ISSN : 2576-392X
Dentistry and Craniofacial Research
Surgical Orthodontic Treatment for a Skeletal Class III Young Patient with Tongue Thrust Habit
Montesinos Armando F1*, Benitez César1 and Ramirez Lugo Oscar2
1Department of Orthodontics, Post-Graduate Studies and Research Division, Odontology Faculty, National Autonomous University of Mexico, Mexico
2Department of Maxillofacial Surgery, Post-Graduate Studies and Research Division, Odontology Faculty, National Autonomous University of Mexico, Mexico
- *Corresponding Author:
- Armando Montesinos F
Department of Orthodontics Post-Graduate Studies and Research Division
Odontology Faculty, National Autonomous University of Mexico
Circuito Institutos S/N Ciudad Universitaria
Colonia Copilco Universidad, Delegación Coyoacán
México Distrito Federal, C.P. 04510
Mexico
Tel: 525555542429
E-mail: amfortod_@hotmail.com
Received date: September 15, 2016; Accepted date: May 19, 2017; Published date: May 28, 2017
Citation: Armando MF , Cesar B, Oscar RL. Surgical Orthodontic Treatment for a Skeletal Class III Young Patient with Tongue Thrust Habit. J Den Craniofac Res. Vol.2 No.2:7. doi: 10.21767/2576-392X.100007
Abstract
This article describes the treatment of a skeletal Class III patient with a severe anterior cross-bite, open-bite, crowding and a tongue thrust habit. Two treatment options were proposed: -conventional orthodontics to camouflage the skeletal anomaly and traditional orthodontics/orthognathic surgery approach. The surgical orthodontic approach was selected, but treatment was started 3 years 8 months from the treatment plan presentation appointment. Surgery was scheduled when pre-surgical orthodontics was finished; a Le Fort I osteotomy was performed for maxilla advancement and a bilateral sagital split osteotomy (BSSO) for mandibular setback. Post-surgical orthodontics was applied for finishing and detailing the occlusion. Total treatment time was 24 months. Good facial balance and occlusal relationships were achieved.
Keywords
Surgical orthodontic treatment; Orthognathic surgery; Pre-surgical orthodontics; Post-surgical orthodontics; Tongue trust habit; Skeletal class III; Openbite; Anterior cross-bite.
Introduction
The primary concern of many patients who seek orthodontic treatment is aesthetics and not for correction of functional disability although there is a severe one. Facial and dental aesthetics affect how people are perceived by society and how they see themselves [1]. Low self-esteem and quality of life is related to dentofacial deformity [2]. Social embarrassment, eating problems, discomfort and bullying are some of the issues patients experience as a result of dentofacial deformity [3,4]. In adolescents and young adults can be a tough time to endure if dentofacial deformity is present and it can lead to depression interfering significantly in vitality, social aspects of the individual and mental health [5]. Adolescents and young adults with dentofacial deformity want to start treatment as soon as possible, so teasing related to their appearance can stop.
Case Report
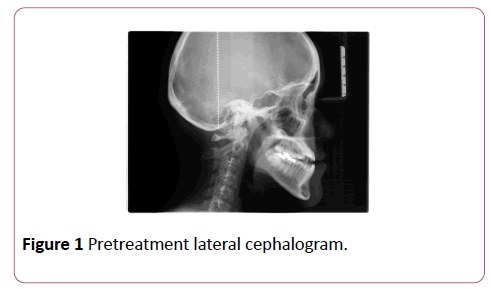
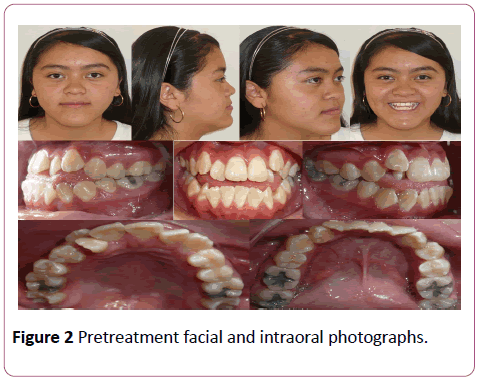
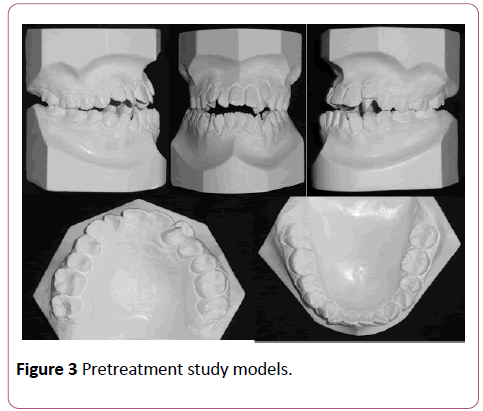
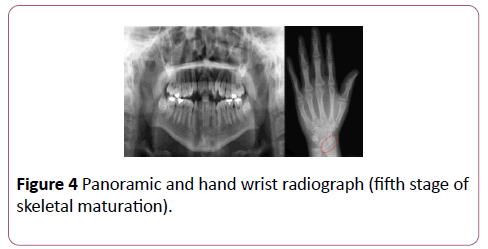
A female patient came to the University orthodontic department with chief complaint of a severe anterior openbite and cross-bite, the patient was 13 years and 10 months old with a healthy medical history. A tongue thrust habit was detected, pretreatment records showed a Class III skeletal relation, proclined upper and retroclined lower incisors (Figure 1 and Table 1). Dental findings showed an Angle Class III malocclusion, anterior cross-bite of -3 mm, -4 mm open-bite, severe upper anterior and moderate lower crowding (Figures 2 and 3). Hand wrist radiograph showed a fifth stage of skeletal maturation, the panoramic radiograph showed diminished root length of the upper incisors, lack of roots parallelism and presence of all third molars (Figure 4).
| Measurement | Norm | Pre-treatment | Post-treatment |
|---|---|---|---|
| SNA | 82° | 85° | 93° |
| SNB | 80° | 98° | 90° |
| ANB | 2° | -13° | 3° |
| Go Gn-SN | 32° | 30° | 30° |
| 1-1 | 130° | 141° | 135° |
| 1-SN | 102° | 125° | 108° |
| IMPA | 90° | 82° | 90° |
Table 1: Cephalometric measurements.
Treatment objectives
The treatment objectives were to
• Achieve better facial balance
• Eliminate the tongue thrust habit
• Correct anterior cross-bite
• Correct open-bite
• Obtain a functional dental relationship
• Maintain the root length of the teeth (Especially upper incisors)
Treatment alternatives
The first treatment option was a conservative camouflage of the skeletal anomaly non-surgical approach: upper and lower first bicuspids extractions to relieve crowding and stripping of the lower incisors or a central lower incisor extraction could eliminate the anterior cross-bite.
It was explained that the future integrity of the periodontal tissue of the lower incisors could be compromised when a patient with a skeletal problem is compensated by dental extractions. The second option was a traditional surgical orthodontic approach: a pre-surgical orthodontic phase to level and align, relieve dental compensations by extracting upper first bicuspids and coordinate the dental arches; the surgical procedure of maxilla advancement and mandibular setback; then post-surgical orthodontic phase for detailing the occlusion. It was explained to the parents that the pre-surgical orthodontics could be started, but the orthognathic surgery could only be performed once the skeletal growth had finished (patient was 13 years and 10 months old, and fifth stage of skeletal maturation). The surgical orthodontic approach was the treatment protocol selected.
Treatment progress
The parents decided not to start treatment and save money for the surgical procedure. Three years and 8 months later they returned to the clinic; patient was 17 years and 6 months old and started treatment. The upper first bicuspids and third molars extractions were prescribed. MBT 0.022” × 0.028” appliance (3M Unitek, Monrovia, CA.) was bonded from second molar to second molar upper and lower.
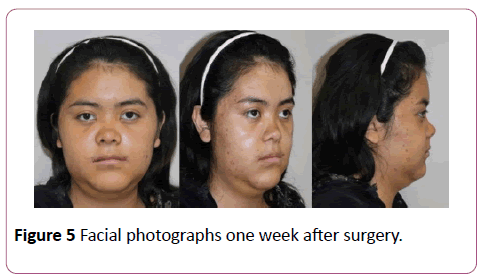
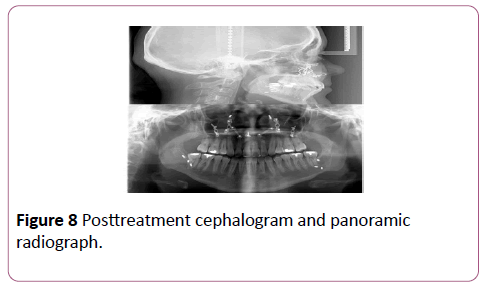
Tongue trust habit correction exercises were prescribed and an in posterior appointment spurs were bonded to upper anterior teeth. The following archwires were used in posterior appointments for one month: Niti 0.012”, 0.014”, 0.016”, 0.016” × 0.022”, 0.017” × 0.025”, 0.019” × 0.0.25”, SS 0.019” × 0.025” upper and lower; an open coil was placed in the upper archwire to create space for the upper left lateral incisor and progressively was tied until complete alignment. The retraction phase in the upper arch was completed with SS 0.019” × 0.025” and tie-backs; pre-surgical orthodontics was finished and the orthognathic surgery was scheduled. A Le Fort I osteotomy was performed to advance the maxilla 5 mm, a bilateral sagital split osteotomy (BSSO) was performed for mandibular setback of 5 mm and rigid fixation was used. The maxillofacial surgeon checked the recovery of the patient each week and three weeks later an orthodontic appointment was scheduled to start the post-surgical phase (Figure 5). A panoramic radiograph was taken to check root alignment and bracket repositioning, NitiCu 0.016” × 0.022” upper and lower archwires were engaged followed by NitiCu 0.019” × 0.025” and SS 0.019” × 0.025” for finishing and detailing. The retention protocol was upper and lower circumferential retainers 24 hours a day.
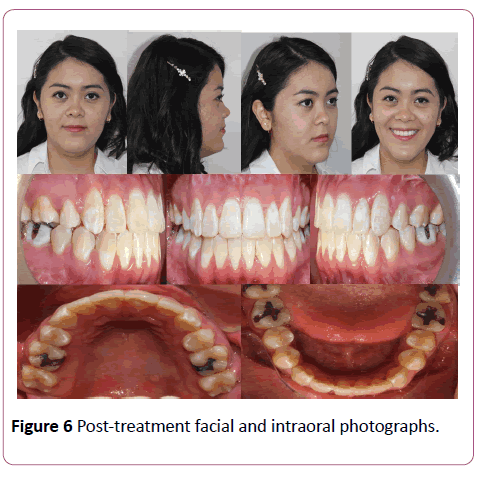
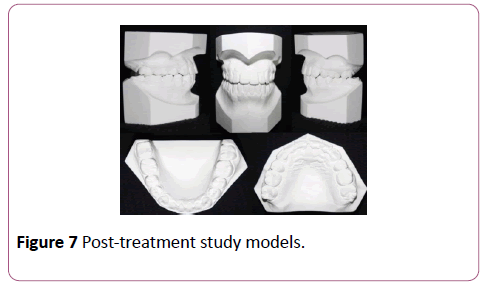
Treatment results
All treatment objectives were achieved, Facial balance was improved and the occlusal relationships were very good. The patient was excited and happy with the new facial appearance and beautiful smile; the masticatory function was also improved (Figures 6 and 7). Panoramic film showed good root parallelism and root length was maintained (Figure 8). Overall active treatment time was 24 months.
Discussion
The concept that surgical correction of dentofacial deformities have both physical and psychological impact on quality of life and concluded in their study significant improvement on it [6], the psychological factors and aesthetics exert a strong influence on the patient´s quality of life, and determine major changes more than functional aspects do [7]. Conventional surgical orthodontic treatment requires three stages: 1. The pre-surgical orthodontics phase to level and align, eliminate dental compensations, and coordinate de arches [2]. The surgical phase in which the planned orthognathic surgery at treatment planning is performed [3]. The post-surgical orthodontic phase to detail the occlusion. Masticatory discomfort and worsening of facial aesthetics after relieving dental compensations are a burden that may decrease the already diminished patient´s quality of life as a result of dentofacial deformity [8]. This first stage in surgical orthodontics can be a burden and patients can really suffer bullying with devastating effects, especially in young adults; but well-motivated patients can endure this stage because of the expected results. One of the most important benefits of the “Surgery First” approach in orthognathic surgery is the immediate correction of the dentofacial deformity [7], this is an important advantage over the traditional approach but not all patients can choose this alternative, some of them due to economic issues therefore they have to save for the surgery costs.
Skeletal deformity in conjunction with abnormal size or function of the tongue can be a real challenge for the orthosurgical team; the correction in all space planes by the specialists and tongue trust control must be executed to break the habit since the beginning of treatment. It has been reported that tongue position or activity are reasons for difficulty in achieving long-term stability in open-bite treatment [9-10]. Lingual-spur therapy results in closure of the anterior open-bite by successfully keeping tongue pressure away from the anterior teeth and serving as a reminder to the patient to discontinue oral habits [9,11-14].
The surgical orthodontic treatment aesthetic and functional outcomes create high levels of satisfaction in skeletal Class III patients [15-17]. Surgical orthodontic treatment has a significant effect on the oral health related quality of life (OHRQoL) of class II and III patients [18]. The young patient reported in this manuscript was very happy with the functional and aesthetics results, she reported some difficult times in the pre-surgical stage because of the worsening of her appearance but after the surgical stage, she was well-motivated to continue the post-surgical one, “All difficulties and discomfort of treatment was hard, but it was all worth it”, she said.
Conclusions
Pernicious habits such as tongue thrusting must be treated since the beginning of treatment. Traditional surgical orthodontic approach must be carefully planned and efficiently applied. The burden and discomfort of pre-surgical and surgical stages can be well tolerated by well-motivated patients, especially for the aesthetics and functional outcomes.
Ethical Approval and Conflict of Interest
The authors declare that the patient was treated with all ethical approval; the informed consent was explained to the patient who signed. The authors declare no conflict of interest and/or financial interest or support.
References
- Isiekwe GI, Sofola OO, Onigbogi OO, Utomi IL, Sanu OO, et al. (2016) Dental esthetics and oral health-related quality of life in young adults. Am J Orthod Dentofacial Orthop 150: 627-636.
- O'Brien K, Wright J, Conboy F, Appelbe P, Bearn D, et al. (2009) Prospective, multi-center study of the effectiveness of orthodontic/orthognathic surgery care in the United Kingdom. Am J Orthod Dentofacial Orthop 135: 709-714.
- Ryan FS, Barnard M, Cunningham SJ (2012) Impact of dentofacial deformity and motivation for treatment: A qualitative study. Am J Orthod Dentofacial Orthop 141: 734-742.
- Gavric A, Mirceta D, Jakobovic M, Pavlic A, Zrinski MT, et al.(2015) Craniodentofacial characteristics, dental esthetics-related quality of life, and self-esteem. Am J Orthod Dentofacial Orthop 147: 711-718.
- De Ávila ED, de Molon RS, Loffredo LC, Massucato EM, Hochuli-Vieira E (2013) Health-related quality of life and depression in patients with dentofacial deformity. Oral Maxillofac Surg 17:187-191.
- Silva I, Cardemil C, Kashani H, Bazargani F, Tarnow P, et al. (2016) Quality of life in patients undergoing orthognathic surgery: A two-centered Swedish study.J Craniomaxillofac Surg44:973-978.
- Rustemeyer J, Gregersen J (2012) Quality of Life in orthognathic surgery patients: Post-surgical improvements in aesthetics and self-confidence. J Craniomaxillofac Surg40: 400-404.
- Kim JH, Mahdavie NN , Evans CA (2012) Guidelines for “Surgery First” orthodontic treatment.In: Bourzgui F (Ed). Orthodontics-Basic Aspects and Clinical Considerations, IN TECH Rijeka, Croatia. pp 265-300.
- Justus R (2001) Correction of anterior open bite with spurs: Long-term stability. World J Orthod 2:219-231.
- Greenlee GM, Huang GJ, Chen SS, Chen J, Koepsell T, et al.(2011) Stability of treatment for anterior open-bite malocclusion: Ameta-analysis. Am J Orthod Dentofacial Orthop 139: 154-169.
- Canuto LF, Janson G, de Lima NS, de Almeida RR, Cançado RH(2016) Anterior open-bite treatment with bonded Vs conventional lingual spurs: A comparative study. Am J Orthod Dentofacial Orthop 149:847-855.
- Cassis MA, Almeida RR, Janson G, Almeida-Pedrin RR, Almeida MR (2012) Treatment effects of bonded spurs associated with high-pull chincup therapy in the treatment of patients with anterior open bite. Am J Orthod Dentofacial Orthop 142: 487-493.
- Torres FC, Almeida RR, Almeida MR, Almeida-Pedrin RR, Pedrin F, et al. (2006) Anterior open bite treated with a palatal crib and high-pull chin cup therapy. A prospective randomized study. Eur J Orthod 28: 610-617.
- Huang GJ, Justus R, Kennedy DB, Kokich VG (1990) Stability of anterior open bite treated with crib therapy. Angle Orthod60: 17-24.
- Asada K, Motoyoshi M, Tamura T, Nakajima A, Mayahara K, et al. (2015) Satisfaction with orthognathic surgery of skeletal Class III patients. Am J Orthod Dentofacial Orthop. 148:827-837.
- Magro-Filho O, Goiato MC, Oliveira DT, Martins LP, Salazar M, et al. (2015) Evaluation of patients' satisfaction after class III orthognathic surgery. J Clin Diagn Res9: 23-30.
- Dantas JF, Neto JN, de Carvalho SH, Martins IM, de Souza RF, et al. (2015) Satisfaction of skeletal class III patients treated with different types of orthognathic surgery. Int J Oral Maxillofac Surg 44:195-202.
- Baherimoghaddam T, Tabrizi R, Naseri N, Pouzesh A, Oshagh M, et al. (2016) Assessment of the changes in quality of life of patients with class II and III deformities during and after orthodontic-surgical treatment. Int J Oral Maxillofac Surg 45:476-485.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences