The Assessment of the Compliance to Occupational Health and Safety Measures among the Health Workers in Three Selected Districts Health Facilities in Kigali, Rwanda
Chinenye Mercy Nwankwo1*, Simon Karanja2 and Hilda Vasanthakaalam3
1Department of Public Health, Jomo Kenyatta University of Agriculture and Technology, Kenya
2School of Public Health, Jomo Kenyatta University of Agriculture and Technology, Kenya
3Department of Nutrition, National University of Rwanda, Kenya
- *Corresponding Author:
- Chinenye Mercy Nwankwo
Department of Public Health
Jomo Kenyatta University of Agriculture and Technology, Kenya
Tel: +2546752028
E-mail: mercynjkuat@gmail.com
Received date: March 14, 2016; Accepted date: April 19, 2016; Published date: April 22, 2016
Citation: Nwankwo CM, Karanja S, Vasanthakaalam H (2017) The Assessment of the Compliance to Occupational Health and Safety Measures among the Health Workers in Three Selected Districts Health Facilities in Kigali, Rwanda. J Biomed Sci Appl Vol. 1 No. 2:8.
Abstract
Background: Globally, work place safety does not occur without a challenge especially in resource constrained set up. This is further worsened by poor hazard control system, lack of task management system and role ambiguity. Aim: This study tried to assess the compliance to occupational health and safety measures among workers from study site. Methodology: Study adopted a cross sectional design involving both qualitative and quantitative data collection approaches. It was carried out among health care workers in the three selected District health facilities in Kigali, Rwanda between July 2016 and December 2016. From a study population of 631 health care worker, about 249 participants were selected systematically, adopting probability proportional to size sampling, Semi structured questionnaire, a focus group discussion guide, an observational checklist was used and policy document review carried out. Data analysis involved descriptive and inferential statistics. Differences in the parameter of estimate were considered significantly different at P<0.05. Results: Study findings showed that four factors were significantly associated with compliance to safety regulations with P<0.05, these includes; factor related to policy enforcement, Hazard report system, Individual level associated factors and health facility level associated factors. Policy gap analysis and focus group discussion revealed low compliance despite accreditation system adopted to improve quality of care in Rwanda, especially in relation to work environment design, hazard detection, case identification, and investigation and follow up documentation. The waste management practices were not in full compliance with international standard. Conclusion: Finally, there was real evidence of poor compliance to hazards incident reports, investigations, follow up and training gap and absence of safety guidelines including individual character short falls. Therefore the government, workers, and health facility administrators must address the policy enforcement related issues, carryout re-structuring, with improved safety training and surveillance, enhanced safety communication and workers capacity building.
Keywords
Compliance; Occupational hazards; Health safety measures; Health facility; Health policy
Introduction
Workplace safety greatly depend on the enforcement of occupational safety policy and inspection of workplace environment to ensure compliance with health and safety standard. Compliance is obtained specifically through active efforts made to reduce occupational hazards when it is not possible to effectively stop it [1]. Occupational health and safety measures; provides moral, legal and economic benefits. It has therefore become necessary for institutional bodies to take up the duty and responsibility of ensuring safety of its ‘employees. It could be seen as an ancient way of protecting, preventing and avoiding consequences that could affect workers’ safety and health [2].
It is increasingly recognized that health workers are subject to a variety of health hazards [3]. Positive safety culture and working in an environment with strict instructions on safe work procedures and commitment to safety measures significantly reduces the risk of hazards [4,5]. Conformity to safety regulations entails compliance and obedience based on strong influences which might be diverse and varied through surveillance activities [6].
However, occupational health risks especially in relation to work overload, lack of task control and role ambiguity and poor organization might be a great threat [7]. Absence of training increases risk and poor compliance to set rule and safety regulations and techniques. Regular supervision and provision of safety devices and training are more likely to reduce health risks in work place. Also if sanctions are given to workers for noncompliance and engaging in high-risk behaviour, it would serve as a deterrent to others who do not believe that their employers are concerned with their safety [8,9].
Perception that safety information’s is not readily available is associated with lower safety efficacy and lower levels of compliance [10]. In workplaces, new employees may start taking unsafe shortcuts while performing job tasks because other more seasoned employees are doing so. While a new worker may not initially perceive these shortcuts as dangerous, because they want to conform to group activities not minding if it is risky [11,12]. Nearly two decades ago, the World Health Organization declared that “access to occupational health services should be ensured for all workers of the world, irrespective of age, sex, nationality, occupation, type of employment, or size or location of the workplace” [13].
The perspectives of this dissertation work are based on the ecological models, evolved from behavioural sciences and public health, examines the interactions between individuals and their physical and socio-cultural environments. The model implies that individual behaviour is affected by and impacts on the surrounding environment and on social interactions [14]. Certain studies have suggested that intense mental fatigues are slightly more frequent among health worker of senior cadres unlike the technicians or auxiliary workers, and from workloads [15].
Also according to stress theory, occupational stress from physical and psychological threats in workplace might contribute to emotional anxiety, anger, violence and aggressive behaviour in workplace, likewise psychological strain, and burnout [16,17].
Most developing countries may not have surveillance for occupational exposure to health hazards in health institutions, thereby limiting estimation of the exact magnitude of such hazards. Universal precaution awareness education has not been fully pronounced among health care workers, particularly in developing countries.
Due to the demand for effectiveness of care, for decision making in health setting and for policy adjustment and other stringent measures to help unburden Rwandan health sector in area of occupational hazards and safety issues. Development of standards and guidelines and the need for cost containment, health services research has become much more prominent in recent years. There were few published empirical studies on the work in OHS in this part of the continent. Result of the study will generate more insight on gap that exists in meeting the occupational safety of health personnel in Rwanda [17].
Study Objective was to determine the compliances to safety standards adopted by the hospital management and the health care workers for the protection of health workers based on policy guidelines in hospitals.
Methods
The study was carried out in Kigali city from the three existing district hospitals that serve the entire Kigali city; Muhima Hospital in Nyarugenge District, Kibagabaga Hospital in Gasabo District and Masaka Hospital in Kicukiro District. Kibagabaga District Hospital receives an average of 230 patients every day and has 120 beds. It has 5 medical specialists, 11 general physicians, 54 nurses, 27 midwives and 89 support staff. Masaka District Hospital serves a population of 355,195 people, with a bed capacity of 148 and about 110 patients per day in outpatient department and 787 in-patients per month. The hospital has one medical specialist, 12 general physicians, 103 nurses, 29 midwives and 92 support staff. Also, Muhima District Hospital serves about 326,478 people, receives about 201 out-patients daily. The staff capacity comprised; 5 medical specialists, 17 general physicians, 45 nurses, 52 midwives and 59 support staff.
The study adopted a cross-sectional design with both quantitative and qualitative approaches. The sample was calculated using Slovene’s formula [18]:
n=N/1+N(e)2=n
where, n=sample; N=Population; e=marginal of error, e=0.05
n=631/(1+631*0.052)
n=249
Sample size for each stratum in the health facilities was worked out by stratification weighted sampling for each specific sample sizes for example: Sample size for medical Doctors in Muhima District Hospital.
Note: nh=nNh/Nn1=249 (22)/63=9
Purposive sampling technique was used to determine the study site which is the three existing district health facilities in Kigali, study samples was drawn systematically based on the size and threshold of health care workers. Stratified sampling technique was used to select different categories of health care workers due to their heterogeneity. Systematic sampling technique with a sampling interval of 7 was used to select participants from the population frame of workers in each of the cadres of the health workers in the three health facilities for the study.
The study instruments were interviewer administered questionnaires, a focused group discussion guide and observational checklists. Policy document for hospital health and safety standards was reviewed to determine level of compliance to international standard. The first part of the questionnaire sort information on respondent demographic profile, the second part seeks questions related to the independent variable (IV) and the third part covering the dependent variable (DV). Meanwhile, further information was sought through focus group discussion, observation and policy document review to help improve the quality of the generated information for better understanding of the problem.
The validity of instruments was ensured via two assessors/ experts in the field of study, who examined the content in the questionnaire. These experts also assisted in assessing the phrasing of the questions to avoid ambiguity. The researcher compiled the responses from the two experts and computed the Content Validity Index (CVI). CVI=57/66=0.86. To ensure reliability of the instruments, data collection instruments were pre-tested in a similar population at Sante Da La Criux Hospital (a private hospital in Kigali) to ensure the validity of the instrument. This was followed by correction of the instrument to eliminate ambiguity. The questionnaire was further translated into the local language (Kinyarwanda) for ease of data collection.
The data generated from the study was coded and entered into the computer programs EPI-Info data and exported to SPSS (version 21). Descriptive statistics (frequencies, 95% CI) were used for exploratory purposes. The variables were weighted using average score rating and the variables were further put into categories of three. Test for the degree of association between independent and dependent variables were done using the Pearson chi-squared test. Differences between the parameter of estimates were deemed significantly different at P<0.05. For the qualitative data, thematic analysis was used.
The researcher in the course of the study handled information with confidentiality and respects for respondent. Also consent and approval of participation obtained from each study participants. In addition, authorization and approval to conduct the study was obtained from the study site and from the Rwandan National Ethical Board and from the Ministry of Health.
Results
The respondent personal characteristics in this study were described according to age, education level and professional categories, others includes, risks behaviour such as smoking and alcohol use (Table 1).
| Background Characteristics (n=249) | Frequency | Proportion (%) | 95% Confidence Intervals |
|---|---|---|---|
| Sex | |||
| Male | 105 | 42.2 | (36.96-48.57) |
| Female | 144 | 57.8 | (51.43-64.03) |
| District Name/Health Facility: | |||
| Nyarugenge (Muhima) | 85 | 34.1 | (28.27-40.39) |
| Gasabo (Kibagabaga | 74 | 29.7 | (24.11-35.81) |
| Kicukiro (Masaka) | 90 | 36.1 | (30.17-42.45) |
| Age group of the study Participants | |||
| 18 to 29years | 76 | 30.5 | (24.86–36.65) |
| 30 to 39years | 137 | 55 | (48.61–61.30) |
| 40 to 49 | 31 | 12.5 | (8.6 –17.20) |
| 50 years and above | 5 | 2 | (06.55–4.66) |
| Duration in service/Length of years of service | |||
| Less than 3 years | 66 | 26.5 | (21.13-32.45) |
| Between 3 and 6 years | 109 | 43.8 | (37.51-50.18) |
| Between 7 to 9 years | 46 | 18.5 | (13.85-23.86) |
| 10 Years and above | 28 | 11.2 | (7.60-15.84) |
| Participants Education: | |||
| None | 3 | 1.2 | (02.49-3.48) |
| Primary | 39 | 15.7 | (11.38-20.78) |
| Secondary | 58 | 23.3 | (18.19-29.04) |
| Diploma / Certificate | 107 | 43 | (36.74-49.37) |
| Degree | 33 | 13.3 | (9.30-18.11) |
| Post Graduate | 9 | 3.6 | (01.67-6.75) |
| Smoking: | |||
| Yes | 2 | 0.8 | (00.09-02.87) |
| NO | 247 | 99.2 | (97.13-99.90) |
| Alcohol: | |||
| Yes | 23 | 9.2 | (05.95-13.54) |
| No | 226 | 90.8 | (86.46-94.05) |
Table 1: Distribution of study participants with regard to Socio-demographic characteristics.
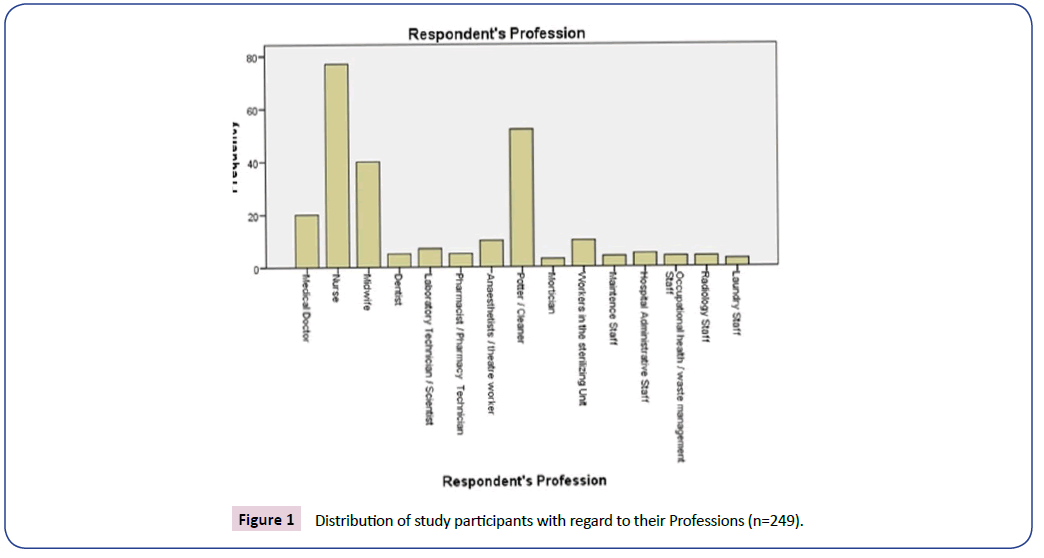
Out of 249 study participants 77 (30.9%, 95% C.I=25.24-37.07) were Nurses; 52 (20.9%, 95% C.I=16.09-26.47) were Potters and Cleaners, while 40 (16.1%, 95% C.I=11.73-21.23) were Midwives. Meanwhile, the least proportion of professional categories that participated in the study were the Laundry staff accounting for 3 (1.2%, 95% C.I=00.25-03.48) (Figure 1).
Findings on factors that lead to poor adherence to safety guideline showed that 90 (36% 95% C.I=30.17-42.45) believe that there are poor policy implementation and regulation. Also 104 (41.8%95% C.I=35.57-48.16) respondent said that forgetfulness of the right procedures in line with policy and distractions hinders compliance to safety rules. Another thing is poor timing of work schedule and carelessness 111 (44.6% 95% C.I=38.30-50.99), unsafe working environment 107 (43% 95% C.I=36.74-49.37), Poor policy enforcement system 112 (45%95% C.I=38.69-51.39) and occupational hygiene practices 130 (52.2%95% C.I=45.81- 58.56).
Other findings based on participants response on compliance to post exposure universal precautions, with regards to careful handling and disposing of sharp instruments during and after procedures showed was 219 (88%, 95% C.I=83.25-91.72), also practice of immediate washing of hands and other skin surfaces after contact with blood was about, 211 (84.7%, 95% C.I=79.66- 88.97). About, 117 (47%, 95% C.I=40.66-53.39) responses revealed noncompliance to the re- evaluation of exposed health care workers within 72 hours.
The summary picture of the participants rating on hospital management commitment occupational policy guidelines, showed a mean index for all aspects (mean=2.9283). These results indicated that there is moderate level of hospital management commitment and leadership to occupational safety Policy guidelines. The hospital waste management program details on inspection and interview showed that: hospital waste management are not fully in line with policy rule, there are no evidence of health waste management reduction facility plan and updated document (in case of changes in production technology every five years). The waste management companies have no real program and develop rules on recovery and disposal of the waste.
Furthermore, the statistics results on policy compliance showed a significant relationship with Health facility associated factors (0.049<0.05) and Strategies for Hazards prevention in hospital (0.02<0.05). Also significant is health Facility Safety Programs (0.000<0.05) and Employees Participation on safety (0.020<0.05) (Table 2).
| Compliance to safety regulations and health facility factors associated with occupational hazards | High Level compliance | Moderate level compliance | Low level compliance | Chi-square | d.f. | P-value | Interpretation | |
|---|---|---|---|---|---|---|---|---|
| Health facility factors associated with occupational hazards | High Level of health facility associated factors to occupational hazards | 33 | 17 | 23 | 9.544a | 4 | 0.049 | Significant |
| 33.3% | 23.0% | 30.3% | ||||||
| Moderate Level of health facility associated factors to occupational hazards | 40 | 37 | 44 | |||||
| 40.4% | 50.0% | 57.9% | ||||||
| Low level of health facility associated factors to occupational hazards | 26 | 20 | 9 | |||||
| 26.3% | 27.0% | 11.8% | ||||||
| Compliance to safety regulations in association with level of awareness of occupational health and safety | ||||||||
| Level of awareness of occupational health and safety | High Level awareness of occupational health and safety | 48 | 40 | 37 | 1.532a | 4 | 0.820907 | Not significant |
| 48.5% | 54.1% | 48.7% | ||||||
| Moderate Level awareness ofoccupational health and safety | 33 | 25 | 48.7% | |||||
| 33.3% | 33.8% | 36.8% | ||||||
| Low level awareness of occupational health and safety | 18 | 9 | 11 | |||||
| 18.2% | 12.2% | 14.5% | ||||||
| Levels of Compliance to Safety regulations in association with individual level factors | ||||||||
| Individual level influencing factors | High Level of Individual associated factors | 41 | 29 | 35 | 5.571a | 4 | 0.233592 | Not significant |
| 41.4% | 39.2% | 46.1% | ||||||
| Moderate Level of individual associated factors | 34 | 33 | 32 | |||||
| 34.3% | 44.6% | 42.1% | ||||||
| Low level of individual associated factors | 24 | 12 | 9 | |||||
| 24.2% | 16.2% | 11.8% | ||||||
| Levels of Compliance to Safety regulations in association with strategies for hazards prevention in hospital | ||||||||
| Strategies for Hazards prevention in hospital | High Level of hazard Prevention strategies | 48 | 33 | 19 | 11.560a | 4 | 0.020939 | Significant |
| 48.5% | 44.6% | 25.0% | ||||||
| Moderate Level of hazard Prevention strategies | 30 | 28 | 35 | |||||
| 30.3% | 37.8% | 46.1% | ||||||
| Low level category of Hazard prevention strategies | 21 | 13 | 22 | |||||
| 21.2% | 17.6% | 28.9% | ||||||
| Levels of Compliance to Safety regulations in association with health facility safety programs | ||||||||
| Health Facility Safety Programs | High Level of hospital health safety programs | 43 | 27 | 11 | 20.478a | 4 | 0.000402 | Significant |
| Moderate Level of hospital health safety programs | 43 | 31 | 40 | |||||
| 43.4% | 41.9% | 52.6% | ||||||
| Low level of hospital health safety programs | 13 | 16 | 25 | |||||
| 13.1% | 21.6% | 32.9% | ||||||
| Levels of Compliance to Safety regulations in association with Employees Participation on safety | ||||||||
| Employees Participation on safety | High Level participation of employee on hospital safety program | 45 | 28 | 8 | 25.653a | 4 | 0.000 | Significant |
| 45.5% | 37.8% | 10.5% | ||||||
| Moderate level employees on safety program | 34 | 27 | 39 | |||||
| 34.3% | 36.5% | 51.3% | ||||||
| Low level Employee participation on safety | 20 | 19 | 29 | |||||
| 20.2% | 25.7% | 38.2% | ||||||
Table 2: Distribution of the relationship between Compliance to safety regulations and health facility factors associated with occupational hazards and other variables at level of 0.05 significant difference of p-value.
Workplace safety compliance from policy review and focus group discussion showed absence of strictly adhered to incident investigations, report and follow up evidence, Training gap/ information sharing and safety warnings. Others are poor equipment maintenance/engineering, fire drill, communication system and emergency intervention plan. A lot of challenges with hospital waste management practices (Table 3).
| Strategic objectives | Achievement status | Existing Gap/ Challenges | Action plan |
|---|---|---|---|
| Policy provides operational guidance on Negative Incident Reporting, | The three health Facilities in Kigali, have adopted the policy, they have hospital health and hygiene committee who have the mandate to address incident cases | ILO and WHO clearly provides a guideline frame work on how to handle safety and hazards related events in workplace. Unfortunately, there are absence of evidence based practices and incident report |
The safety and hygiene committee need to be fully functioning in line with guideline and with evidence based result. Inaugurating the safety committee is not enough but a functional and active committee, with an evidence based documented proof of activities. |
| Incident Investigation, | Only a fraction of incident cases were investigated to ensure quality assurance, equity in services and risk reduction | There are few incident investigations carried out but no report of the activities or ILO and WHO clearly provides a guideline frame work on how to handle safety and hazards related events in workplace. Unfortunately, there are absence of evidence based practices and report |
Regular review of incident cases put down strategies for prevention of future occurrence and regular report and updated information and research in relation to occupational health and safety. |
| Reporting and Handling of Accidents/Injuries While on Duty | Injection safety strategies, pre- exposure and post exposure treatment and mitigation strategies are fully in practice | Training gap/ information sharing and evaluation | Regular safety and hygiene incident review and evaluation to identify gap, for improvement |
| No Smoking of Tobacco Products on Hospital Premises and Taking Alcohol, Abuse of Drugs and Other Substances in District Hospitals | Smoking information and warning exist. Also restriction for health personnel to avoid risk to self and others |
But not fully enforced, reported and communicated to attract the desired behaviour change | Enforcing policy and disease prevention especially to prevent secondary smoking effect |
| Manual Handling (Lifting of Loads) | Not yet addressed due to poor finance | Participant response of confirms the burden of manual handling and lifting | The need to ensure evidence based insurance cover for treatment and hazard mitigation strategies. |
| Storage and Labeling on Flammable Products, Storage of Hazardous Materials and Dangerous Goods, Purchase of Hazardous Materials and Dangerous Goods |
Strict purchase operation mechanism exist and proper labelling | But storage and disposal mechanism are not in line with the policy guide especially for hazardous chemicals | May need to consult experts to help out to reduce the environmental and human contamination |
| Radio and Other Noise Making Devices in Hospital Settings | Strict control measures are fully in place and enforced | No report of incident | Need to keep surveillance and improved communication |
| Fire Extinguishers Use | Fire mitigation strategies are designed, but not yet fully addressed | The fire extinguisher though exist but no form of training, fire drill, communication system and emergency intervention plan | Experts services may be employed to mitigate incidents |
| Monitoring Data on Incidents, Injuries and other Events | Great majority of the health practices are carried out without regards to the guidelines | Weak monitoring, investigation, follow up and absence of incident reports | Improvement through: Training, investing and improvement reporting and research |
| Hazards and Risk reduction | Little activity | Workplace environmental safety are not enforced, Poor equipment maintenance, engineering, poor supply of PPE that are necessary to prevent hazards | Fund mobilization, improved communication, proper job placement, training, job supervision and motivation |
| Handling Storage and Disposal of Clinical and other Waste | Contract manager with little experience | No safety guidelines for activities in various departments, Absence of job supervision and evaluation update. The forum for dealing with challenges in waste management | Programs for improved waste management |
| Safety committee and responsibilities | There are evidence of existence of the safety and hygiene committee in the three health institution | Workers involvement in decision making and a lot of other safety issues. |
Table 4: Summary of Policy Implementation and Compliance Gap Analysis.
A multi-nominal regression analysis showed statistical relationship with Factor resulting to Poor policy enforcement (0.000<0.05) and Hazards reports systems (0.012<0.05). Also significant is Individual level influencing factors to occupational health hazards (0.024<0.05) and health factors influencing factors to occupational hazards (0.018<0.05) (Table 4).
| Levels of Compliance to Safety regulations | B | Std. Error | d. f. | Sig. | Exp(B) | 95% Confidence Interval for Exp(B) | ||
|---|---|---|---|---|---|---|---|---|
| Lower Bound | Upper Bound | |||||||
| Level compliance Safety regulations |
Intercept | -0.779 | 1.161 | 1 | 0.503 | |||
| Hazard Knowledge | 0.190 | 0.239 | 1 | 0.426 | 1.209 | 0.757 | 1.930 | |
| Hospital Management policy commitment | -0.432 | 0.247 | 1 | 0.080 | 0.649 | 0.400 | 1.054 | |
| Respondents opinion of workplace hazards | -0.250 | 0.239 | 1 | 0.295 | 0.779 | 0.488 | 1.243 | |
| Types of Hazard cases | 0.123 | 0.235 | 1 | 0.602 | 1.131 | 0.713 | 1.793 | |
| Factor resulting to Poor policy enforcement | 0.904 | 0.233 | 1 | 0.000 | 2.470 | 1.564 | 3.902 | |
| Hospital hazards Prevention strategies | -0.403 | 0.240 | 1 | 0.094 | 0.668 | 0.417 | 1.070 | |
| Hazards reports systems | 0.484 | 0.192 | 1 | 0.012 | 1.622 | 1.113 | 2.363 | |
| Individual level influencing factors | -1.045 | 0.465 | 1 | 0.024 | 0.352 | 0.141 | 0.874 | |
| Health Facility influencing factors | 1.102 | 0.467 | 1 | 0.018 | 3.009 | 1.205 | 7.514 | |
Note: The reference category is: Low level compliance.
Table 4: Distribution of multi-nominal regression analysis of variables influencing Levels of Compliance to Safety regulations.
Discussion
Compliances to safety standards adopted for the protection of health workers based on policy guidelines in hospitals in Kigali Rwanda; found that high number of study participants are practicing hand washing after any direct contact with Patient and safe collection and disposal of sharps equipment’s. Another high frequencies of the participants confirmed use of gloves for contact with body fluids, non-intact skin and mucous andcorrect disposal of used personal protective equipment safely. In the area of compliance to universal post exposure precautions, with regards to careful handling and disposing of sharp instruments during and after procedures the study also found high compliance rate to immediate washing of hands and other skin surfaces after contact with blood.
On the other hand, the study equally found low compliance to the re- evaluation of exposed health care workers within 72 hours just like study by [19] on the Access to occupational post-exposure prophylaxis for primary health care workers in rural Africa showed higher mean knowledge and confidence scores but no different mean attitude scores than those who did not. (P=0.008) than for those who did not (8.8 of 12). Findings from employee participation on safety committee were average, about 168 (67%, 95% C.I=61.27-73.25), just like existence of written statements, goals, contracts languages other document describing functions, duties and authorities of health and safety committee about 154 (61.8%, 95% C.I=of 55.50-67.91).
It is important to know that about 137 (55%, 95% C.I=48.61-61.31) disagreed that hospital safety committee meets consistently at a regular schedule time and place. While, about 141 (56.6%, 95% C.I=48.61-61.31) responses showed absence of investigations/ analyses for all accidents resulting in injury, regardless of how minor they may be or reported. The summary picture on how the respondents rated hospital management commitment and leadership to Policy guidelines, a mean index for all aspects was rated and computed which were equal to (mean=2.9283). These results indicated moderate level of hospital management commitment to occupational safety Policy guidelines.
The study also found four major study variables that have positive association with compliance practices including; Health facility associated factors (0.049; P<0.05), Hazards prevention strategies in hospital (0.02; P<0.05), Health Facility Safety Programs (0.000; P<0.05) and Employees Participation on safety (0.020; P<0.05). This finding is in line with [20] study that tried to establish employees’ perception on occupational health and safety at Eapcc, further determine the extent to which workers had complied with the OSHA 2007 stipulations. The regression results show that there was significant relationship between occupation health concerns and employees performance (r=-0.925, p=0.001) and a negative but significant relationship between occupational safety concerns and performance of employees (r=-0.777, P=0.002). Another study on compliance to safety by [21] in Nairobi on the Extent of Compliance with Occupational Safety and Health Regulations at Registered Workplaces in Nairobi. The Overall, the extent of compliance with the Act at workplace stood at 64.49%.
It is good to know that the Government of Rwanda adopted the health facility accreditation system among many strategies to improve quality of care, to foster continuous quality in Health facilities and with elaborated policies, procedures and guidelines to be followed in service delivery. The study however, found were evidence of low compliance to incident investigations, report and follow up. There were safety information sharing and training evaluation records gaps. Workplace environmental safeties are not fully enforced as recommended in the policy. The study also found that there were a lot of challenges the health facilities faced in dealing with medical waste management. It is pertinent that attention is given to it based on the policy guide especially for hazardous chemicals. However, the safety committee and responsibilities were just recently inaugurated and are yet to come to terms with safety issues that exist.
Focus group discussion findings brought out issues related to work overtime, absence of motivation and leave due to shortage of staff. Also poor investigation, follow up and report of workplace incident cases. There are no guidelines on risk aversions and procurement procedures for equipment’s replacement or training and safety information and practice guides. The waste management companies have no real program and develop rules on recovery and disposal of the waste. The policy and procedure for medical waste management decontamination and recycling are not fully implemented.
The study confirmed the existence of a written policy supporting and mandating the safety and effective communication system, based on the information from high number of hospital management staff, about 6 out of 9 management staff of the three health facilities (66.7%, 95% C.I=29.93-92.51). On the other hand a very low number of the management staff, 3 out of the 9 (33.3%, 95% C.I=07.49-70.07) agreed that everyone in the hospital knows who has been assigned responsibility for the program and recognizes employee contributions to worker safety and health at the hospital.
A multi-nominal regression analysis strongly confirmed the following as the main variables that influences compliance to safety practices in the study: poor policy enforcement (0.000; P<0.05), hazards reports systems (0.012; P<0.05), Individual level associated factors (0.024; P<0.05) and lastly health level associated factors (0.018; P<0.05).
Based on the study findings as stated above, it is obvious that both the employers and the employees in the health facilities are strongly implicated with poor compliance to health and safety regulations. The findings from the policy gap review showed that the ILO and WHO safety and hazards control in workplace were not strictly adhered as indicated above. Even focus group discussion findings showed similar findings and related issues. These findings are comparable to other related studies conducted in the Sub Saharan African.
The study was done in a district health facility and findings cannot be generalized to the primary health care system in Rwanda, and the very few non response rates that may affect the study outcome interpretation which might weakness the study. However, But the study tried to overcome information bias through use of broad data collection instrument and is well able to supply the needed information in area of occupational health hazards and safety compliance related issue in Rwanda and resource constraint context.
In conclusion, this study observed low compliance level with occupational health and safety policy in relation to employee participation in safety program, post exposure safety compliance, hospital management leadership commitment. This finding was influenced by Health facility related associated factors, factors related to hazards prevention strategies in hospital. Other factors that contributed to low compliances include health facility safety programs and employees participation on safety. In addition are issues related to poor policy enforcement and hazards reports systems as well as issues related to individual level related associated factors.
Though, Government of Rwanda adopted the health facility accreditation system as one of the many strategies to improve quality of care. There are still low compliance to incident investigations report and follow up, training gap/ safety information sharing and job supervision lapses. There were absence of evidence based practices in relation to waste management and evaluation update on investigations on safety related issues and poor documentation of event. The government can do a lot by addressing issues related to safety information communication, training and job supervision and an establishment of a surveillance system for registering, reporting and management of occupational exposure. Adopt a more effective design of medical waste disposal and a more inclusive involvement of employees in safety and hazards prevention programs.
Key Points
• There are many short falls with compliances to workplace safety for both the employers and the employees which affect their health negatively and the quality of care.
• Occupational health and safety study like this would most likely provide moral, legal and economic benefits to the society, when proper lesson are drawn.
• Adherence to set standards and guidelines in workplace not only promotes safety but prevents disability, economic loss, meet job demand and with quality assurance.
References
- Jagger J, De Carli G, Perry J, Puro V, Ippolito G (2003) Occupational exposure to bloodborne pathogens: epidemiology and prevention. In: Wenzel RP, editor. Prevention and control of nosocomial infections. 4th edn. Philadelphia: Lippincott Williams & Wilkins Publication Ltd, USA.
- Arocena P, Nunez I (2009) The effect of occupational safety legislation in preventing accidents at work: Traditional versus advanced manufacturing industries. Environment and Planning C 27: 159-174.
- Joan B (2010) WHO Healthy workplace framework and model: Background supporting literature and practices. Geneva: WHO Headquarters.
- Faragher EB, Cass M, Cooper CL (2005) The relationship between job satisfaction and health: A meta-analysis. Occup Environ Med 62: 105-112.
- Fleming M, Buchan D (2002) Best Practice Quick Guide Risk Perception Management. National Safety Council 800: 621-719.
- Kassin S, Steven F, Markus HR, Saul M (2011) Social psychology. 8th edn. Cengage Learning Publication Ltd, California, USA.
- Annalee Y, Karen L, Ray C, Mickey K, Marc Corbiere E (2007) Determinants of Healthcare Workers’ Compliance with Infection Control Procedures Healthcare Quarterly 10: 44-52.
- Ford MT, Tetrick LE (2011) Relations among occupational hazards, attitudes, and safety performance. J Occup Health Psychol 16: 48-66.
- Hambach R, Mairiaux P, Francois G, Braeckman L (2011) Worker’s perception of chemical risks: A focus group study. Risk Analysis 31: 335-342.
- Real K (2008) Information seeking and work place safety: A field application of at risk perception attitude framework. Journal of Applied Communication Research 36: 339-359.
- Cooper D (2003) Psychology risk & safety: Understanding how personality & perception can influence risk taking. Professional Safety 48: 39-46.
- Harding CM, Eiser JR (1984) Characterizing the perceived benefits of some health issues. Risk Analysis 4: 131-141.
- Irene H, Jettinghoff K, Cedillo L (2007) Raising awareness of stress at work in developing countries: A modern hazard in a traditional working environment: Advice to employers and worker representatives. Protecting Workers’ Health, Series no. 6. Geneva: World Health Organization.
- Mcleroy KR, Bibeau D, Steckler A, Glanz K (1988) An ecological perspective on health promotion programs. Health Education Quarterly 15: 351-377.
- Shimizu HE, Ciampone MH (2004) The representations of nursing auxiliaries and technicians about team work at an intensive-care unit. RevLat Am Enfermagem 12: 623-630.
- Elmarie B (2006) The development of a model for an employee wellness programme for a fast moving consumer goods organisation. Unpublished Thesis, Pretoria, University of Pretoria.
- International Labour Organization (1981) Rwanda occupational health and safety policy for hospital practice. Occupational Safety and Health Convention 155: 56-70.
- Tejada JJ, Punzalan JR (2012) On the Misuse of Slovin’s Formula. The Philippine Statistician 61: 590-592.
- Baets AJ, Sifovo S, Pazvakavambwa IE (2007) Access to occupational post-exposure prophylaxis for primary health care workers in rural Africa: a cross-sectional study. Am J Infect Control 35: 545-551.
- Mailu JM (2016) Establishing Employees Perception on Occupational Health and Safety concerns at East African Portland cement: Occupational Safety and Health. Master’s Thesis. Nairobi: Jomo Kenyatta University of Agriculture and Technology.
- Stephen NM, Nzuve Ayub BL (2012) The Extent of Compliance with Occupational Safety and Health Regulations at Registered Workplaces in Nairobi. International Journal of Business, Humanities and Technology 7: 161-167.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences