Prognostic Factors of Renal Impairment in Multiple Myeloma in Senegal
1Nephrology Department, Aristide le Dantec Hospital, Dakar, Senegal
2Nephrology Department, Renaissance Hospital, N'Djamena, Chad, Central Africa
3Nephrology Department, General Hospital, National Reference of N’Djamena, Tchad, Central Africa
- *Corresponding Author:
- Guillaume MA
Nephrology Department, Renaissance Hospital, N'Djamena
Chad, Central Africa
Tel: 0023566619595
Email: zalba2001@yahoo.fr
Received date: July 07, 2018; Accepted date: August 20, 2017; Published date: August 27, 2018
Citation: Moustapha M, Guillaume MA, Fall K, Tall A, Faye A, et al. (2018) Prognostic Factors of Renal Impairment in Multiple Myeloma in Senegal. J Nephrol Urol. Vol.2 No.1:12.
Copyright: © 2018 Moustapha M, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
Introduction: The occurrence of renal impairment in multiple myeloma is a major turning point in the evolution of this incurable malignant hemopathy. This is the main prognostic factor and more and more authors report its major impact on the long-term overall survival of these patients. The aim of this study was to describe the prognosis and to determine the prognostic factors of renal involvement in multiple myeloma in Senegal.
Patients and method: This was a multicenter, retrospective descriptive and analytical study lasting 7 years, involving 133 patients with renal impairment during follow-up. Predictive factors, prognosis and treatment outcome of hematologic and renal response were studied at 3 months, 6 months and 1 year of follow-up.
Results: One-year survival was observed in 17% of patients. It was conditioned by renal prognosis, hyperbeta2- microglobulinemia and anaemia. Renal prognosis was negatively influenced by hyperprotidemia, proteinuria and advanced age. Patients treated with Velcade, who were adjusted for other drugs, had better recovery of renal function. Predictors of kidney damage were age, gender, high blood pressure, diabetes, NSAIDs, exposure to toxic products, taking herbal medicine. Finally, anaemia and hyperbeta2-microglobulinemia were associated with a higher occurrence of death.
Conclusion: The prognosis of renal involvement in multiple myeloma in Senegal is still poor and in addition to the prognostic factors reported in the literature, the inaccessibility to chemotherapy last generation is the challenge to improve this prognosis.
Keywords
Multiple myeloma; Renal impairment; Prognostic factors; Senegal
Abbreviations
EPO: Erythropoietin; CSH: Hematopoietic Stem Cells; IRA: Acute Renal Failure; DFG: Glomerular Filtration Rate; NSAIDs: Nonsteroidal Anti-inflammatory Drug; CKD: Chronic Renal Failure; NFS: Blood Count; ESP: Electrophoresis of Seric Proteins; eGFR: Estimated Glomerular Filtration Rate.
Introduction
Multiple myeloma is the most common dysglobulinemia. It is defined by a plasmocytosis >10% with or without CRAB criteria such as anemia, hypercalcemia, renal failure, and the presence of bone lesions [1]. It is an incurable hematological malignancy and its gravity is due to its many complications, infectious, neoplastic, hematological (AL amyloidosis), renal and bone often disabling. The prognosis for a long time is evaluated by the classification of Salomon and Durie and the international score. The kidney is the major target of multiple myeloma, nearly 40% of myeloma patients will develop kidney disease and among them 10 to 15% will need dialysis [2,3]. The high incidence of advanced renal impairment at the time of diagnosis has a significant impact on the overall survival of these patients. A Spanish study showed that myeloma patients with ARI had an overall survival of 8.6 months compared to 34.5 months in patients who had never developed ARI in this field [4]. Reversibility of renal function has also been a major survival feature known for more than 20 years because long-term survival is better in those with complete renal recovery compared to those with partial or absent recovery (28 months versus 4 months, p <0.001) [3]. Many prognostic factors for myeloma have already been identified, including age, physical fitness, albuminuria, beta 2 micro globulin, lactate dehydrogenase (LDH), renal function, genetic factors, and free light chains [2,4-6]. However, there is little information regarding the prognosis of renal involvement. Therefore, this study was initiated for the first time in Senegal, the purpose of which was to describe the prognosis and to determine the prognostic factors of renal involvement during multiple myeloma.
Patients and Methods
This was a retrospective, descriptive and analytical study lasting seven years from January 1, 2010 to January 1, 2017. The study was conducted in four Dakar centers, namely the dialysis nephrology service. Renal transplantation and internal medicine department (clinical hematology unit) of the Aristide Le Dantec University Hospital, the National Center for Blood Transfusion (CNTS) and the Pathology Anatomy and Cytology Department of the General Hospital of Grand Yoff. We included all patients with renal impairment related to multiple myeloma diagnosed according to the ISWMG criteria. This renal impairment is defined by the presence of renal insufficiency or proteinuria or active urinary sediment. We excluded incomplete files. The studied parameters were the clinical and biological evolution of the patients, the molecules used for the basic treatment and the hematological and renal response to the chemotherapy, the predictive factors of the renal damage, the factors of severity, the prognostic factors, the death and survival rates as well as factors associated with the occurrence of complications, death, hematologic remission and renal recovery. Survival at 3 months, 6 months and 1 year and associated factors were studied. The renal response to treatment was assessed using IMWG criteria. The prognostic score was evaluated according to Salomon and Durie and the ISS international classification.
Results
In a population of 175 patients with myeloma followed, 133 cases of renal impairment were retained. The average age was 58.07 years old with (40 to 70 years). Twenty-two patients (16.5%) had functional renal failure. The renal biopsy puncture was performed in 59.4% of the patients (n= 79). The diagnoses retained were myeloma tubulopathy (61%), MIDD (Randall type) (3.5%) and untyped amyloidosis (case 1). The other etiologies are indexed in Table 1.
| Diagnosis | Frequency (n=113) | Percentage (%) |
|---|---|---|
| Amyloidosis | 1 | 0.88 |
| Myeloma tubulopathy | 69 | 61.06 |
| Randall Disease | 4 | 3.54 |
| Acute tubular necrosis | 1 | 0.88 |
| Extramembranous glomerulonephritis | 1 | 0.88 |
| Glomerular thrombotic microangiopathy | 1 | 0.88 |
| Minimal glomerular lesion | 1 | 0.88 |
Table 1: Histological data.
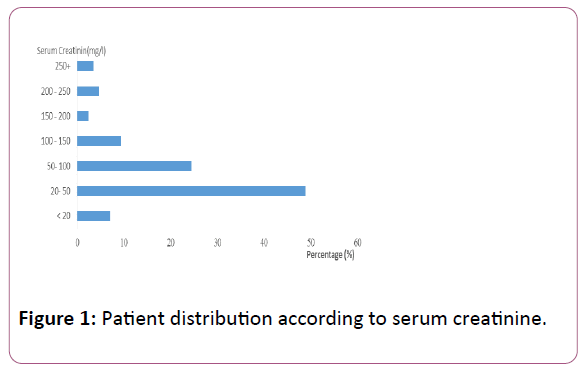
From a biological and prognostic point of view, anemia was present in 77.9% with an average hemoglobin level of 7.54 g/dl with (3.1-13.1 g/dl). Thrombocytopenia and leukopenia accounted for 31.6% and 8.13% respectively. Hypercalcemia was observed in 60.52% of cases, with a mean serum calcium concentration of 117.42 ± 25.46 mg/l. Proteinuria was observed in 50% of patients. There were 62.8% of the patients who had a GFR of less than 30 ml/min/1.73 m2, with an average serum creatinine of 62.49 mg/l. The distribution of patients by serum creatinine is summarized in Figure 1.
The average rate of albuminemia was 20.61 g/l with (9.1-49.8 g/l). Hypoalbuminemia was noted in 56 patients (65.11%). The beta2-microglobulin assay was performed in 23 patients. The average quantitative level was 29.71 mg/l with (1.23-96.46 mg/l). A hyer-beta2-microglobulinemia was noted in 73.9%. The summary of the paraclinical and prognostic characteristics of the study population is summarized in Table 2.
| Characteristics | Included Patients | Percentage (%) |
|---|---|---|
| Anaemia | 175 | 100 |
| Leukopenia | 175 | 100 |
| Thrombocytopenia | 175 | 100 |
| Accelerated sedimentation rate | 23 | 89 |
| Elevated C Reactive Protein | 23 | 58 |
| Impaired renal function | 86 | 49,14 |
| Hypercalcemia | 76 | 43.42 |
| Proteinuria > 0, 5 g/24 h | 49 | |
| Addis account | ||
| Hematuria | 77 | 44 |
| Leucocyturia | 34 | 19.42 |
| Electrophoresis of serum proteins | 175 | 100 |
| Hyperprotidemia | 35 | 20 |
| Hypoalbuminemia | 56 | 32 |
| Gamma-globulinemia peak | 47 | 26.85 |
| Hyper α1-globulinemia | 22 | 12.6 |
| Hyper α2-globulinemia | 33 | 18.86 |
| Myeloma type | 60 | 34.28 |
| Immunoglobulin G | 39 | 65 |
| Immunoglobulin A | 8 | 13.33 |
| Immunoglobulin M | 1 | 1.67 |
| Light chain kappa | 6 | 10 |
| Light chain lambda | 6 | 10 |
| Spinal Plasmacytosis | 69 | 39.43 |
| < 10% | 8 | 11.6 |
| (10-30) | 22 | 33 |
| (30-60) | 16 | 24 |
| > 60% | 14 | 31.3 |
| Renal biopsy | ||
| Tubular damage | 79 | 64.57 |
| Glomerular damage | 70 | 62 |
| Mixed damage | 8 | 7 |
| Hyper ß2-microglobulin | 23 | 73.9 |
| Salmon and Durie stage III | 16 | 92.9 |
Table 2: Summary of paraclinical and prognostic characteristics of the study population.
Therapeutically, 70 patients (81.4%) had been treated with chemotherapy; 62 patients had received the Alexanian protocol (Melphalan-Dexamethazone) among which one patient had relapsed after 10 cures; he had been switched to the VCD protocol for 4 courses (Velcade-Cyclophosphamide- Dexamethazone). Three patients received respectively a VCD protocol, a VD protocol (Velcade-Dexamethasone) and Thalidomide alone. Two patients received the MPT protocol (Melphalan-Prednisone-Thalidomide). One patient had received the VTD protocol (Velcade Thalidomide-Dexamethasone) associated with a CSH transplant. Two other patients were transplanted from CSH. Hemodialysis was necessary in 11% of patients. All patients benefited from transfusion of red blood cell pellets and EPO. Eviction of light chain precipitation factors (NSAIDs, herbal medicine, dehydration and the use of iodinated contrast products) was systematic. Prognostically, in 76 patients, 92.9% of patients were classified as stage III and 17.1% stage II according to Salomon and Durie. The international prognostic index (ISS) was noted in 23 patients; 13 patients were in stage III, 8 patients in stage II and 2 patients in stage I. After 3 months of evolution, 44 patients (51.16%) remained in consultation; 13 patients died (15.11%) and the remaining patients were lost to follow-up. At the renal level, mean serum creatinine in 36 patients (41.86%) was 34.9 mg/l with (6.4-160 mg/l). The average DFG according to MDRD was 43.65 ml/min/1.73 m2 with (4.91-115 ml/min/1.73 m2). Five patients had a complete recovery of renal function; 13 patients, partial recovery and progression to IRC for 18 patients. Thirty-six patients (41.86%) had NFS and serum protein electrophoresis. The average control hemoglobin level was 8.38 g/dl (3.2-13.8 g/dl). Hematologic response was complete in 7 patients, partial in 9 patients, and worse in 20 patients as summarized in Table 3.
| Population after 3 months (n=) | Population after 6 months (n=) | Population after 1 year (n=) | |
|---|---|---|---|
| Hematologic response | |||
| Complete answer | 7 | 2 | 2 |
| Partial anwer | 9 | 19 | 5 |
| Aggravation | 20 | 10 | 8 |
| Renal response | |||
| Complete answer | 5 | 2 | 1 |
| Partial answer | 13 | 5 | 5 |
| CKD evolution | 18 | 19 | 9 |
| Death | 13 | 2 | 9 |
| Lost sight | 29 | 8 | 10 |
Table 3: Summary of the follow-up of our case series.
After one year of evolution, evaluation of renal function was performed in 15 patients (62.5%). Recovery was complete in one patient, and partial in 5 patients. The others patients had progressed to CKD, including 4 in chronic hemodialysis. The death rate was 27.90% (24 patients). Regarding the long-term treatment of myeloma, Alexanian protocol was used in 60% of patients. It associates Melphalan and Prednisone. The other treatments are summarized in the Table 4.
| Treatment | Percentage (%) |
|---|---|
| Symptomatic treatment: Dietary and lifestyle measures |
|
| Water intake according to diuresis and hydration status | 87.2 |
| Stop NSAIDs | 16.3 |
| Stopping the contrast product | 24.4 |
| Stop converting enzyme inhibitors | 14 |
| Drug | |
| Isotonic saline | 53.5 |
| Bisphosphonate | 89.29 |
| Calcitonin | 10.71 |
| Furosemide | 19.64 |
| Antibiotic | 34.88 |
| Analgesic | 54.7 |
| Instrumental | |
| Orthopedic immobilization | 5.81 |
| Dialysis | 12 |
| Background treatment: (70 patients) | |
| Alexanian (Melphalan-Prednisone) | 88.57 |
| MPT (Melphalan-Prednisone-Thalidomide) | 2.85 |
| VCD (Velcade-Cyclophosphamide-Dexamethazone) | 2.85 |
| VD (Velcade-Dexaméthasone) | 1.42 |
| Thalidomide | 1.42 |
| VTD (Velcade-Thalidomide-Dexaméthasone) | 1.42 |
| Bone marrow transplant | 2.85 |
Table 4: Summary of the therapeutic means of our series.
Discussion
Anatomo-clinical forms of renal damage observed in our patients were of good prognosis. But their management was late because of the often lengthy delay between the clinicalbiological and histological diagnosis as well as the effective start of the treatment which sometimes required a specific treatment that did not exist in Senegal. This could explain the fact that 93% of our patients were Solomon and Durie stage III at the time of diagnosis, only 5 patients had a complete hematologic response, and half of the patients had progressed to CKD. In fact, myelomatous cylinder nephropathy (61% of the cases in our series) requires rapid management based on the speed of purification or elimination of the light chains precipitated in the renal tubules as well as the decrease in their circulating rate [4]. This tubulopathy should be avoided with effective prevention of intratubular precipitation of light chains: Avoid contrast agents, avoid nephrotoxic drugs and diuretics and alkalinize urine. With the same idea, Viggiano propose to identify subjects at high risk of CKD progression from urates by analyzing the urinary sediment. Specifically, urinary sediment should be interrogated for the presence of urate crystals, which would demonstrate supra-saturating levels of uric acid in the kidney. However, we did not measure the level of blood uric acid for effective prevention and management [7].
In addition, the non-observance therapeutic, the inaccessibility of the chemotherapies and the lack of means of care could justify, the death of half of our patients, the aggravation of their symptomatology and that they are lost sight of. Finally, anemia is still a real problem for our patients because of the low availability of blood products and the cost of hematopoietic growth factors. Anemia would be an aggravating factor of the ischemia reperfusion phenomenon in distal convoluted tubules secondary to intra tubular precipitation of light chains. Nigro had demonstrated that UCP2 protein deficiency was responsible for proximal tubular lesions, especially if the cause was vascular (hypertensive) [8]. These phenomena could accelerate myelomatous cylinder nephropathy causing renal insufficiency. Hyperbeta2- microglobulinemia was observed in 73.9% with a quantitative determination of 29.71 mg/l. This is similar to the data in the literature. It is an independent prognostic factor, the most significant of all parameters related to the tumor mass, which can be used even in the absence of monoclonal gammopathy [9].
Its prognostic role would be paramount in our incident patients. However, the statistical analysis did not show a significant correlation. It would have been judicious to establish a linear correlation between hematological and histological parameters as demonstrated by Nigro in their study. They propose the use of the fractal dimension as a new estimator of nephron integrity. Indeed, it would have been wise toboth the fractal dimension of tubules and the density of tubules have significant positive correlation with the eGFR and inverse correlation with the level of uric acid and urea. They observed that tubular density predicted for the levels of uric acid in different pathological conditions. This result is in agreement with previous observation that the strongest correlate of renal function is the relative interstitial volume [10]. In addition, dialysis with high permeability membranes and plasma exchanges are not routinely performed in our centers. Some studies evoke their interest in the management of these kidney attacks, although their effectiveness remains controversial [11]. Note that our results remain similar to those of authors in developing countries where MP and M-Dex are still used in more than 50% of cases [12-14].
The statistical analysis shows a statistically significant correlation between the occurrence of a death and the presence of anemic syndrome (p=0.019) and hyperbeta2- microglobulinemia (p=0.003). These factors are described in the literature in addition to advanced age, general impairment, bone lytic lesions, hypercalcemia and thrombocytopenia [6,15,16]. In the literature, predictive factors for renal impairment were age, gender, arterial hypertension, diabetes, NSAIDs, exposure to toxic products, and herbal intake. We also found a significant association between hyperprotidemia (p=0.028) and renal impairment. This reinforces the assertions of Bridoux and Kumar's team [17,18]. In multivariate analysis, male gender is significantly correlated with severe impairment of renal function (p=0.008). In terms of prognosis, recovery of renal function was negatively correlated with hyperprotidemia (P=0.001) and proteinuria (p=0.0039). These results corroborate the data from the literature [17-19]. The association with a urinary tract infection was a better prognosis (p=0.010). Patients treated with Velcade and those whose medications were adapted for renal function had better recovery of renal function (P=0.008). The 1- year overall survival rate was 17.4%, which is lower than the data from the Asian and European literature [20-22]. This low rate could be explained by the fact that half of our patients were lost to follow-up. Knudsen reports, however, that 12-month survival is more dependent on the reversibility of renal function than on the efficacy of chemotherapy [23]. Thus, recovery of renal function would improve long-term survival. This conclusion could perfectly explain our results.
Conclusion
Prognosis of renal impairment in multiple myeloma in Senegal remains poor because of the delay in management between the diagnosis of myeloma and the actual start of treatment. Predictors of kidney disease are dominated by age, gender, high blood pressure, diabetes, NSAIDs, exposure to toxic products, and herbal intake; the prognostic factors are the same reported in the current literature. In our work, renal impairment is related to the male genus, proteinuria and hyperprotidemia.
Accessibility to the latest generation of chemotherapies and care in general remains the major challenge to improve this situation. As noted in our study, recovery of renal function is positively correlated with Velcade treatment and dosage adjustment of drugs. The same is true for overall survival at 1 year, which is improved by the reversibility of renal function.
References
- Chng WJ, Dispenzieri A, Chim CS, Fonseca R, Goldschmidt H, et al. (2014) IMWG consensus on risk stratification in multiple myeloma. Leukemia 28: 269-277.
- Gorsane I, Barbouch S, Mayara M, Abdelghani KB, Goucha R, et al. (2016) Renal impairment in multiple myeloma: A single center experience. Saudi J Kidney Dis Transplant Off Publ Saudi Cent Organ Transplant Saudi Arab 27: 480-485.
- Blade J, Fernandez-Llama P, Bosch F, Montoliu J, Lens XM, et al. (1998) Renal failure in multiple myeloma: Presenting features and predictors of outcome in 94 patients from a single institution. Arch Intern Med 28158: 1889-1893.
- Ecotiere L, Thierry A, Debiais-Delpech C, Chevret S, Javaugue V, et al. (2016) Prognostic value of kidney biopsy in myeloma cast nephropathy: A retrospective study of 70 patients. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc 31: 64-72.
- Kleber M, Ihorst G, Udi J, Koch B, Wasch R, et al. (2012) Prognostic risk factor evaluation in patients with relapsed or refractory multiple myeloma receiving lenalidomide treatment: Analysis of renal function by eGFR and of additional comorbidities by comorbidity appraisal. Clin Lymphoma Myeloma Leuk 12: 38-48.
- Haynes RJ, Read S, Collins GP, Darby SC, Winearls CG (2010) Presentation and survival of patients with severe acute kidney injury and multiple myeloma: A 20-year experience from a single centre. Nephrol Dial Transplant Off Publ Eur Dial Transpl Assoc - Eur Ren Assoc 25: 419-426.
- Viggiano (2018) Urate-Lowering agents in asymptomatic hyperuricemia: Role of urine sediment analysis and musculoskeletal ultrasound Kidney Blood Press Res 43: 606-615.
- Nigro M, Sanctis C, Formisano P, Stanzione R, Forte M, et al. (2018) Cellular and subcellular localization of uncoupling protein 2 in the human kidney. J Molecular Histology 49: 437-445.
- Durie BG, Stock-Novack D, Salmon SE, Finley P, Beckord J, et al. (1990) Prognostic value of pretreatment serum beta 2 microglobulin in myeloma: a Southwest Oncology Group Study. Blood 75: 823-830.
- Nigro (2018) A cross-sectional study on the relationship between hematological data and quantitative morphological indices from kidney biopsies in different glomerular diseases. BMC Nephrology 19: 62
- Hutchison C, Bridoux F, Fermand JP (2011) Renal improvement in myeloma with plasma exchange. N Engl J Med 365: 1060-1062.
- Ben Abdeladhim A, Aissaoui B, Ben Othman T, Gharbi A, Bouguerra A, et al. (1989) Multiple myeloma. General etiologic data (68 cases). Blood and/or urine protein anomalies (67 cases). Tunis Med. 67: 607-612.
- El Husseiny NM, Kasem N, El Azeeim HA, Mattar MW (2014) Multiple myeloma: A descriptive study of 217 Egyptian patients. Ann Hematol 93: 141-145.
- Fall S, Dieng F, Diouf C, Djiba B, Ndao AC, et al. (2017) Diagnostic and evolutionary profile of multiple myeloma in Senegal: Monocentric study conducted from 2005 to 2016. Pan Afr Med J 27: 262.
- Haynes R, Leung N, Kyle R, Winearls CG (2012) Myeloma kidney: Improving clinical outcomes Adv Chronic Kidney Dis 19: 342-351.
- Chombart B, Lemoussu LG, Eschard JP, Ackah-Miezan S, Novella JL, et al. (2005) Factors useful for predicting survival of myeloma patients in everyday practice. A 10-year study of 148 patients older than 55 years. J Bone Spine Rev Rhum 72: 544-549.
- Kumar SK, Lee JH, Lahuerta JJ, Morgan G, Richardson PG, (2012) et al. Risk of progression and survival in multiple myeloma relapsing after therapy with IMiDs and bortezomib: A multicenter international myeloma working group study. Leukemia 26: 149-157.
- Bridoux F, Delbes S, Sirac C, Pourreau F, Puyade M, et al. (2012) Renal disorders associated with monoclonal gammopathies: Diagnostic and therapeutic progress. Presse Medicale Paris Fr 41: 276-289.
- Kumar S, Paiva B, Anderson KC, Durie B, Landgren O, et al. (2016) International myeloma working group consensus criteria for response and minimal residual disease assessment in multiple myeloma. Lancet Oncol 17: e328-e346.
- Kim K, Lee JH, Kim JS, Min CK, Yoon SS, et al. (2014) Clinical profiles of multiple myeloma in Asia-An Asian Myeloma Network study. Am J Hematol 89: 751-756.
- Takahashi N (2015) Multiple myeloma and renal impairment. Nihon Rinsho Jpn J Clin Med 73: 38-41.
- Heher EC, Rennke HG, Laubach JP, Richardson PG (2013) Kidney disease and multiple myeloma. Clin J Am Soc Nephrol CJASN 8: 2007-2017.
- Knudsen LM, Hjorth M, Hippe E (2000) Renal failure in multiple myeloma: Reversibility and impact on the prognosis. Nordic myeloma study group. Eur J Haematol 65: 175-181.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences