Spontaneous Remission of Vogt-Koyanagi-Harada Meningoencephalitis
Nuran Abdullayev1*, Volker Maus1, Victor Neuhaus1, Christoph Kabbasch1, Jan Borggrefe1 and Anastasios Mpotsaris2
1Institute of Diagnostic and Interventional Radiology, University Hospital Cologne, Kerpener Straße 62, 50937 Cologne, Germany
2Clinic for Diagnostic and Interventional Neuroradiology, University Hospital Aachen, Pauwels Straße 30, 52074 Aachen, Germany
- *Corresponding Author:
- Nuran Abdullayev
Institute of Diagnostic and Interventional Radiology
University Hospital Cologne
Kerpener Straße 62, 50937 Cologne, Germany
Tel: +49 221 478-82035
E-mail: nuran.abdullayev@uk-koeln.de
Received date: January 10, 2018; Accepted date: January 16, 2018; Published date: January 24, 2018
Citation: Abdullayev N, Maus V, Neuhaus V, Christoph K, Borggrefe J, et al. Spontaneous remission of Vogt-Koyanagi-Harada Meningoencephalitis. J Clin Radiol Case Rep 2018, Vol.2 No.1:01.
Copyright: © 2018 Abdullayev N, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
We describe a 65-year-old patient with Vogt-Koyanagi-Harada (VKH) syndrome and primary malignant melanoma of the trunk presenting with systemic tumor progress and new contrast-enhancing intracranial lesions without neurological symptoms. While the systemic melanoma disease ultimately was in progress, the correct radiological interpretation of brain lesions as intracranial manifestation of VKH was mandatory to prevent the patient from unnecessary whole brain radiotherapy.
Keywords
Vogt-koyanagi-harada; Meningoencephalitis; Cerebral manifestations of VKH; Vitiligo
Case Report
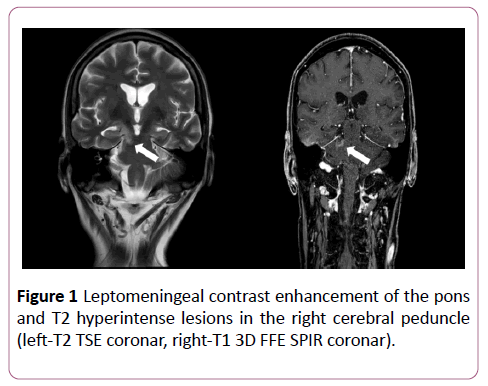
A 65-year-old patient with a 10-year history of VKH disease including vitiligo and uveitis and a 27-year history of primary malignant melanoma of the trunk exhibited histologically proven mediastinal melanoma masses (BRAF V600E-Mutation, American Joint Committee on Cancer stage IV) during followup. Initial brain MRI was normal. Treatment with BRAF and MEK inhibitors was initiated with partial response in the 2- months chest and abdominal CT control-scan. Brain MRI control-scan revealed new leptomeningeal contrast enhancement of the pons and T2 hyperintense lesions in the right cerebral peduncle without neurological symptoms (Figure 1)
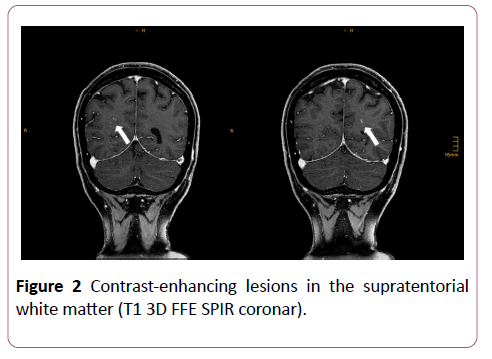
Treatment of melanoma remained unchanged and further control-MRI of the brain after 2 months showed absence of contrast enhancement with regressive T2 lesions. New contrast-enhancing lesions were present in the supratentorial white matter (Figure 2).
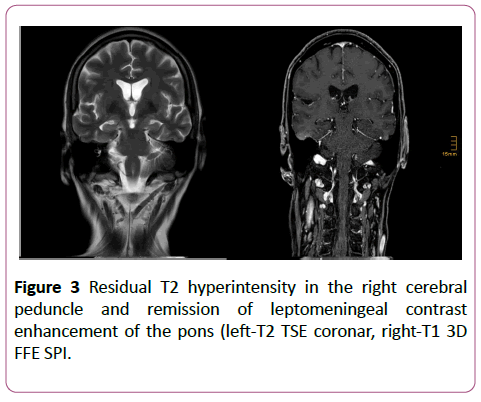
Mediastinal melanoma masses showed remission on CT. Morphological findings and clinical course were deemed atypical for brain melanoma metastasis and accepted as cerebral manifestation of VKH syndrome. Probatory steroid therapy was recommended, but rejected by the patient. Nevertheless, a further 3-months control-MRI of the brain demonstrated complete remission of all contrast-enhancing lesions and slight residual T2 hyperintensity in the cerebral peduncle (Figure 3). Melanoma metastases were dramatically progressive on CT during unchanged therapeutic regimen.
Discussion
VKH syndrome is a granulomatous inflammatory disorder mainly affecting tissues containing pigmented cells (ocular, auditory, integumentary). Patients often present with vitiligo, alopecia, auditory signs, and meningeal irritation [1]. Th1 and Th17 CD4+ lymphocytes seem to play a pivotal role in the pathogenesis of VKH disease [2].
The natural history can be divided into 4 stages: prodromal, acute-uveitic, chronic, and chronic recurrent and is characterized by bilateral uveitis with multifocal retinal detachment and iridocyclitis. The involvement of the central nervous system is rare and may be associated with focal neurological signs [3].
Neuroimaging (MRI) is mandatory to confirm intracranial manifestation of VKH, although abnormal MRI findings have been reported in a few cases only. Early reports described diffuse leptomeningeal contrast enhancement and T2-bright periventricular lesions, while more recent ones described lesions within the brain stem and peduncle as well as pachymeningeal enhancement [4,5].
We here present a patient with progressive malignant melanoma and VKH syndrome exhibiting multiple new contrast-enhancing cerebral lesions and leptomeningeal enhancement with spontaneous remission. Interestingly, our patient showed a very late onset of leptomeningeal involvement without neurological symptoms, although abnormal signal changes and pathologic contrastenhancement were located in the right cerebral peduncle. Hashimoto et al. described similar changes mainly in the posterior fossa as preferred localization [6].
In the present case, the opposed systemic course of the progressive melanoma disease under continuous immunotherapy in contrast to the initially new-onset intracranial lesions, that finally resolved spontaneously, led to the correct interpretation of these findings. In conclusion, cerebral manifestations of VKH in patients with primary malignant melanoma have to be delimited from melanoma metastasis as misinterpretation of clinical and MRI findings may lead to erroneous treatment, e.g., whole brain radiotherapy.
Conflict of Interest
The authors declare no conflict of interests.
References
- Read RW, Holland GN, Rao NA, Tabbara KF, Ohno S, et al. (2001) Revised diagnostic criteria for Vogt-Koyanagi-Harada disease: report of an international committee on nomenclature. American Journal of Ophthalmology 131: 647-652.
- Moorthy RS, Inomata H, Rao NA (1995) Vogt-koyanagi-harada syndrome. Survey of Ophthalmology 39: 265-292.
- Nitta E, Takamori M (1989) Wallenberg's syndrome in a case of Vogt-Koyanagi-Harada disease. Rinsho Shinkeigaku Clinical Neurology: 29: 505-508.
- Lohman BD, Gustafson CA, McKinney AM, Sarikaya B, Silbert SC (2011) MR imaging of Vogt-Koyanagi-Harada syndrome with leptomeningeal enhancement. American Journal of Neuroradiology 32: E169-E171.
- Han HJ, Kim HY, Park JH, Lee EJ, Kim DG, et al. (2010) Magnetic resonance imaging of pachymeningeal enhancement in Vogt-Koyanagi-Harada disease. Neurological Sciences 31: 785-788.
- Hashimoto T, Takizawa H, Yukimura K, Ohta K (2009) Vogt-Koyanagi-Harada disease associated with brainstem encephalitis. Journal of Clinical Neuroscience 16: 593-595.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences