ISSN : 2574-2825
Journal of Nursing and Health Studies
The Effect of Mother and Newborn Early Skin-To-Skin Contact on the Duration of Separation and Expulsion of the Placenta
Hadeer Yahya Al-Morbaty, Asma Abdulhamid Ashmauey* and Ahlam Abdullah Al-Ghamdi
Obstetrics and Gynecologic Department, College of Nursing, College of Medicine, Imam Abdul-Rahman Bin Faisal University, Kingdom of Saudi Arabia
- *Corresponding Author:
- Asma Ashmauey
Obstetrics and Gynecologic Nursing, College of Nursing Imam Abdul-Rahman Bin Faisal University, Kingdom of Saudi Arabia
Tel: +966501642977
E-mail: aaashmauey@uod.edu.sa
Received date: May 24, 2017; Accepted date: June 03, 2017; Published date: June 08, 2017
Citation: Al-Morbaty HY, Ashmauey AA, Al-Ghamdi AA. The Effect of Mother and Newborn Early Skin-To-Skin Contact on the Duration of Separation and Expulsion of the Placenta. J Nurs Health Stud. 2017, 2:2. doi: 10.21767/2574-2825.100016
Abstract
Objective: To identify the effect of mother and newborn early skin-to-skin contact (SSC) on the duration of separation and expulsion of the placenta.
Methods: In a randomized controlled clinical trial, (28 parturient women) equally divided into two groups. Early mother and newborn SSC was applied to the experimental group, while no intervention was done to the control group. The study has been conducted in the delivery room at King Fahd Hospital of the University, AL Khobar, and Saudi Arabia.
Results: The results of this study demonstrated a statistically significant positive effect of early SSC in shortening the duration of the placental delivery. The median duration of placental delivery was (308.5 seconds) and (570 seconds) in the experimental and control groups respectively; the difference was statistically significant as P value=0.042*.
Conclusion: The significant difference between-groups favoring SSC mothers to have shorter duration time of placental delivery. Such difference should be taken into account in routine care after delivery.
Keywords
Skin-to-skin contact; Delivery; Placenta separation; Newborn
Keyphrases
Skin-to-skin contact is an aspect of child birth rearing. It has several benefits such as enhancing uterine contractions which helps in separation and expulsion of placenta in a shorter time. It also provides warmth to the newborn which enhances parenting bonding and behaviors. This article is aimed to enhance such benefits.
Introduction
Bringing a child into the world is a joyous moment. There are ups and downs when a woman ultimately becomes a mother. Skin-to-skin contact (SSC) is an aspect of child rearing which might look simple and uncomplicated to some, but it is considered an art to experienced mothers. Skin to skin contact is defined as holding the newborn naked against the mother’s or father’s skin near the chest. Skin-to-skin contact increases oxytocin levels in the maternal blood. Oxytocin is a chemical messenger that is synthesized in the hypothalamus and is released from the posterior pituitary into the peripheral circulation as a response to social contact. Its release is especially pronounced with SSC [1,2].
Studies done [3,4] have shown that the major positive impact of SSC on newborns and their parents through the release of oxytocin hormone. The importance of this hormone is in its role of stimulating uterine contractions which help enhance and decrease duration of placental separation and expulsion. It also helps the ejection of breast milk during newborn suckling, in addition to the emotional process that takes place between the mother and the newborn during childbirth. Moreover, no negative long-term outcomes were found
Skin to skin contact is promoted at delivery by allowing early contact with the newborn, and allowing the mother the time to hold her newborn. This will lead to positive maternal bonding behaviors including eye to eye contact, touching, smiling, talking, and cuddling the newborn [5,6].
Skin-to-skin contact through sensory stimuli such as touch, warmth, and odor is a powerful vagal stimulant, which among other effects release maternal oxytocin. High oxytocin level causes a mother to become familiar with the unique odor of her newborn, and once attracted to it, to prefer her own newborn’s odor above all others. When the fetus is born, he is already imprinted on the odor of his amniotic fluid. This odor imprint helps him find mother's nipple, which has a similar but slightly different odor [7,8].
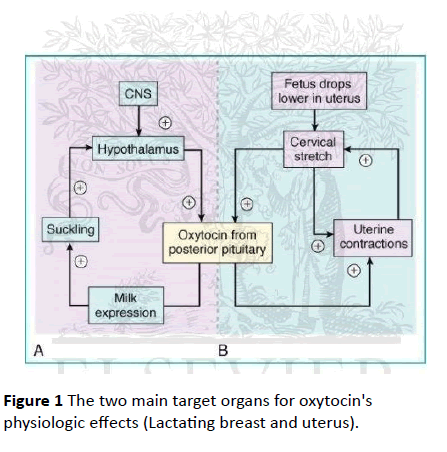
The two main target organs for oxytocin's physiologic effects are the lactating breast and the uterus. Suckling of the nipple of the lactating breast stimulates oxytocin release which is responsible for milk "let down" (allowing milk to flow) and milk ejection during breastfeeding by causing contractions of the myo-epithelial cells in the lactating mammary gland, the levels of oxytocin are based on the amount of such contact. Nursing during the initial hour after birth cause oxytocin to surge to exceptional levels in both mother and newborn [9,10]. Oxytocin levels are higher in mothers who exclusively breastfeed than in those who use supplementary bottles. The “after pains” often occur during nursing signaling that oxytocin is being released and through blood stream stimulates uterine contractions which decrease the chance of maternal death due to postpartum hemorrhage [11] (Figure 1).
Placental separation typically occurs within a few minutes after delivery. As the fetus is born, the uterus spontaneously contracts around its diminishing contents. The sudden decrease in the uterine size is accompanied by a decrease in the area of placental implantation. This results in the decidua layer separating from the uterine wall. Once the placenta separates from the wall of the uterus, the uterus continues to contract until the placenta is expelled. This process typically takes 5 to 20 minutes i.e. (300 to 1200 seconds) after delivery of the baby and occurs spontaneously [12]. Skin-to-skin contact should be started during the first minute after birth and throughout the third stage of labor, to produce elevated levels of oxytocin aiding in separation and expulsion of the placenta [3,13].
Furthermore, human babies are born helpless, needing to be entirely cared for and protected [1]. Skin-to-skin contact immediately after birth has a positive effect on the newborn. It maintains his body temperature normal better even than in an incubator [2]. When a newborn is taken out of this natural habitat, it shows all the physiologic signs of being under significant stress. A newborn not in close contact with his mother (or father) by distance (under a heat lamp or in an incubator) or swaddled in a blanket, may become too sleepy or lethargic or becomes disassociated altogether or cry and protest in despair [14]. For all these reasons, it has been recommended to keep mother and newborn together for at least the first hour of life [3].
Unfortunately, in industrialized societies hospital routines may significantly disrupt early mother newborn interactions and have harmful effects. To overcome this matter, the initial physical assessment of the stable newborn can be performed while the newborn is SSC with the mother’s chest/abdomen after delivery. In addition, APGAR scoring which is a rapid newborn assessment of five physiological signs can be taken as well as suctioning of the newborn’s airway secretions. The newborn must be covered across the back with a pre-warmed blanket and with a dry cap to prevent heat loss. Ideally, all other interventions are delayed until at least after the end of the first breastfeeding [15,16].
Aim: The aim of the current study was to evaluate the effect of early SSC between mother and newborn on the duration of placental delivery.
Hypothesis: The researcher hypothesizes that SSC leads to the reduction of the duration of placental delivery.
Methods
The study was conducted in the labor and delivery room at King Fahd Hospital of the University, AL Kho bar, Saudi Arabia. All parturient women, aged 20-40 years, who had a normal singleton full term pregnancy, between 38-41 weeks of gestation, in the first stage of labor with cephalic presentation were included in this study. Those who had physical, mental, medical and obstetrical problems or had previous uterine surgical scar were excluded from the study. A total of 28 parturient women were randomly assigned alternatively into control and experimental groups.
An informed written consent was obtained from each parturient woman after explaining the purpose of the study and before data collection. An interview questionnaire sheet was used to collect the socio- demographic and obstetrical data and was collected from the parturient women in both groups during the first stage of labor. The assessment items related to the second and third stage of labor such as APGAR score, temperature of the newborn, and respiratory distress syndrome was collected during and after delivery. A ‘stop watch’ was used to calculate the duration of the third stage of labor in both groups starting from the complete expulsion of the fetus till the complete placental delivery (separation and expulsion of the placenta). A comparison between both groups was done to identify the effect of mother and newborn early SSC on placental delivery using SPSS version 15 as statistical software. A P-value of ≤ 0.05 was considered statistically significant.
Results
Both groups were comparable regarding socio-demographic data. Furthermore, there were no statistical differences between both groups regarding the obstetrical data except for the time of delivery (Table 1).
| Socio-demographic characteristics | Experimental N=14 |
Control N=14 |
Test and P value | ||
|---|---|---|---|---|---|
| Age (years) | Z=0.346 P=0.7 | ||||
| Range | 20-40 | 22-35 | |||
| Mean ± SD | 28.4 ± 6.1 | 27.5 ± 3.6 | |||
| Median (IQR) | 27.50 (10) | 27 (6) | |||
| Educatio | No. | % | No. | % | |
| Read/write | 1 | -7.10% | 0 | 0.00% | FETP=0.7 |
| Primary education | 4 | -28.60% | 3 | -21.40% | |
| Secondary education | 7 | -50.00% | 6 | -42.90% | |
| University education | 1 | -7.10% | 5 | -35.70% | |
| Others (Master) | 1 | -7.10% | 0 | 0.00% | |
| Occupation | |||||
| House wives | 11 | -78.60% | 12 | -85.70% | FETP=1 |
| Working mothers | 3 | -21.40% | 2 | -14.30% | |
| Income (SR/month) | |||||
| <3000 SR | 3 | -21.40% | 3 | -21.40% | FETP=1 |
| 3000- | 3 | -21.40% | 5 | -35.70% | |
| 6000- | 6 | -42.90% | 1 | -7.10% | |
| ≥9000 | 2 | -14.30% | 5 | -35.70% | |
| Nationality | |||||
| Saudi | 10 | -71.60% | 12 | -85.80% | FETP=0.6 |
| Bahraini | 0 | 0.00% | 1 | -7.10% | |
| Somali | 1 | -7.10% | 0 | 0.00% | |
| Sudanese | 1 | -7.10% | 0 | 0.00% | |
| Egyptian | 1 | -7.10% | 0 | 0.00% | |
| Indonesian | 1 | -7.10% | 1 | -7.10% | |
| Region | |||||
| Alkhobar | 12 | -85.70% | 12 | -85.70% | FETP=1.0 |
| Dammam | 1 | -7.10% | 1 | -7.10% | |
| Qateef | 0 | (0 .0%) | 1 | -7.10% | |
| Jizan | 1 | -7.10% | 0 | 0.00% | |
IQR=Inter quartile range; FETP=Fisher’s exact test
Table 1 Distribution of the studied experimental and control groups of parturient women according to their socio-demographic characteristics.
It was interesting to notice that, in the current study all deliveries (100%) in the experimental group occurred at evening time compared to only four deliveries (28.6%) in the control group. The observed difference was statistically significant as P value=0.001). All other observed differences were not statistically significant (Table 2).
| Obstetrical History | Experimental N=14 | Control N=14 | Test and P value | ||
|---|---|---|---|---|---|
| Past Obstetrical History | No. | % | No. | % | |
| Gravidity | |||||
| 2 | 4 | 28.60% | 9 | 64.40% | Z=1.248 P=0.2 |
| 3 | 6 | 42.90% | 1 | 7.10% | |
| 4 | 2 | 14.30% | 2 | 14.30% | |
| 5 | 0 | 0.00% | 1 | 7.10% | |
| >5 | 2 | 14.20% | 1 | 7.10% | |
| Range | 2-8 | 2-8 | |||
| Mean ± SD | 3.4 ± 1.6 | 3± 1.7 | |||
| Median (IQR) | 3 (2) | 2 (2) | |||
| Parity | |||||
| 0 | 1 | 7.10% | 2 | 14.30% | Z=1.177 P=0.2 |
| 1 | 4 | 28.60% | 7 | 50.00% | |
| 2 | 6 | 42.90% | 2 | 14.30% | |
| 3 | 1 | 7.10% | 2 | 14.30% | |
| ≥ 4 | 2 | 14.30% | 1 | 7.10% | |
| Range | 0-6 | 0-5 | |||
| Mean ± SD | 2.1 ± 1.6 | 1.5 ± 1.3 | |||
| Median (IQR) | 2 (1) | 1 (1) | |||
| Miscarriage | |||||
| 0 | 10 | 71.40% | 9 | 64.30% | FETP=1.0 |
| 1 | 4 | 28.60% | 4 | 28.60% | |
| 2 | 0 | 0.00% | 1 | 7.10% | |
| No. of living children | |||||
| 0 | 2 | 14.30% | 2 | 14.30% | Z=0.742 P=0.5 |
| 1 | 4 | 28.60% | 7 | 50.00% | |
| 2 | 5 | 35.70% | 2 | 14.30% | |
| 3 | 1 | 7.10% | 2 | 14.30% | |
| ≥ 4 | 2 | 14.30% | 1 | 7.10% | |
| Range | 0-6 | 0-5 | |||
| Mean ± SD | 2 ± 1.7 | 1 ± 1.3 | |||
| Median (IQR) | 2 (-1) | 1 (-1) | |||
| Obstetrical History (cont.) | |||||
| current pregnancy: Gestational age | |||||
| Range | 38-40 | 38-41 | Z=0.346 P=0.7 | ||
| Mean ± SD | 38.8 ± 0.9 | 39 ± 1.03 | |||
| Median (IQR) | 38.5 (2) | 39 (2) | |||
| Pregnancy Planning | |||||
| Planned | 11 | 78.60% | 10 | 71.40% | FETP=1.0 |
| unplanned | 3 | 21.40% | 4 | 28.60% | |
| Current delivery: Time of delivery | |||||
| Morning (AM) | 0 | 0.00% | 10 | 71.40% | X2=15.556* |
| Evening (PM) | 14 | 100.00% | 4 | 28.60% | P= <0.001 |
| Presence of episiotomy | |||||
| Yes | 5 | 35.70% | 6 | 42.90% | X2=0.150 |
| No | 9 | 64.30% | 8 | 57.10% | P=0.7 |
| Presence of tear | |||||
| First degree | 9 | 64.30% | 7 | 50.00% | X2=0.583 |
| No tear | 5 | 35.70% | 7 | 50.00% | P=0.4 |
N.B: level of the fundus is constant for both groups (100%)
*=Statistically significant difference
Table 2 Distribution of the studied experimental and control groups of parturient women according to their obstetrical history.
Surprisingly, the newborns with SSC were warmer than the control group. The newborns’ temperature ranged between (35.9°C to 37.5°C) with SSC compared to (35.5°C to 36°C) in the control group under warmer which was statistically significant, as P value=< 0.001, with a median of 36.5°C vs. 35.7°C in the experimental vs. control group respectively. The mean temperature was 36.5 ± 0.5 in the experimental group vs. 35.7 ± 0.7 in the control group. But, there were no differences in all other newborns’ characteristics (Table 3).
| Newborns Characteristics | Experimental N=14 | Control N=14 | Test and P value | ||
| No. | % | No. | % | ||
| Presence of Caput Succedaneum | |||||
| Yes | 4 | 28.60% | 5 | 35.70% | FETP=1.0 |
| No | 10 | 71.40% | 9 | 64.30% | |
| Presence of Cephal hematoma | |||||
| Yes | 0 | 0.00% | 2 | 14.30% | FETP=0.5 |
| No | 14 | -100% | 12 | 85.70% | |
| NICU admission | |||||
| Yes | 0 | 0.00% | 1 | 7.10% | FETP=1.0 |
| No | 14 | 100% | 13 | 92.90% | |
| APGAR Scoring at 1 minute | |||||
| Range | 08-Sep | 06-Sep | Z=0.061 p=0.95 | ||
| Mean ± SD | 8.7 ± 0.5 | 8.50 ± 1.0 | |||
| Median (IQR) | 9 (1) | 9 (1) | |||
| APGAR Scoring at 5 minutes | |||||
| Range | Constant value | 09-Oct | Z=2.121 p=0.3 |
||
| Mean ± SD | =10 | 9.7± 0.5 | |||
| Median (IQR) | 10 (1) | ||||
| Temp. Newborn (˚C) | |||||
| Range | 35.9-37.8 | 35.5-36 | Z=4.301 p=< 0.001* | ||
| Mean ± SD | 36.5 ± 0.5 | 35.7 ± 0. 7 | |||
| Median (IQR) | 36.5 (0.7) | 35.7 (0.3) | |||
N.B: NICU=Neonatal Intensive Care Unit
*=Statistically significant difference
Table 3 Distribution of the studied experimental and control groups of parturient women according to their newborns’ characteristics.
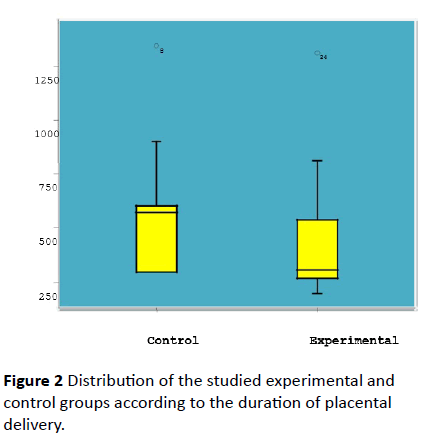
The results demonstrated a statistically significant positive effect of early SSC on shortening the duration of placental delivery (separation and expulsion of placenta). Half (50.0%) of women in the experimental group had shorter duration of the placental delivery (< 300 seconds) compared to none (0.0%) of women in the control group. On the other hand, less than half (42.9%) of women in the experimental group compared to (92.9%) of women in the control group had normal duration (300 to 1200 seconds) of placental delivery. The median duration of placental delivery was (308.5 seconds) and (570 seconds) in the experimental and control groups respectively; P=0.042 (Figure 2), (Table 4).
| Duration of placental delivery (in seconds) | Experimental N=14 | Control N=14 | Test and P value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Shorter (< 300 sec.) | 7 | 50.00% | 0 | 0.00% | ADR=0.5 NNS=2 |
| Normal (300-1200 sec.) | 6 | 42.90% | 13 | 92.90% | |
| Delayed (>1200 sec.) | 1 | 7.10% | 1 | 7.10% | |
| Range | 200-1312 | 300-1345 | Z=2.033 P=0.042* |
||
| Mean ± SD | 441.4 ± 303.7 | 550.4 ± 290.4 | |||
| Median (IQR) | 308.5 (278) | 570 (300) | |||
Z=Mann-Whitney
ADR=Attributable Duration of placental delivery Reduction
NNS=Number needed to apply SSC
*=Statistically significant difference
Table 4 Distribution of the studied experimental and control groups of parturient women according to the duration of placental delivery.
From the results of the current study it was noticed a negative correlation between newborn’s temperature and the duration of placental delivery in the experimental group. This means that the warmer newborn is SSC, the shorter duration of placental delivery (Table 5).
| Newborn’s variables | Duration of placental delivery | |||
|---|---|---|---|---|
| Experimental | Test and P value | Control | Test and P value | |
| Presence of Caput succedaneum | ||||
| Yes | Md. =252.50 | Z=1.556 | Md. =300 | Z=0.768 |
| No | Md. =320.50 | P=0.1 | Md. =600 | P=0.4 |
| Presence of Cephal-hematoma | ||||
| Yes | Not found | ---------- | Md. =600 | Z=0.191 |
| No | ----------- | Md. =570 | P=0.8 | |
| NICU admission | ||||
| Yes | Not found | ---------- | 600 seconds | Z=0.649 |
| No | ------------ | Md. =540 | P=0.5 | |
| APGAR Scoring at 1 minute | r=0.08 | P=0.8 | r=0.25 | P=0.4 |
| APGAR Scoring at 5 minutes | Value was constant =10 for all | r=0.000 | P=1 | |
| Temp. Newborn (°C) | r=- 0.37 | P=0.2 | r=0.56 | P=0.04* |
N.B: r=correlation coefficient for quantitative variables
Qualitative variables are presented as median (Md.)
Z=Man-Whitney test
NICU=Neonatal Intensive Care Unit
*=Statistically significant difference
Table 5 The relationship between newborn’s variables and the duration of placental delivery.
Discussion
There was a clear evidence that SSC has both physiological and behavioral regulation benefits for both mothers and infants [1]. In a study done in this context, its findings clearly stated that SSC and breastfeeding are with no doubt the most natural cost-efficient means of bonding between the mother and her newborn. The results of the present study revealed that there is a significant relationship between SSC and the duration of placental delivery (separation and expulsion of placenta). The study demonstrates that we need to treat two women with early SSC to reduce the duration of placental delivery in one of them, NNS=2 (Table 4). This is in congruent with a published study done, they have demonstrated the effect of early SSC between the mother and the newborn on the time to expel placenta. A tendency towards shorter time of placental delivery was found in SSC group [5].
Strikingly, it was evident that there is a significant correlation between the duration of placental delivery and newborns’ temperature. The newborns in the experimental group were warmer than those in the control group. This may be attributed to the fact that the SSC may imply better thermal regulation for newborns and refuting the belief of many care providers that skin-to-skin contact may cause a low temperature in newborns, where the heat is transferred from the body of the mother to the body of the newborn. We noticed a negative correlation between newborn’s temperature and the duration of placental delivery in the experimental group. This means that the warmer newborn is SSC, the shorter duration of placental delivery (Table 5). This is supported by several studies which have demonstrated the beneficial effects of SSC on the thermal control of newborn. In the study done in this context [5], its findings mentioned that an increase in temperature of infants was found only in the first few minutes of life in SSC group. Although they observed that the temperature registered in the SSC group in the first minute of life is significantly lower than in the control group, a tendency towards greater recovery from hypothermia at 5 minutes in SSC group was found. The mean temperature at 1 min of life was 36.6°C ± 0.79°C in the SSC group vs. 36.9°C ± 0.58°C in the control group. The differences between the delivery room temperature and the heater temperature may be the reason for this temperature difference.
The higher temperature in the early postnatal period has been attributed to the increase in metabolism that takes place in the infant after birth. Studies had demonstrated how those infants born by vaginal delivery presented higher plasma catecholamine levels, which causes peripheral blood vessel constriction and elevated temperature. Another implied mechanism was the conduction of temperature from the mother to the infant. Some investigators referred to the increase in axillary temperature in mothers during SSC; therefore, heat was transferred from the body with higher temperature (the mother) to the body with lower temperature (the infant). The newborns placed in SSC with their mothers were more likely to be warmer because of the thermal response of maternal skin temperature (mediated by oxytocin) in reaction to skin-to-skin contact with their newborns [17,18].
Conclusion
The current study enabled the researcher to utilize the benefits of early SSC among the parturient women and proved the hypothesis that SSC leads to the reduction of the duration of placental delivery in half of parturient women. We recommend the implication of early SSC in our routine practice in all maternity hospitals and it should be an available choice for all parturient women.
Acknowledgment
First and foremost, praises and thanks to Allah then the authors gratefully acknowledge Imam Abdul-Rahman Bin Faisal University (IAU) for this opportunity. Special thanks for the supervisors: Dr. Asma Abdull-hamid Ashmauey, professor of Ob/Gyne, College, of Nursing, IAU and Dr. Ahlam Abdullah A l Ghamdi, Assisted Prof. College of Medicine, IAU, Consultant Ob/Gyne, Reproductive Endocrinology and Infertility, KFHU for their meticulous supervision, unlimited help and guidance. We acknowledge Dr. Hoda Ghareeb Mohamed, Associate professor, Community Medicine, Preventive and Social Health for her valuable help in the statistical analysis. Special thanks for all nursing staff, residents and supervisors of the labor and delivery unit in the King Fahd Hospital of the University, AL Kho bar, Saudi Arabia.
References
- Linda F, Palmer DC (2002) Attachment parenting international news. [www.thebabybond/.com]. Accessed on: 15 May 2012.
- Molina PE (2012) Endocrine Physiology (3rdedn). McGraw-Hill, New York.
- Roos N (2011) How bonding effects hormones in kangaroo mother care. [ezinearticles.com/?How-Bonding-Effects-Hormones-in-Kangaroo-Mother-Care&id=5759073]. Accessed on: 30 October 2012.
- Larimer K (1999) Kangaroo care benefits. [www.prematurity.org/baby/kangaroo.html]. Accessed on: 30 October 2012.
- Gabriel M, Martin L, Escobar L, Villalba F, Blanco R, et al. (2010) Randomized controlled trial of early skin-to-skin contact: Effects on the mother and the newborn. Acta Pediatric 99: 1630-1634.
- Moore ER, Anderson GC (2007) Randomized controlled trial of very early mother-infant skin-to-skin contact and breastfeeding status. J Women’s Health 52: 116-125.
- Forster DA, McLachlan HL (2007) Breastfeeding Initiation and birth setting practices. J Women’s Health 52: 273-280.
- Fraser DM, Cooper MA (2008) Myles textbook for midwives (14thedn) UK Churchill Livingstone, London, pp: 515-517.
- Ricci SS (2009) Essentials of maternity, newborn, and woman’s health nursing. (2ndedn) Welter's Kluwer Health, Lippincott Williams & Wilkins, USA.
- Illingworth RS (1991) The normal child, some problems of early years and their treatment (10thedn) Churchill Livingstone, Edinburgh, London, New York and Tokyo pp: 2-35.
- Kiss A, Mikkelsen JD (2005) Oxytocin-anatomy and functional assignments: A minireview. Endocarp Regal PubMed 16468232: 97-105.
- Chapman L, Durham R (2010) Intrapartum assessment and intervention. In: Chapman L, Durham R, (Eds). Maternal-Newborn Nursing: The critical components of nursing care (1stedn). F.A. Davis company, Phladelphia, pp: 160-165.
- Browne JV (2004) Early relationship environments: Physiology of skin-to-skin contact for parents and their preterm infants. Clin Perinatol 31: 287-298.
- Newman J, Kernerman E (2009) The importance of skin to skin contact. [www.nbci.ca/index.php?option=com_content&view=article&id=82:the-importance-of-skin-to-skin-contact-&catid=5:information&Itemid=17]. Accessed on: 30 October 2012.
- Chapman L, Durham R (2012) Intrapartum assessment and intervention. In: Chapman L, Durham R, (Eds). Maternal-Newborn Nursing: The critical components of nursing care. (2ndedn) F.A. Davis company, Phladelphia pp: 160-165.
- Moore ER, Anderson GC, Bergman N (2007) Early skin-to-skin contact for mothers and their healthy newborn infants. Cochrane database syst rev 3: 1-12.
- Puig G, Sguassero Y (2007) Early skin-to-skin contact for mothers and their healthy newborn infants. [www: apps.who.int/rhl/newborn/gpcom/en/index.html] Accessed on: 30 October, 2012.
- Chaparro CM, Lutter C (2007) Mother and newborn skin-to-skin contact. In: Chaparro CM, Lutter C (Eds). beyond Survival: International delivery care practices for long-term maternal and infant nutrition, health and development. Pan American Health Organization: Washington D.C pp: 16-18.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences