The Introduction of a Clinical Practice Guideline for the Management of Suspected Appendicitis May Influence Computed Tomography Usage
1Surgery and Critical Care, Royal Darwin Hospital, Rocklands Drv, Tiwi, Northern Territory, Australia
2Royal Adelaide Hospital, North Terrace, Adelaide, 5092, Australia
- *Corresponding Author:
- Damien Harris
Surgery and Critical Care
Royal Darwin Hospital, Rocklands Drv
Tiwi, Northern Territory, Australia
Tel: +61 0434 823 143
E-mail: drharris@ozemail.com.au
Received Date: Jan 29, 2018; Accepted Date: Feb 05, 2018; Published Date: Feb 12, 2018
Copyright: © 2018 Harris D, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: A clinical practice guideline for the management of patients with suspected appendicitis was introduced at the Royal Adelaide Hospital. This guideline advises on restricted use of CT scanning for further investigation. The aim of this study was to compare pre and post guideline implementation periods for CT usage rate on such patients. Method: Patients that presented to the Emergency Department and had symptoms and exam findings suspicious for appendicitis were included in the study. Such patients were identified from hospital and emergency department databases and in the post guideline implementation period were also identified prospectively if they were referred to the on-call surgical registrar. Results: Two hundred and sixty-five patients were included in the study with 88 patients having had appendicectomies for appendicitis. Analysis was compared in 4 patients groups. CT usage was less in the post guideline implementation by a total of 31%. In 2 of the groups the result was statistically significant. There was no significant change in unnecessary operations (24%) following implementation of the guideline although statistical power was weak for this analysis. Conclusion: This study suggests that hospitals with high CT usage rates for suspected appendicitis can reduce their CT usage to be consistent with the national average and clinical practice guidelines or protocols may assist in this endeavor
Introduction
Acute right iliac fossa pain is a common presenting complaint to the emergency department [1], often referred to the on-call surgical unit for further management because the main differential diagnosis is appendicitis. The diagnosis of appendicitis is often made clinically with minimal investigations. However, in some cases alternate diagnoses may masquerade as appendicitis or appendicitis may present atypically and further investigations or a period of observation is warranted.
Computed tomography (CT) scanning has high sensitivity and specificity for the diagnosis of appendicitis [2]. It has been shown to reduce the rate of negative appendicectomies without increasing the rate of perforation [3]. However, there is associated long term cancer risk which is greater for younger patients and in females (approximately 1 in 1000 for each CT scan of abdomen/pelvis [4]). In addition, there is also risk of allergy, anaphylaxis and nephrotoxicity.
At the Royal Adelaide Hospital, South Australia, CT usage on patients who have appendicectomy is higher than the national average (in 2009/2010 was 33% compared to 17% nationally) [5]. It can be argued that some of these scans are unnecessary and put patients at risk as well as increase demand on hospital resources.
In July 2012, a clinical practice guideline for the management of suspected appendicitis was introduced to the Royal Adelaide Hospital [6]. This guideline was formulated through extensive discussion with surgeons involved in the Acute Surgical Unit. It advises on various aspects of a patient care including the use of diagnostic imaging. For clinically stable patients with a typical presentation, CT is only recommended on patients that are obese or older than 50 years after a 24 hour period of observation. Thus, it does not advocate routine CT usage.
This recommendation differs from what occurs in practice. CT scans are frequently performed on older patients with typical presentation of appendicitis and are often ordered on younger patients routinely.
It was hypothesised that implementation of the guideline would lead to a lower rate of CT usage in such patients. If this is true then it may be an argument to develop and implement clinical practice guidelines for the management of other presentations such as epigastric pain, suspected diverticulitis, colitis and small bowel obstruction to further reduce the number of unnecessary CT scans.
This approach for reducing CT usage has been demonstrated in pediatric populations [7,8]. However, it is not known whether such an approach applies in our institution which manages only adult patients in which there are many logical clinical reasons to utilize CT scan for right iliac fossa pain management.
Methods
An audit of the guideline was conducted for the 3 months from May 2013. Data for this study was collected in conjunction with this audit. A series of information sessions was conducted to raise awareness of the clinical practice guideline prior to the audit period. These were delivered to emergency department doctors at one of their regular training sessions and at each surgical unit departmental meeting. Ethics approval was granted for the audit.
Relevant presentations to the Royal Adelaide Hospital Emergency Department in the audit period were identified. The inclusion criteria for the study were:
• A final diagnosis of appendicitis,
• patients referred to the surgical unit with suspected appendicitis, and
• Patients presenting to the emergency department with localised right iliac fossa pain and tenderness.
Exclusion criteria applied to the audit data generally were:
• Previous appendicectomy.
• Abdominal surgery in the last 6 weeks.
• Diagnosed urinary tract infection.
• Pregnant patients.
Presentations for the audit were identified via 4 different methods. Firstly, presentations were prospectively identified by Acute Surgical Unit registrars (who take emergency department surgical referrals) who then filled out an audit proforma. Secondly, coding data of all emergency surgical admissions with discharge diagnosis consistent with a presentation of suspected or confirmed appendicitis. Thirdly, theatre database searched for all appendicectomies and laparoscopies. Fourthly, a search of the Emergency Department database for all presentations that may be consistent with a presentation of suspected appendicitis. The search terms considered are displayed in below points.
Search terms
• Abdominal Pain
• Acute Appendicitis
• Peritonitis
• Acute abdomen
• Renal colic
• Ureteric colic
• Pelvic inflammatory disease
• Ovarian cyst
• Ovarian torsion
• Mittleschmerz
For all cases identified from these methods, discharge letters were examined to identify the cases meeting the inclusion criteria.
A comparison group of patients was identified retrospectively for patients that presented in the 3 months starting May 2011, prior to the introduction of the guideline. These patients were identified as described above with the exception of the first method since it was done retrospectively.
Data were entered into an Excel spread sheet and included demographic data, brief description of presentation, details of CT imaging, operation, histology and final diagnoses were determined for each presentation with reference to the audit forms, case notes and electronic patient information databases. Final diagnosis was determined from the best diagnostic test available with the hierarchy being histopathology then operative report, CT imaging, US imaging (positive reports only) and then clinical diagnosis.
Secondary exclusion criteria were applied specifically for this study and were:
• CT scan performed prior to presentation for investigation of the patients current symptoms.
• Duration of right iliac fossa pain greater than 7 days.
• Age of patient greater than or equal to 70 years.
• Previous diagnosis of inflammatory bowel disease.
• A patient from a high level of care nursing home or with dementia.
• Patients with severe renal failure (eGFR <30 mL/min/1.73 m
• Previous diagnosis of appendicitis with US or CT imaging.
Patients that transferred to private hospitals for further management were not excluded even though data may not have been complete (i.e. no histopathology or operative report). In such cases the plan and diagnosis was assumed to be correct. If more than one diagnosis was found and one of the diagnoses was appendicitis then presentation was counted as appendicitis (i.e. cases with appendicitis and carcinoid tumour, or if ruptured ovarian cyst was noted intraoperatively but histology demonstrated mucosal appendicitis).
For each of the two data sets (pre and post guideline), 4 groups were compiled to compare for the analysis.
• Patients that had appendicitis and had an appendicectomy,
• Patients that had operative management,
• Patients that were admitted under the surgical unit for further management,
• All patients in the data set.
The primary outcome measure was selected to be on the first group. The secondary outcome on the second group and so on. Since the hypothesis was that CT usage should be less in the post guideline implementation group, a one-tailed Chisquared test of statistical significance was applied with a pvalue <0.05 considered to be significant.
Statistical analysis was also carried out for CT scan, sex, age, diagnosis (appendicitis, alternate diagnosis or abdominal pain of unknown aetiology). Continuous variable data used t-test while categorical data used Chi-squared test. Two-tailed tests were used here to determine differences between the patient groups.
The ratios of operations that were negative for appendicitis were determined for the two periods. This was defined as the number of appendicectomies negative for appendicitis plus number of diagnostic laparoscopies divided by total appendicectomies plus diagnostic laparoscopies. A diagnostic laparoscopy was one where no other significant procedure was performed. For instance, washout of pelvis from a presumed ruptured ovarian cyst was considered a diagnostic laparoscopy while a diagnostic laparoscopy which then proceeded to oophorectomy would be removed from the calculation.
A qualitative case note review of the presentations in the group 1 post guideline implementation period that had CT scans was conducted to ascertain the clinical scenario and determine the reason why the CT was ordered. A MANTREL [9] score out of 10 was calculated for each of these presentations.
Results
There were 311 presentations identified from the general audit data prior to secondary exclusion and this was made up of 152 patients in the pre guideline group and 159 patients in the post guideline group. The average ages were 37.8 and 34.5 years respectively. Twenty and 26 patients were excluded from the pre and post protocol implementation data sets respectively. The results for each group are displayed in Table 1.
Table 1: Comparison data for each group between pre and post protocol.
| Diagnosis (%) | ||||||||
|---|---|---|---|---|---|---|---|---|
| Number of patients | CT scans (%) | Appendicitis | Abdominal pain of unknown aetiology | Other | Ave age (std) | Sex M/F (%) | ||
| Group 1 | 2011 | 41 | 14 (34.1%) | 41 (100%) | 0 | 0 | 39.4 (15.1) | 22/19 (53.7/46.3%) |
| 2013 | 47 | 10 (21.3%) | 47 (100%) | 0 | 0 | 31.2 (12.1) | 28/19 (59.6%/40.4%) | |
| p value | 0.0881 | - | - | - | 0.0057 | 0.5762 | ||
| Group 2 | 2011 | 56 | 17 (30.4%) | 41 (73.2%) | 6 (10.7%) | 9 (16.1%) | 35.4 (14.9) | 23/33 (41.1/58.9%) |
| 2013 | 62 | 10 (16.1%) | 47 (75.8%) | 7 (11.3%) | 8 (12.9%) | 30.8 (11.0) | 32/30 (51.6/48.4%) | |
| p value | 0.0331 | 0.7468 | 0.9205 | 0.6246 | 0.0617 | 0.2517 | ||
| Group 3 | 2011 | 85 | 31 (36.5%) | 48 (56.5%) | 20 (23.5%) | 17 (20.0%) | 35.2 (14.0) | 30/55 (35.3%/64.7%) |
| 2013 | 97 | 20 (20.6%) | 49 (50.5%) | 30 (30.9%) | 18 (18.6%) | 31.6 (12.0) | 39/58 (40.2%/59.8%) | |
| p value | 0.0088 | 0.4217 | 0.2646 | 0.8053 | 0.0698 | 0.4956 | ||
| Group 4 | 2011 | 132 | 36 (27.3%) | 48 (36.4%) | 60 (45.5%) | 24 (18.2%) | 35.2 (13.6) | 42/90 (31.8%/68.2%) |
| 2013 | 133 | 25 (18.8%) | 49 (36.8%) | 58 (43.6%) | 26 (19.5%) | 31.7 (12.1) | 51/82 (38.3%/61.7%) | |
| p value | 0.0506 | 0.9356 | 0.7625 | 0.7761 | 0.0273 | 0.2656 | ||
Note: There was one case of appendiceal endometriosis diagnosed on histology in 2013 was not counted as appendicitis. This patient had laparoscopic appendicectomy without prior CT.
Just over a third of patients meeting secondary exclusion criteria had appendicitis (36.4% and 36.8% in 2011 and 2013 respectively). The sex breakdown in all groups was not statistically different between pre and post guideline implementation for each group however there were more females in group 4 by a ratio of approximately 2:1. There was an increase in admissions for the post guideline group of 14% (97 compared to 85) despite the total number of cases after exclusion being very similar (133 compared to 132). P value 0.0670.
The ratio of negative appendicitis at operation is displayed in Table 2. Two cases are excluded from 2011 and 1 from 2013 for this calculation since further operative management of an alternate diagnosis was required. In the 2013 data set the presentation excluded was a 40 year old female who presented with 3 days of pain migrating to the right iliac fossa.
Table 2: Negative appendicitis at operation.
| Operative cases | Negative for appendicitis | |||
|---|---|---|---|---|
| M/F | Total | M/F (%) | Total (%) | |
| 2011 | 23/31 | 54 | 1/12 (4.3%/38.7%) | 13 (24.1%) |
| 2013 | 32/30 | 62 | 4/11 (12.5%/36.7%) | 15 (24.2%) |
| Total | 55/61 | 116 | 5/23 (9.1%/ 37.7%) | 28 (24.1%) |
She had a normal ultrasound and no CT. At laparoscopy she was found to have a mass of her ascending colon so converted to a laparotomy and right hemicolectomy. Histology was reported as diverticulitis and pericolic abscess. In the 2011 data set one case excluded from this calculation was a 25 year old female who presented with 1 day of abdominal pain initially migrated to the right iliac fossa and then developed generalised peritonitis. She did not have imaging and proceeded to laparoscopic appendicectomy. The appendix was not inflamed but gross bacterial peritonitis confirmed. Procedure was converted to exploratory laparotomy but no cause found. The other case in 2011 excluded from the calculation was a 39 year old female with 3 days of right iliac fossa pain she had a CTKUB showing a right adenexal mass. At laparoscopy she was found to have an ovarian torsion and had a right salpingo-oophorectomy.
It shows the results of the qualitative case note review on patients that had CT studies and were in the group 1 post guideline implementation data set. Thus all patients had appendicectomies for appendicitis (Table 3).
Table 3: CT scans in group 2 post protocol implementation period.
| Case | Age | Sex | MANTREL score (/10) | Reason for CT | Ordered by |
|---|---|---|---|---|---|
| 1 | 22 | F | 4 | Patient previously investigated by gastroenterologist who had suspicion that patient has Crohn’s disease. CT was ordered because of suspicion for Crohn’s ileitis. CT was non diagnostic and was equivocal for both appendicitis and ileitis. | Surgical team |
| 2 | 24 | F | 7 | Patient too unwell to delay diagnosis. Complaining of watery bowel motions for 2 weeks. CT ordered because colitis was the differential. Diagnostic for appendiceal abscess. | Surgical team |
| 3 | 50 | F | 5 | Patient obese with atypical presentation. Significant co-morbidities with Prinzmetal’s angina and on clopidogrel. Negative study for appendicitis but treated medically for appendicitis. Ongoing pain and fevers resulted in change to operative management. | Surgical team |
| 4 | 62 | F | 9 | Although typical history, tested positive for urine nitrites on dipstick without lower urinary tract symptoms. CT ordered to differentiate from UTI was positive for appendicitis. Patient the transferred to private hospital for operation. | Surgical team |
| 5 | 38 | M | 5 | Patient with medical background who wanted CT diagnosis. Positive CT. | Surgical team |
| 6 | 34 | M | 9 | Presented for 2nd time in 24 hrs. Urine tested positive for nitrites without lower urinary tract symptoms. Too unwell to await urine microscopy. Positive CT. | Emergency department |
| 7 | 43 | M | 5 | Differential diagnosis of mesenteric adenitis in the setting of URTI. CT positive. Patient transferred for operation privately as busy theatre list. | Surgical team |
| 8 | 18 | F | 5 | Patient had 3 previous laparoscopies for ovarian pathology thus suspicious of same. CT showed mildly thickened appendix. | Surgical team |
| 9 | 39 | M | 5 | Patient unwell and thought to have renal calculi. CT KUB positive for appendicitis. | Emergency department |
| 10 | 53 | F | 6 | Patient had significant co-morbidities. CT positive for appendicitis. | Surgical team |
Discussion
There was a 29% lower rate of CT usage in patients that had appendicitis and appendicectomy (group 1) in the post guideline implementation period compared to pre guideline implementation. However, this was not demonstrated to be statistically significant (p value 0.0881). There were also lower CT usage rates in the remaining groups with 41%, 35%, 31% for groups 2, 3 and 4, respectively and in groups 2 and 3 it was statistically significant (p values 0.0331 and 0.0088 respectively). The failure to show statistical significance in the first group may have been due to the reduced power with less patients in the study group (the post hoc power for group one is 38.2). If a reduction in CT scanning of at least 25% is deemed to be clinically significant then study sample size should be 177 to detect such a difference.
A reduction in CT usage rates were noted in the patients that proceeded to operative management (group 2) and patients that were admitted under a surgical team (group 3) following implementation of the clinical practice guideline. Statistical significance was demonstrated in these groups. It is encouraging that there was no significant change noted in the ratio of negative appendicitis at operation between the pre and post guideline implementation periods. This figure was approximately a quarter of operations (24%), with a large difference between male and female cases (9% and 38% respectively). However, this must be interpreted with caution as there was limited power in this study to demonstrate a difference. It is known from Krajewski et al. [3] that CT usage can reduce the negative appendicectomy rate by about half and our study did not have the statistical power to detect this influence.
Decreased CT usage in the post guideline implementation era may result in increased hospital admissions. There was an increase of 13% in the admission rate between the two periods (p value 0.067). If such an effect is real it may be justified from the view of patient care as it reduces risk of radiation exposure and contrast risks. It may be argued however, that the increased admission rate has a greater cost given that a CT scan may cost approximately $320 compared to a hospital admission of approximately $800 per day.
Most CTs in the post guideline period were ordered by the surgical team (8/10) and these studies may be the least avoidable. CT scans ordered by the emergency department may be avoided by referral to the surgical team. However, for the surgical team to avoid ordering a CT it may involve operative management or observation while awaiting further results (say urine or stool microscopy, cases 2, 4 and 6). In many clinical situations this may not be ideal depending on the clinical state (cases 2, 6 and 9) and the co-morbidities of the patient (cases 3 and 10). There are also non clinical factors that influence CT usage. There were 2 cases (4 and 7) where patients received CT in the setting of delays to the emergency theatre. There was also at least one patient (case 5) which appears to have received a CT scan because of patient preference.
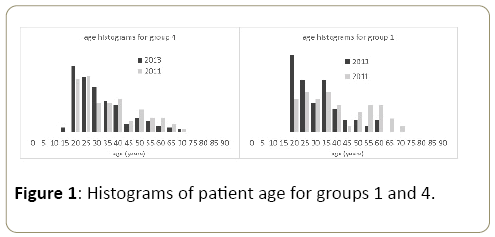
The results are suggestive that CT usage was reduced following implementation of the clinical practice guideline but is not proof of causality. However, it is suspected that there may have been a behavioural change regarding CT usage in parallel with the guideline’s introduction. Also, there was a significant change in junior and consultant surgical and emergency department staff between the 2 periods and this may contribute to different practices (Figure 1).
There are some aspects of this observational study that may be a source of bias. The 2011 data set consists of older patients in all 4 groups with relatively low p-values. Figure 1 demonstrates that there is almost a bimodal distribution of patients with a relative lack of patients in their forties. The age difference of patients is even more pronounced in group 1. This age difference may be a source of bias. The risk/benefit consideration for CT usage in older patients is more favourable since older patients have decreased absolute cancer risk as a result of radiation exposure, they are more likely to have an alternate diagnosis and are generally at greater risk of surgical and anaesthetic complications. Thus there may have been greater CT usage in the 2011 data set because of the age difference.
Another source of bias may be due to the unusual number of patients in 2011 that did not receive operative management. In 2011 there were 7 patients diagnosed with appendicitis that were medically managed. Three of these patients received CTs which showed periappendiceal abscesses and the plan was for interval appendicectomy electively. The 4 other patients were managed non-operatively because of patient preference. Had these 4 patients proceeded to surgery the effect in group 2 would have been reduced to below statistical significance (p value 0.0523).
Another source of bias may be due to the different methods used to identify patients. Specifically the lack of prospective data collection in the 2011 data set. This effect would be greatest on group 4 and less so on groups 3, 2 and 1, since these presentations were identified from coding and theatre data.
One way of increasing the effect of the guideline may be related to the promotion and general awareness of the guideline amongst relevant medical staff. This was the first guideline that was developed in our institution that relates to the management of an acute general surgical condition (excluding trauma). With the continual turnover of medical staff the series of information sessions may not have been adequate promotion. In addition, awareness may be raised generally if there were further guidelines or protocols developed for other acute general surgical conditions. Thus adherence may be greater if a series were released rather than a protocol relating to a single condition.
Conclusion
This study is suggestive that hospitals with high rates of CT usage for the investigation of suspected appendicitis can achieve reductions in CT use and consequently reduce radiation and contrast risks to patients. Such a behavioral change may be achieved via the implementation of hospital guidelines or protocols and their promotion for the management of such presentations. Reduced CT usage for such presentations was not associated with an increase in unnecessary operations but was associated with increased admissions, although statistical power was limited.
References
- Paterson HM, Qadan M, De Luca SM, Nixon SJ, Paterson-Brown S (2008) Changing trends in Surgery for Acute Appendicitis. British Journal of Surgery 95: 363-368.
- Terasawa T, Blackmore CC, Bent (2004) Systematic Review: Computed Tomography and Ultrasonography to Detect Appendicitis in Adults and Adolescents. Ann Intern Med 141: 537-546.
- Krajewski S, Brown J, Phang PT, Raval M, Brown CJ (2011) Impact Of Computed Tomography of the Abdomen On Clinical Outcomes in Patients with Acute Right Lower Quadrant Pain: A Meta-Analysis. Can J Surg 1: 43-53.
- Sodickson A, Baeyens PF, Andriole KP (2009) Recurrent Ct, Cumulative Radiation Exposure and Associated Radiation Induced Cancer Risks from Ct of Adults. Radiology 1: 175-183.
- National Health Round Table (2009/2010).
- Royal Adelaide Hospital ASU Protocol (2012) Appendicitis.
- Russell WS, Schuh AM, Hill JG (2013) Clinical Practice Guidelines for Pediatric Appendicitis Evaluation can Decrease Computed Tomography Utilization while Maintaining Diagnostic Accuracy. Pediatric Emergency Care 5: 568–573.
- Adibe OO, Amin SR, Hansen EN (2011) An Evidence-Based Clinical Protocol for Diagnosis of Acute Appendicitis Decreased the Use of Computed Tomography in Children. J Pediatr Surg 1: 192-6.
- Ohle R, O’Reilly F, O’Brien KK (2011) The Alvarado Score for Predicting Acute Appendicitis: A Systematic Review BMC Medicine 9: 139.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences