the outcome of NE, while no such trial is available to predict the outcome of re-operation; 2) It is designed to be reversible and adjustable, whereas the effects of re-operation are permanent; and 3) It is less invasive than reoperation. Despite these attributes, is often reserved for patients who have failed multiple, and indeed all possible, re-operations a strategy that might reduce a patient’s chance of successful treatment with Neurostimulation. But original indications are expanded to management of back and radiating pain, avoiding surgery and strong opioids abuse.
The Management of Low Back Pain Based on Scientific Evidence
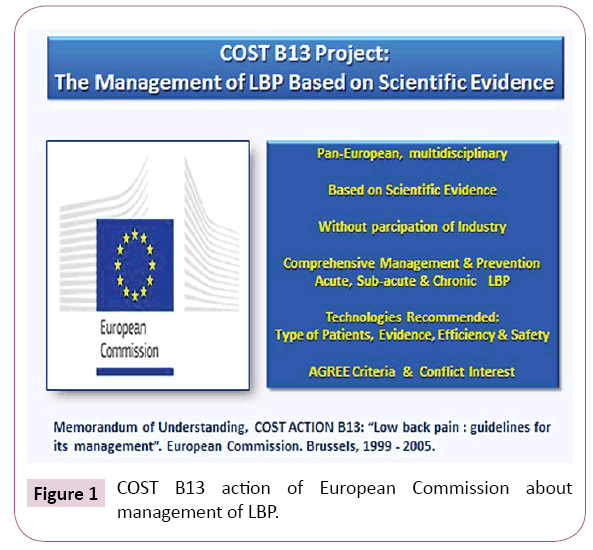
In 2001 The European Union (EU) made efforts to minimize the health cost about LBP by two paths: The Eurobarometer Survey and The COST B13 project.
The “Eurobarometer”
It is a part of European Commission Health Strategy analyzing health aspects of European citizens. Muscleskeletal problems affects 22% of population, 32% had pain on the week prior to the survey. In Europe LBP is the most common type affecting 67 million. The 44% of 55 age group have restrictive pain. In Europe LBP affects more frequently Industrial workers, agriculture, fisheries, and construction people. The 20% of adults has low back pain, it is the second location more frequent of pain. Only 10% of acute cases origin should be identified, chronic pain lasts more than 3 months and affects 10% of cases. LBP is the most frequent cause of consultation and disability of industrial workers under 45. 25-40% of patients with medical care have radiated pain but 2% have acceptable results for the nerve root decompression surgery. Only 20% of patients with signs of disk herniation will recover the normal physical activity. However in 58% of cases, early primary care achieves good improvements of pain, disability and begin again to work. At least 75% of patients present one relapse of year [1].
Cost of Low Back Pain
LBP generates very high cost, in fact around 5% of patients with disability generates 75% of healthcare costs.
There are important geographic variations in terms of length and chronicity. 90% of crisis are resolved in 6 weeks but 10% of patients develop chronic pain and frequent exacerbation. On the other hand there are limited consensus regarding the appropriate use on diagnostic and treatment, excessive variation for indication of surgery which in USA is 500% than Europe. Finally, few technologies have been effective, based on scientific evidence with Randomized Control Trials (RCTs) [2].
Deyo et al. published one interesting research which examines all aspects about impact in health, economic and social system of LBP in National Health Systems of developed countries which is entering in crisis [3].
Medicare spending for in-patient back surgery increase 200% only in one decade, lumbar fusion is 47% of total spending for back surgery. Similarly, increase in spinal cord implants has been reported. Management of FBSS including interventional techniques results in acceptable improvement and relieves intractable pain [4].
From 1990 costs have been increasing, medical treatment between 9000 and 19000 $ patient/year and surgery around 19000 to 35,000 $ [5]. Developed countries have increased interventionist techniques 235% in parallel to progress new injection techniques guided by X-ray, Echography or Magnetic Resonance including Neuro-navigation. Cost of intervencion in patient with pain from spinal origin continues increasing but also complications like FBSS [6].
The European Multinational Cost B13 Program
In order to reduce the variability in the management of LBP European Union designed the first program in the world based on scientific evidence. The European Commission Directorate of General Research Political Co-Ordination and Strategy branch developed under the title “Low Back Pain: Guidelines for its management” since 1999 to 2005 one big Meta-Analysis where were reviewed all Clinical Practice Guidelines (CPG) and 871 Systematic Reviews, Randomized control trials (RCT´) and Prevention studies involving a total of 49 experts [7].
COST B13 clinical guideline
COST B13 Guide includes recommendations for management Acute, Chronic and prevention of LBP which it is the difference with previous guides. American Pain Society (APS) published in 2009 one guide recommended limiting the use of Interventional techniques avoiding invasive therapies and showing benefits of non-invasive (stay active, intensive rehabilitation and cognitive/ behavioral emphasis).
In contrast American Society of interventional Pain Physicians published a critical review of Interventional Techniques for chronic and acute LBP that differs from APS Guidelines including epidural injections, nerve blocks, radiofrequency, and percutaneous adhesiolysis as appropriate methodology. In addition, European Guide COST B13 included interventional techniques such as Neuromodulation and Blockades but limiting use in radiating and intractable pain with other measures. Probably future RCTs obtain a balance between non-invasive and Interventional therapies [8].
The COST B13 Guide is pan-European, multidisciplinary, based on scientific evidence, funded without participation of the industry or profit institutions. It provides comprehensive management of acute, chronic low back pain and its prevention. In the Spanish version, recommendations related to acute and chronic low back pain were integrated to improve clinical practice and applying different techniques depending on type of patients, scientific evidence, effectiveness, and safety. Also we added a conflict of interest declaration by its members, and applying instrument AGREE. It is included in the national health systems of European Community from primary to hospital care.
Search strategy & development
The systematic reviews were identified using the results of validated search strategies in the Cochrane Library, Medline, Embase and, if relevant, other electronic databases, performed for Clinical Evidence. A three-stage development process was undertaken. First, recommendations from systematic reviews. Secondly, existing national guidelines were compared and recommendations summarized. Thirdly, the recommendations were discussed by the multinational group of experts. A section was added to the guidelines in which the main points of debate are described. The recommendations are set in a clinical relevant order.
A grading system was used for the strength of the evidence and levels of evidence recommended in the method guidelines of the Cochrane Back Review group. Several systematic reviews have included non-English language literature (publications in French, German, Spanish, Dutch and sometimes also Danish, Norwegian, Finnish and Swedish). The Working Group aimed to identify gaps in the literature and included recommendations for future research (Figure 1) [9].
Figure 1: COST B13 action of European Commission about management of LBP.
Epidemiology
The origin of LBP is by frequency: Common low back pain 90%, symptomatic herniated disk 4%, ankylosis (0.3 - 5%), compression fractures 4%, and spinal malignancy 0.7%. Pain can occur in different ways: Episodes acute last less than 3 months in more than 90% of the cases, which are usually benign, and they can be treated with simple steps, usually this corresponds to the type "Non-specific”" but the rest of the cases may be due to other causes and therefore must diagnose and treat "specifically" and quickly. Chronic pain lasts more than 3 months and constitutes about 10% of cases, but generates higher costs [10].
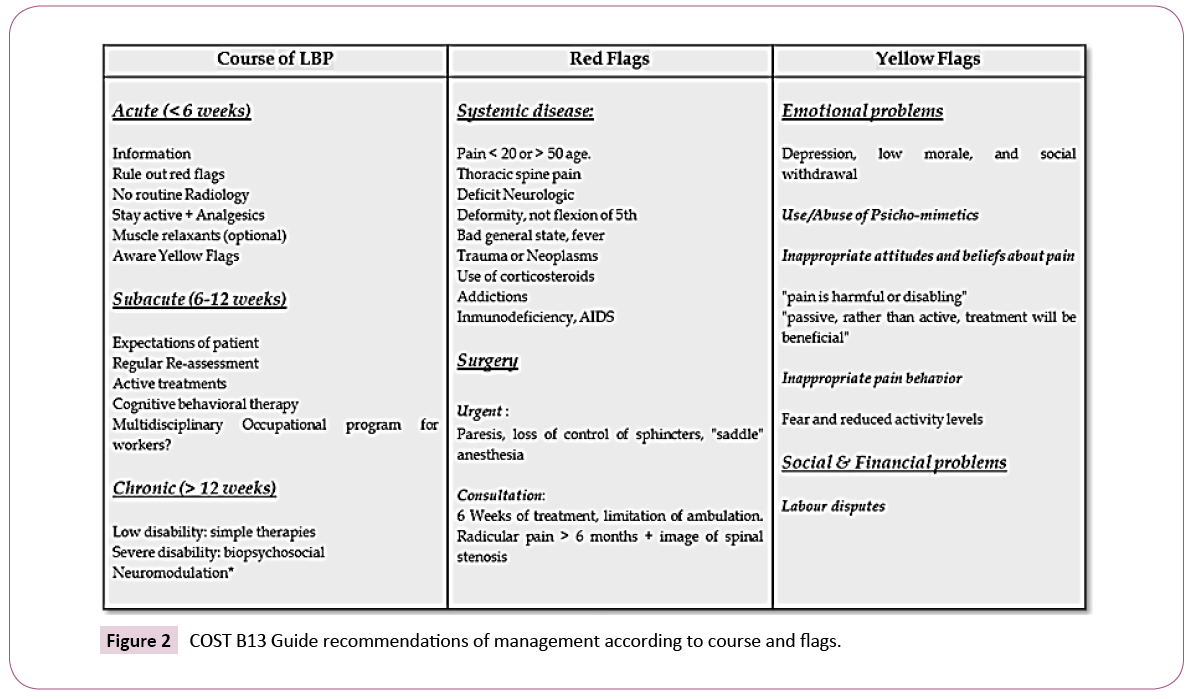
Prevention & management
The key to preventing the acute pain onset and chronicity is integrating preventive measures into clinical course; diagnostic, therapeutic and preventive actions so optimize long term results. Generally pain yields around 6 weeks, as a novelty we introduced the term “sub-acute” for episodes reach between 6 and 12 weeks and are warning signs called “Yellow flags” needing new evaluations and treatments (Figure 2) [11].
Figure 2: COST B13 Guide recommendations of management according to course and flags.
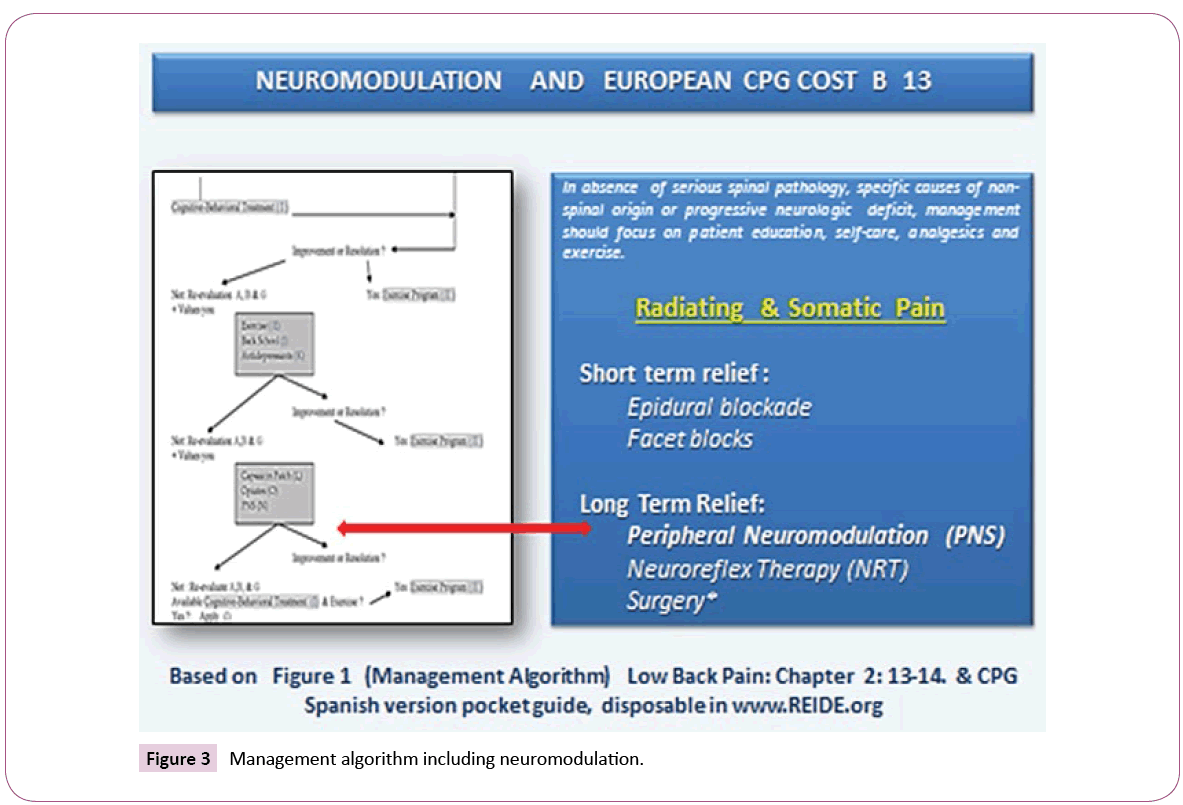
Our Guide recommended patient education, self-care, analgesics and exercise only in absence of serious spinal pathology, specific non-spinal ethiology or progressive neurologic deficit. Short term relief in radiating pain may be obtained with epidural blockade with local anesthetics and steroids, or facet blocks in selected cases.
Neuromodulation
COST B13 Guide was the first included use of Neuromodulation in management of LBP. According to Scientific Evidence, Neuromodulation Techniques including Peripheral Neuromodulation (PeNS) and Neuroreflex-therapy (NRT) can offer good results in LBP avoiding surgery and providing functional recovery (Figure 3) [12].
Figure 3: Management algorithm including neuromodulation.
LBP & the IASP SIG on Neuromodulation
The International Association for the study of pain (IASP) is the leading professional scientific forum for investigation, practice and education on pain, having around 7,000 members, in 133 countries, 90 national chapters and 20 Special Interest Groups (SIGs). It brings together scientists, clinicians, health-care providers and policymakers to stimulate and support the study of pain and translate that knowledge into improved pain relief worldwide.
The purpose and mission of the Special Interest Group on Neuromodulation (SIGN) is:
1. Promote interdisciplinary collaboration among scientists, clinicians and other professionals within the health-care networks world-wide in research and clinical application of neuromodulatory treatment strategies.
2. Facilitate inter-professional education and training in the field of neuromodulation with particular attention to the clinical application of emergent neuromodulatory techniques for pain and symptom management.
3. Stablish a platform and forum for address emerging issues and development of evidence-based practices and policies [13].
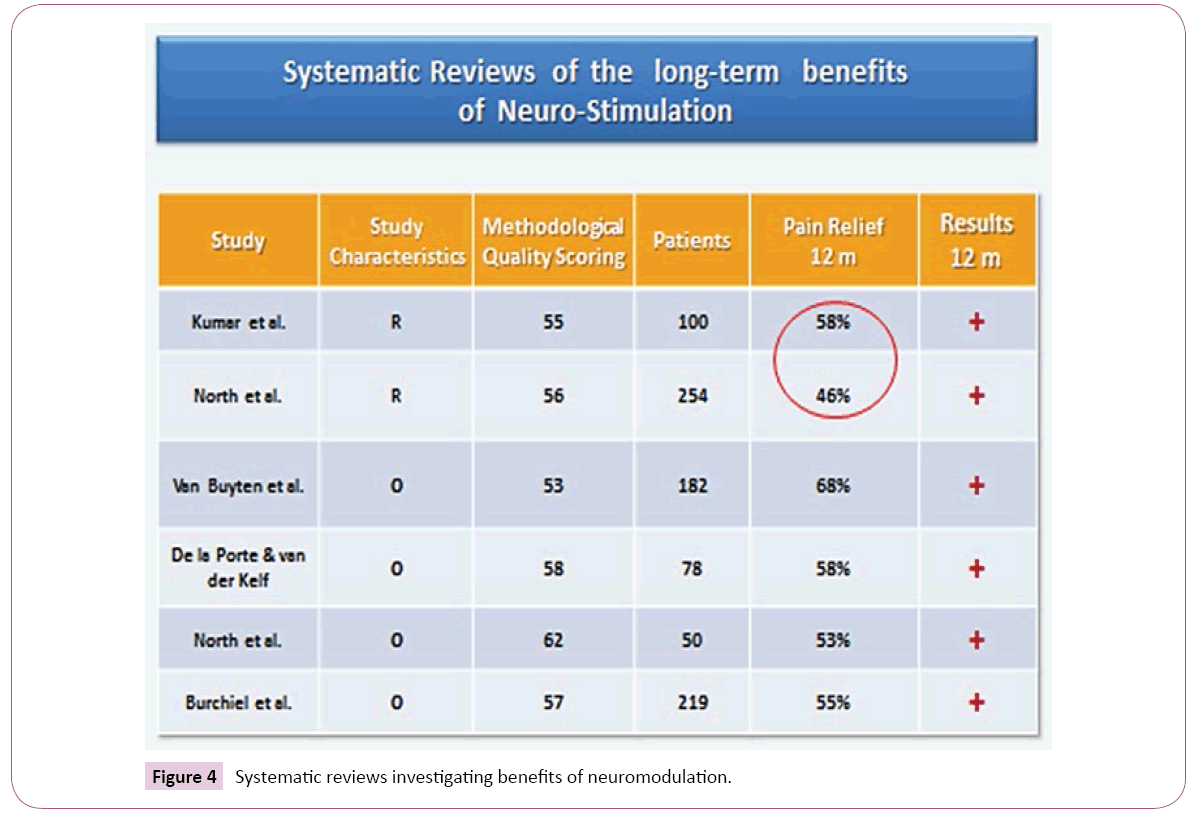
In this way, our SIG has been promoted Cost-Effective researches and clinical application of neuromodulatory treatment strategies in LBP. In fact Cost-effectivity was evaluated in 2 systematic reviews and 3 studies with positive results. Really Neurostimulation in patients with neuropathic leg and back pain generates important improvements on functional and health status (Figure 4) [14].
On one hand, SIG on Neuromodulation promote investigations about new modalities of Neurostimulation integrating studies, cost-effectivity and scientific evidence. On the other hand developing multinational working groups, evidence-based studies and health policies.
Neuromodulation Techniques for LBP
Rational use of Neuromodulation techniques in CLBP (including radiating) are being studied because recent developments about new modalities of stimulation like high frequency in SCS or recent discoveries. The most interesting are described below.
Spinal cord stimulation (SCS)
SCS is a safe, reversible and minimally invasive procedure, not associated with medication-patient side effects but device complications are not uncommon, however is becoming less frequent because new modalities and technological developments. SCS is effective in radiating, neuropathic, and CPRS pain.
Before the first 2 years SCS implantation cost was higher than conventional pain therapy however after this period it is significantly lower. Also quality of life results showed 27% improvement compared with 12% for the conventional pain therapy. Neurostimulation would be more cost-effective in terms of patient satisfaction and return to work [15].
Peripheral stimulation
• Peripheral nerve stimulation (PENS): Particulary our SIG make attention to the clinical application of emergent neuromodulatory techniques for pain and symptom management. Peripheral Neurostimulation (PENs) should not be confused with transcutaneous nerve stimulation (TENS) applied over the same area. EN creates a local electrical field wich is narrower and produces a higher current density. The recommended stimulation algorithm of care is as follows: Stage I: external neuromodulation → Stage II: needle neuromodulation → Stage III: temporary catheter trial → Stage IV: permanent neuromodulating implant. Dr Goroszeniuk (2000) introduced a stimulating monoelectrode percutaneously near the nerve in neuropathic pain syndrome patients, using 2 Hz stimulation obtained 11 weeks of complete pain relief. This experience is a simplified version of the therapeutic and diagnostic neurostimulation test using a single stimulating needle over nerves and plexuses. The pattern of stimulation with low frequencies (2–10 Hz) and wide pulse adjusting amplitudes of stimulation to below those that produce motor stimulation, usually between 2 and 20 volts, has clinical efficacy in many pain disorders including back pain, coccycodynia and CRPS [16]. Paicius (2007) applied NE on patients with chronic back pain who failed conventional therapies. All patients decreased pain intensities, use of medications and increased their activity. These available data are indicative of the effectiveness, simplicity, patient acceptance; use of simple and inexpensive testing leads should allow better selection of patients and will expand its applications [17].
• Peripheral nerve field stimulation (PNfS): PNfS is becoming utilized sometimes as a first, minimally invasive, neurostimulation procedure if the pain is limited to a relatively small and well-defined. The principle of PNfS is that the lead should be placed within or as near as possible to the painful area. Each electrical contact spreads a circumferential electrical field which is about 2 cm in diameter [18]. The number, spacing, and distribution of the electrical contacts should therefore be carefully planned according to the size and shape of the painful area [19]. Larger areas might require several leads placed strategically [20]. It is crucial to carefully map the transition zone between the allodynic and nonallodynic area and place the lead exactly in that zone. This is an effective indication for intractable axial lumbar pain (FBSS or not) and including neuropathic radiated pain [21].
Cluneal nerve stimulation
The superior cluneal nerve is reliably found at the level of the iliac crest, whereas the medial cluneal nerves are cutaneous branches arising from the dorsal rami of S1 through S3 just lateral to the neuroforamen traveling near the posterior superior iliac spine (PSIS) [22]. Between 2007 to 2011, 60 patients underwent a trial of superior cluneal nerve stimulation with or without middle cluneal nerve stimulation and/or spinal cord stimulation for FBSS, 83% of patients had a successful trial and permanent implantation [23].
A pan-European Study of Axial back pain treated with Peripheral Neurostimulation demonstrated a statistically significant reduction in pain measured by a visual analog scale. Its registry of efficacy was used as supporting evidence in the successful application for CE Mark approval of PNfS in the European Union. Courtney recently presented one study about efficacy of superior and middle cluneal nerve stimulation with or without spinal cord stimulation in the treatment of axial pain in patients with FBSS showing a dramatic reduction in pain scores and significantly improved Oswestry Disability Scores. Recent report by Elliot Krames called “triangulation” method using epidural stimulation in combination with PNfS indicated can be more efficacious than either technique used alone.
Dorsal root nerve stimulation (DRGS)
The dorsal root ganglion (DRG) has emerged as a potential target for treating chronic neuropathic pain before morphometric magnetic resonance studies [24]. Dorsal root ganglionectomy for failed Back surgery patients demonstrated improvement of pain scales [25] Lynch publishes one case of successful stimulation [26] and Wrigth for intractable disc pain [27] Stimulation of sensory neurons in the DRG may result in more precise and selective stimulation when the pain distribution is in a region over which paresthesia is difficult to achieve with SCS [28].
Prospective studies in Europe showed mean reductions in lower limb pain of 54.6% and 58.6% at 3 and 6 months respectively, with concurrent improvements in quality of life [29].
Non-invasive Brain Stimulation Techniques
Pain in CPRS and other entities is related with associated with functional reorganization and hyperexitability of the somatosensory and motor cortex. Non-invasive brain stimulation techniques such as transcranial magnetic stimulation (TMS) and transcranial direct current stimulation (tDCS) modulate the cortical excitability and starts the reversal of cortical reorganization in patients with spontaneous or provoked pain providing new strategies to relieve pain. Repetitive sessions of tDCS have analgesic effects overtaking the period of stimulation and are cumulative, transient and site-specific [29].
Patients with neuropathic pain showed significant increase in cerebral blood flow in the ventral-lateral thalamus, medial thalamus, anterior cingulate/orbitofrontal cortex, anterior insula and upper brainstem in PET scans after motor cortex stimulation. All of these areas are known to be involved in various mechanisms of transmission of pain. The activation of the contralateral motor cortex may trigger directly thalamic activity via cortico-thalamic projections, modulating the spinothalamic tract which is the predominant ascending pain-signaling pathway [30,31].
Safety of tDCS has been evaluated in animal and human studies involving healthy volunteers, and patients with complex regional pain syndrome (CRPS) [32]. For that non-invasive brain stimulation techniques could be an alternative to alleviate allodynia and hyperalgesia in radiating pain from spine origin [33].
New Experiences in LBP Modulation
Facet joint neuromodulation
The facet joint can be modulated to improve pain disorders in the spine with some modalities of pulsed radiofrequency used to stimulate different levels of intensity and frequency. Chang designed one study to alleviate the refractory chronic facet joint pain which can be useful for other spine levels. In the same way than Gorostzeniuk´s experience stimulating monoelectrode percutaneously near the nerve in order to predict final implanctation of multielectrode [34].
The medial branch stimulation & multifidus stimulation
Electrical stimulation to elicit episodic lumbar multifidus contraction is a new treatment option for CLBP. Results demonstrate clinically important, statistically significant, and lasting improvement in pain, disability, and QoL.
The recommendations for the Neuromodulation Appropriateness Consensus Committee (NACC) found insufficient, low-quality, or contradictory evidence for SCS use including high frequency (SCS) in patients with predominant low back pain. The multifidus stimulation could be a good choice in selected patients.
There is a clinical need for treatment options for patients with CLBP who have failed existing conventional pain management therapies. Following a single episode of debilitating back pain, lumbar multifidus function is often disrupted at the segmental level due to arthrogenic muscle inhibition leading to a chronic pain state. The results of this feasibility study demonstrated significant and clinically important improvements in low back pain, disability, and QoL at 90-days post activation [35].
Wireless neuromodulation
The minimally invasive approach using wireless electrodes with percutaneous placement over different targets provide good results and will be expand the number of indications for the treatment of chronic pain indications. In the case of CLBP and radiated pain percutaneous electrodes placement avoid implanted pulse generator and long connection. This system is advantageous in front of classic technique, more confortable to patient and surgeon, reducing cost, adverse events and time of surgery [36]. For example DRG wireless stimulation with high frequency seems to be better stability, mitigating postural influences, provides lower energy consumption and good analgesic effect [37].
Development of IASP Evidence-based Practices and Policies
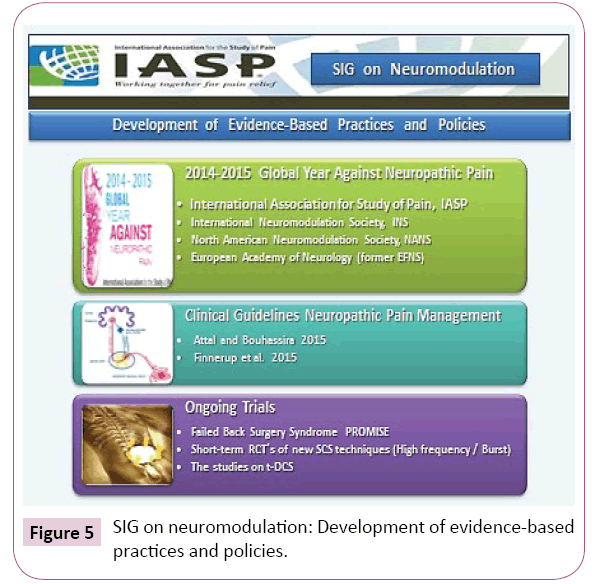
LBP is an entity which includes local and radiated pain can be caused by multiple neural structures. Neuropathic pain is defined as pain that arises as a direct consequence of a lesion or diseases affecting the somatosensory system including lumbar radiculopathy and chronic postsurgical pain. IASP announced the period 2014-2015 as Global Year against neuropathic pain. Which consequences of this announcement are implicated by our SIG? The first is seeking input to other Groups like IASP Neuropathic SIG, International Neuromodulation Society (INS) and European Academy of Neurology (EAN) to define and design strategies and working groups to develop policies about management of back and radiating pain (Figure 5). The second was promoting long term studies about efficacy and costs comparing Neuromodulation versus Surgery. Recent guidelines were published according to the Grading of Recommendations Assessment, Development and Evaluation (GRADE) system. Nevertheless these recommendations, it is still well known that many patients with neuropathic pain are not adequately treated. On the other hand neuromodulation techniques can be very helpful especially in neuropathic pain syndromes.
Also ongoing trials for Neurostimulation in Failed Back Surgery Syndrome (eg. PROMISE), the Multicenter Study by Rigoard and colleagues and short-term RCT´s of new technique (High frequency and Burst stimulation) most likely will be considered. R-TMS also is given a weak recommendation for transient pain relief in central and peripheral neuropathic pain. The studies on t-DCS are developing new targets and strategies of treatment focused on chronic pain and emotional implications in LBP patients having promising results.
Conclusion
In summary it is essential to investigate further for an underlying structural etiology and assess whether these painful symptoms indicates a systemic process. An emerging evidence base suggests that CLBP may originate in dysfunctional nociceptive processing within the central nervous system. Misattribution of pain to direct peripheral nerve injury (radiculopathy with associated motor, sensory, and reflex deficits) may lead to poor clinical outcomes. For this reason it seems Neuromodulation offers emergent possibilities related to these findings.
It is essential that new strategies of treatment of LBP and radiating pain are adapted to Scientific Evidence being cost-effective. The goal is not only pain relief than avoiding disability integrating patients to normal life.
In the future Neuromodulation will be an important role in management of diseases. New efforts are made by the International Association for Study of Pain, International Neuromodulation Society, the North American Neuromodulation Society and the European Academy of Neurology (former EFNS) to publish new recommendations with regard to neuromodulation techniques.
In order to get access with neuromodulation techniques into therapeutic algorithms for CLBP and neuropathic pain, members of our SIG are called upon to initiate well designed studies in homogenous patient groups with a control group for invasive and non-invasive stimulation techniques. SIGN can serve as network for all of us to create and perform such studies [38].
References
- https://ec.europa.eu/health/ph_publication/eb_health_en.pdf
- https://www.cost.eu/COST_Actions/bmbs/B13
- Deyo RA, Mirza SK (2006) Trends and variations in the use of spine surgery. Clin Orthop Relat Res 443: 139-146.
- Wenger DR (2007) Spine surgery at a crossroads: does the economic growth threaten professionalism? Spine 32: 2158-2165.
- Manchikanti L (2010) A critical review of the American Pain Society clinical practice guidelines for interventional techniques: part 2. Therapeutic interventions. Pain Physician 13: E215-264.
- Straus BN (2002) Chronic pain of spinal origin: The costs of intervention. Spine 27: 2614-2619.
- Memorandum of Understanding (1999) COST ACTION B13: “Low back pain: guidelines for its management”. European Commission.
- Marques EL (2012) The management of LBP and Scientific Evidence. In Low back pain. In; Noratesh A, In Tech.
- Marques EL, Kovacs F, Urrutia G, Gil del Real MT, Alonso P (2008) The Spanish version of COST B13 Guide: A clinical guideline for back pain based on scientific evidence. Dolor 23: 7-17.
- van Tulder M, Koes B (2006) Chronic low back pain. Am Fam Physician 74: 1577-1579.
- https://www.kovacs.org/descargas/GUIADEPRACTICACLINICALUMBALGIAINESPECIFICA_136paginas.pdf
- www.REIDE.org
- https://www.iasp-pain.org/SIG/Neuromodulation
- North RB, Kumar K, Wallace MS, Henderson JM, Shipley J, et al. (2011) Spinal Cord Stimulation Versus Re-operation in patients With Failed Back Surgery Syndrome: An International Multicenter Randomized Controlled Trial (EVIDENCE Study). Neuromodulation 14: 330-335.
- Frey ME, Manchikanti L, Benyamin RM, Schultz DM, Smith HS, et al. (2009) Spinal cord stimulation in patients with failed back surgery syndrome: A systematic review. Pain Physician 12: 379-397.
- Gorostzeniuk T (2003) Percutaneous insertion of permanent peripheral stimulating electrode in patients with neuropathic pain. 6th INS World Congress, Madrid.
- Paicius RM, Bernstein CA, Lempert-Cohen C (2007) Peripheral field nerve stimulation for the treatment of chronic low back pain : preliminary results of long term follow up: a case series. Neuromodulation 10: 279-290.
- Abejon D, Krames E (2009) Peripheral subcutaneous field stimulation; what is in a moniker? Neuromodulation 12: 1-4.
- Deer T, Pope J, Hayeh S, Narouze S, Patil P, et al. (2014) Neurostimulation for the Treatment of Axial Back Pain: A Review of Mechanisms, Techniques, Outcomes, and Future Advances. Neuromodulation 17: 52-68.
- Barolat G (2009) Peripheral Subcutaneous Stimulation, A Photographic Surgical Atlas. Blurb Edition.
- McRoberts WP, Wolkowitz RM, Meyer DJ, Lipov E, Joshi J, et al. (2013) Peripheral nerve field stimulation for the management of localized chronic intractable pain: Results from a randomized control study. Neuromodulation 16: 565-574.
- Tubbs RS, Levin MR, Loukas M, Potts EA, Cohen-Gadol AA (2010) Anatomy and landmarks for the superior and middle cluneal nerves: application to posterior iliac crest harvest and entrapment syndromes. J Neurosurg Spine 13: 356-359.
- Courtney P (2011) Superior and middle cluneal nerves: an important target for stimulation in the treatment of failed back surgery syndrome (FBSS). INS Meeting, London, 2011.
- Hasegawa T, Mikawa Y, Watanabe R, An HS (1996) Morphometric analysis of the lumbosacral nerve roots and dorsal root ganglia by magnetic resonance imaging. Spine 21: 1005-1009.
- North RB, Kidd DH, Campbell JN, Long DM (1991) Dorsal root ganglionectomy for failed back surgery syndrome: a 5–year follow-up study. J Neurosurg 74: 236-242.
- Lynch PJ, McJunkin T, Eross E, Gooch S, Maloney J (2010) Case report: successful epiradicular peripheral nerve stimulation of the c2 dorsal root ganglion for postherpetic neuralgia. Neuromodulation 14: 58-61.
- Wright RE, Colliton JW (1998) Neurostimulation of the L2 dorsal root ganglion for intractable disc pain: description of a novel technique. IFESS 3rd Annual Conference Proceedings.
- Grigsby E, Deer T, Weiner R, Wilcosky B, Kramer J (2010) Prospective, multicenter clinical trial studying dorsal root ganglion stimulation in the treatment of back pain. North American Neuromodulation Society Annual Meeting Proceedings.
- Huygen FJPM, Baranidharan G, Simpson K, Patel NK, Love-Jones S, et al. (2014) An upper limb neuropathic pain cohort treated with stimulation of dorsal root ganglia (DRG): pooled data from four prospective European studies. Abstract. Las Vegas: 18th Annual Meeting of the North American Neuromodulation Society, December 11–14.
- García-Larrea L, Peyron R, Mertens P, Gregoire MC, Lavenne F, et al. (1999) Electrical stimulation of motor cortex for pain control: a combined PET-scan and electrophysiological study. Pain 83: 259-273.
- Antal A, Brepohl N, Poreisz C, Boros K, Csifcsak G, et al. (2008) Transcranial direct current stimulation over somatosensory cortex decreases experimentally induced acute pain perception. Clin J Pain 24: 56-63.
- Poreisz C, Boros K, Antal A, Paulus W (2007) Safety aspects of transcranial direct current stimulation concerning healthy subjects and patients. Brain Res Bull 72: 208-214.
- Knotkova H, Homel P, Crucian RA (2009) Cathodal tDCS over the somatosensory cortex relived chronic neuropathic pain in a patient with complex regional pain syndrome (CRPS/RSD). J Pain Manag 2: 365-368.
- Knotkova H, Feldman D, Factor A, Sibirceva U, Dvorkin E, et al. (2008) Repetitive transcranial direct current stimulation improves hyperalgesia and allodynia in a CRPS patient. Brain Stimulat 1: 254-255.
- Chang MC (2018) Effect of pulsed radiofrequency treatment on the thoracic medial branch for managing chronic thoracic facet joint pain refractory to medial branch block with local anesthetics. World Neurosurg 111: e644-e648.
- Tyler Perryman L, Larson P, Glaser J (2016) Tissue depth study for a fully implantable, remotely powered and programmable wireless neural stimulator. Int J Nano Stud Technol pp: 1-6.
- Billet B, Wynendaele R, Vanquathem NE (2017) Wireless neuromodulation for Chronic Back Pain: Delivery of high-frequency dorsal root ganglion stimulation by a minimally invasive technique. Case Rep Med p: 4203271.
- https://www.iasp-pain.org/SIG/Neuromodulation
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences