The Management of Sacral Schwannoma at the Level of S2 and Review of Literature
Arrotegui I*
Department of Neurosurgery, Consortium University, General Hospital of Valencia, Spain
- *Corresponding Author:
- Arrotegui I
Department of Neurosurgery
Consortium University General Hospital of Valencia, Spain
Tel: +34962750054
E-mail: athbio@yahoo.es
Received Date: December 19, 2017; Accepted Date: January 11, 2018; Published Date: January 26, 2018
Citation: Arrotegui I (2018) The Management of Sacral Schwannoma at the Level of S2 and Review of Literature. J Nerv Syst Vol.1 No.1:7
Abstract
Schwannomas of the sacrum are extremely rare. We report a 56-year-old patient who only clinically reported difficulty was sciatica. The imaging studies carried out showed a sacral tumor of a posterior location without an erosive character of the bone, which impressed initially as a Schwannoma. The patient underwent a posterior approach with partial resection of the lesion (80%). The histological report of the Department of Pathology was schwannoma. The postoperative evolution is being satisfactory.
Keywords
Spinal schwannoma; Spinal cord tumor; Giant schwannoma; Giant schwannoma of the sacrum
Introduction
Tumors of nerve sheaths are the most frequent spinal tumors, and together with meningiomas they comprise 90% of all intradural extramedullary tumors. Schwannomas are usually solitary, but they can be multiple in neurofibromatosis type II. They occur more frequently in the fourth decade of life, are intradural-extramedullary in 70-75%, extradural in 15% and with both components (hourglass) in another 15%. The intramedullary are rare (1%).
Large sacral schwannomas are extremely rare [1]. Although in these cases the total exeresis is recommended independently of the risk of a neural lesion, only in very few cases is it achieved in the first operation [2,3].
In this type of giant tumor lesion, MRI and in particular the threedimensional, clearly shows the bone region destroyed, as well as allowing safe surgical planning for total resection with sacroiliac reconstruction. In some cases, it is possible to visualize the relationship between the tumor and theiliac arteries [4].
The management of these large sacral tumors is complex due to the difficult access to the lesion, the high degree of local recurrence, the resistance to radiotherapy, the risk of malignant transformation, and its extreme vascularization that causes a significant transoperative blood loss. Therefore, it is recommended to evaluate a preoperative adjunctive therapy such as embolization, to reduce transoperative bleeding. In other types of lesions, the procedure of embolization is of primary value, to achieve the resolution of symptoms and the ossification of benign lesions, such as aneurysmal bone cysts and giant cell tumors.
This work discloses the clinical history and the particularities in the treatment of a patient with a presacral schwannoma.
Case Report
A male patient, 56 years old, of the white race, about 8 months before has gone to a specialized consultation of Neurosurgery began to present difficulty in walking. The appearance of painful lumbosacral discomfort leads the patient to our office. In the exam performed, there were no motor, sensory or sphincteric deficits, but pain to the acupressure in the sacral region. We proceed to the study of the lumbosacral region.
MRI studies show the lesion of the sacrum in its. MRI of the lumbosacral region defines a tumor mass that is located in the sacrum, Lateral view Figure 1. In MRI of the lumbosacral region the relationship of the tumor can be seen in more detail with the neighboring structures, its exact definition in size and intrasacral extension anterior view Figure 2.
Surgical treatment was planned
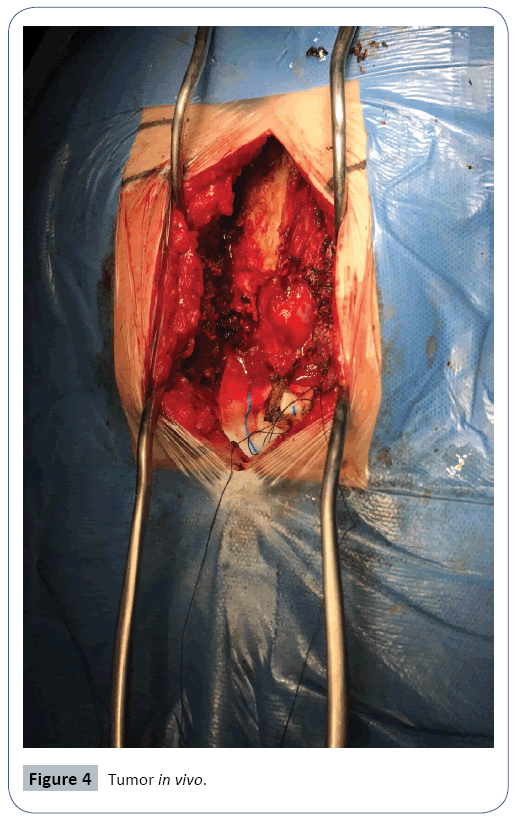
Patient in decubitus prone, incision focused on the sacral region through the help of scopia Figure 3. Separation of the muscular planes with the help of an ultrasound motor with a serrated terminal, a bone window was made for the tumor to be removed, which was subsequently enlarged by the use of laminotomes of different sizes Figure 4. A partial exeresis was performed to safeguard nerve bundles intimately related to the S2 root and which were identified with the help of intraoperative potentials.
Post-operatory days: The evolution of the patient was satisfactory, lumbosacral pain disappeared. Histological diagnosis: Schwannoma.
Discussion
Schwannoma is a benign neoplasm of schwann cell, arising along sensory nerve roots in the extremities and upper thorax. These tumors rarely arise within bone, among which mandible and sacrum are the most common sites of involvement. Only 79 intraosseous schwannomas have been reported in English literature and 21 were located at the sacrum [5]. Most of the cases were treated by curettage and overall results were favorable due to preservation of sacral nerve roots. However, the rate of local recurrence was reported to be relatively high (54 percent) when treated by conservative means. The patients who were treated with sacral amputation had greater chance of having postoperative bowel and bladder dysfunction, in addition to decreased sensation and motor weakness of lower extremities due to sacral nerve roots injury [6].
In 2001, Lirchar [7], Proposes a new term for a particular type of aggressive benign spinal schwannoma, preferably located in the lumbosacral location, the so-called invasive schwannoma, characterized by its high degree of vascularization. On the other hand, Ogose et al. [8] report a benign variant of schwannoma, often confused with a sarcoma and usually solitary.
They report the benefit of performing the immunohistochemical analysis of S-100 and Ki-67 protein to differentiate a cellular schwannoma from a malignant tumor of the peripheral nerve [8,9]. The frequency of occurrence of intraosseous cell schwannoma is 0.2%, between all bone tumors, and the retroperitoneal location in the pelvis is the most predominant [10]. Malignant retroperitoneal schwannomas have been found, sometimes exceptional as reported with ossification of the lesion by Mortele et al. [11] in a patient with Von Recklinghausen's disease.
There is still no consensus in terms of diagnostic modality, need for histological diagnosis before surgery and selection of the best surgical option.
Radiographs of the sacrum are usually abnormal in almost all cases, because the tendency to reach large proportions, these sacral schwannomas cause bone injuries by erosion [12]. Radiological findings are often the diagnostic target, since these tumors of the vain Intraosseous nerves are hidden due to their scant symptoms. In our patient it must be recognized that the imaging studies indicated to the lumbosacral spine were the key to the diagnosis.
CT and MRI can generally determine the nature of the tumor and its relationships with the surrounding anatomical structures. CT clearly defines the sacral bone involved, but poorly the intraspinal extension of the tumor, which is more evident in MRI [13,14].
On CT, these lesions appear as an intraspinal mass or an intraspinal lesion with an extradural and/or paraspinal component. Its density varies from hypodense to hyperdense with respect to the spinal cord. Although the tumor can be seen on CT, the differentiation of the tumor from the medullary tissue is sometimes difficult, which is solved in most cases with a myeloce [15].
Bone erosion if well visualized on CT, which is seen in our case. In our patient, the CT showed a homogeneous, well-defined tumor mass that eroded the sacrum in its anterior cortex and projected into the presacral space.
The MRI shows with greater clarity the rostrocaudal extension in the spinal canal. In general, this imaging study reflects a large mass of presacral soft tissue, well defined, just to one side of the midline with bone involvement. The lesions appear heterogeneous due to the long time of degeneration [16]. The MRI also clearly shows the intrapelvic extension, its relations with the neurovascular structures and its growth in hourglass or halteres in case of growth and extension through the sacral foramen [17]. MRI performed on the patient gave us more details in relation to neighboring structures such as the rectum and bladder, and the actual extension in both the sacrum and intrapelvic.
Some authors consider it necessary to know the histological diagnosis before planning surgery, therefore bearing in mind that it is presacral lesions in contact with the rectum many times, they suggest the biopsy of the lesion through a rectosigmoidoscopy. This procedure has the disadvantage already reported by several authors of inoculating colonic germs at the site of the lesion or in the sacrum itself.
The principle of treatment in these tumors is complete resection with clean sacral margins. The surgical approach can be posterior, anterior or combined depending on the nature and size of the lesion, as well as its situation in relation to the L5-S1 junction. Total resection of the lesion can be difficult and bleeding. The sacral segments may need to be resected both for reasons of surgical approach and to obtain clear, tumor-free limits. Rectal resection is rarely necessary when the lesion is approached abdominally [18].
Authors such as Iwasaki et al. [2] and Nowaki et al. [19] recommend total exeresis despite the risk of a neurological deficit in a first operation. Others, such as Santi et al. support total sacrectomy, but perform an iliac-lumbar fixation [3].
The instrumentation sometimes fails after the resection of large sacral schwannomas, so some surgeons perform bone grafts of the fibula or iliac crest, given its good vascularization, for the reconstruction of the pelvic rim. The tricortical bone graft with vascular pedicle is placed in the dead space of the right and left residual sacrum [20]. However, these techniques are relatively complicated.
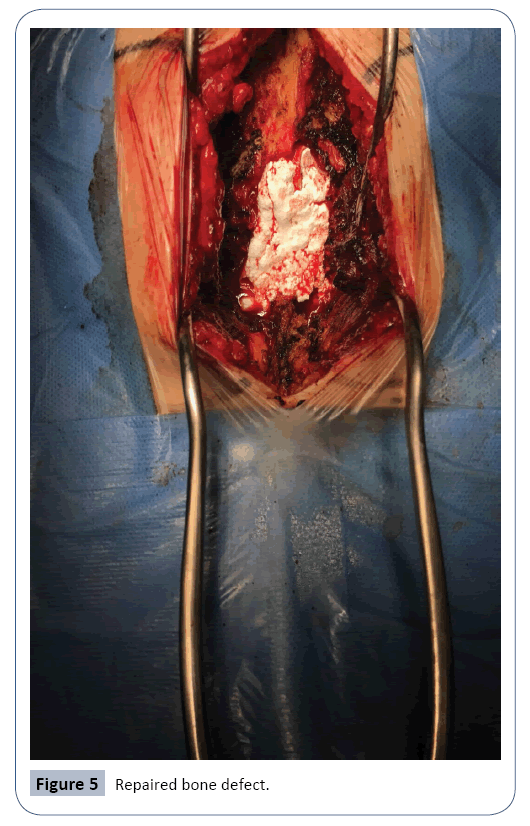
Our patient was not subjected to instrumentation since the surgical procedure of anterior sacrectomy that was performed did not cause instability due to the location of the lesion at the level of S2. The tumor was resected with the help of the monitotization of the sacral roots, the opening of the tumor capsule was performed, performing the emptying of 80% of tumor tissue, avoiding the part of tumor tissue intimately attached to the fibers of the sacral root. Subsequently, a repair of the osseous bone defect was made using the patient's own bone with the help of a spoon adapted to the ultrasound motor (piezosurgery) and nanogel Figure 5.
Resection has been described in 2 surgical stages through the same approach; in other cases in the same surgical time, combined anterior and posterior approaches are performed, with the use of a high speed drill that allows to preserve the sacral roots, after careful dissection [6,14,18,21].
Conclusion
In our opinion, the accumulated experience indicates that it is an approach or another, aggressive resection should be performed to achieve a good result, and therefore surgical planning should be aimed at complete resection, which is curative in most of the cases [5,14,19,22-24]. Independent of the aforementioned, it is also believed that the need for an adequate tumor resection should be assessed considering the preservation of the function of the roots; if there are risks of sacrificing many roots, proceed then to incompletely resect the lesion, since in the case of giant schwannomas the degree of recurrence is low.
References
- Porchet F, Sajadi A, Villemure JG (2003) Spinal tumors: clinical aspects, classification and surgical treatment. Schweiz Rundsch Med Prox 92: 1897-905.
- Iwasaki M, Nakamura K, Takeshita K, Kawaguchi H, Akune T, et al. (1998) Surgical management of giant schwannoma in the lumbosacral region. J Spinal Disord 115:444-447.
- Santi MD, Mitsunaga MM, Luckett JL (1993) Total sacrectomy for a giant sacral schwannoma. A case report. Clin Orthop Relat Res 294:285-289.
- Ortolan EG, Sola CA, Gruenberg MF, Carballo VF (1996) Giant sacral schwannoma. A case report. Spine. 21(4):522-526.
- Salvant JB, Young HF (1994) Giant intrasacral schwannomas: an inusual case of lumbosacral radiculopathy. Surg Neurol 41:411-413.
- Orrickapton HH, Gurcay O (1999) Combined posterior and posterolateral one – stage removal of a giant cervical dumbbell schwannoma. Pediatr Neurosurg 30:102-107.
- Burc G, Kramberger S, Kovacic S, Seruga T, Vorsic M (2004) Recurrent giant invasive thoracolumbar schwannoma. Wien Klin Wochenschr 116:93-96.
- Ogose A, Hotta T, Hatano H, Kawashima H, Unrezu H, et al. (2003) Presacral multiple cellular schwannoma. Spinal 28:426-429.
- Nagonska E, Matyja E, Mossakowski Z, Zabek M (1999) Giant cervico-thoracic schwannoma with long clinical history. Case report. Folia Neuropathol 37:185-188.
- Takeyama M, Koshino T, Nakazawa A, Nitto H, Nakamura J (2001) Giant intrasacral cellular schwannoma treated with high sacral amputation. Spine 26:16-19.
- Mortele K, Lammerling M, Defreyne L, Spelemon F, De Potter C,et al. (1998) Ossified retroperitoneal malignant schwannoma with spinal leptomeningeal metastases. Neuroradiology 40:48-50.
- Turk PS, Peters N, Libbey NP, Warebo HJ (1992) Diagnosis and management of giant intrasacral schwannoma. Cancer 70:2650-2657.
- Yamamichi F, Novomura M, Soeda A, Kamaoka T, Fujikawa K (1999) Retroperitoneal schwannoma. A case report. Hinyokika Kiyo 45:41-43.
- Pollo C, Richard A, De Preux J (2004) Resection of a retroperitoneal schwannoma by a combined approach. Neurochirurgie 50: 53-56.
- Kitamura J, Hida K, Seki T, Iwasaki Y (2002) Giant invasive sacral schwannoma extending to the 4th lumbar spine. No Shinkei Geka 30:1203-1208.
- Tonsgard JH, Kwik S, Short P, Dachman AH (1998) CT imaging in adults with neurofibromatosis 1. Frequent asymptomatic plexiform lesions. Neurology 50:1755-1760.
- Papuri R, Davies AM (2002) MR imaging features of giant presacral schwannomas: a report of four cases. Eur Radiol 12:2365-2369.
- Domínguez J, Lobato RD, Ramos A, Rivas JJ, Gómez PA, et al. Giant intrasacral schwannomas: report of six cases. Acta Neurochir139:954-959.
- Nowaki MP, Czernicki Z. Sacrectomy (1990) at the level of S2 in schwannoma of the sacral region. Case report and review of the literature. Nowotway 40:201-206.
- Oshima Y, Miyoshi K, Mikami Y, Kawamura N (2005) Pelvic ring reconstruction with a vascularized pedicle iliac bone graft for a large sacral schwannoma. J Spinal Disord Tech 18:200-202.
- Turgut M, Ozcan OE, Saglam S (1996) Giant intrasacral schwannomas forming a presacral mass: a report of an unusual cause of lumbosacral radiculopathy. Zantralbl Neurochir 57:201-205.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences