Multidisciplinary Approach to Correct Alveolar Bone Loss and Vertical Maxillary Deficiency to Restore Dento-Maxillofacial Aesthetics and Functional Ability
Piyush Sharma1, Linjing Shu2, Wang Tao1*, Rami Dawazeh3 and Ankit Sharma4
1Department of Oral Surgery, Affiliated Hospital of Stomatology, Chongqing Medical University, Chongqing, P.R. China
2Department of Oral Implantology, Affiliated Hospital of Stomatology, Chongqing Medical University, Chongqing, P.R. China
3Department of Neurosurgery, First Affiliated Hospital of Chongqing Medical University, Chongqing, P.R. China
4Department of Oral Surgery, Affiliated Hospital of Stomatology, Peking Medical University, Beijing, P.R. China
- *Corresponding Author:
- Wang Tao
Head Department of Oral Surgery, Affiliated Hospital of Stomatology
Chongqing Medical University, Chongqing, P.R. China
E-mail: taosan@126.com
Received date: April 19, 2016; Accepted date: May 25, 2016; Published date: May 29, 2016
Citation: Sharma P, Shu L, Tao W, Dawazeh R, Sharma A (2018) Multidisciplinary Approach to Correct Alveolar Bone Loss and Vertical Maxillary Deficiency to Restore Dento-Maxillofacial Aesthetics and Functional Ability. Int J Case Rep 2:5
Copyright: © 2018 Sharma P, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Several techniques have been reported to increase the amount of bone for maintain the architecture of the residual jaw bone crest, which decides the ideal placement of dental implants. Disagreement is still present among clinicians about ideal treatment as direct comparison among procedures is virtually impossible. The use of autogenous bone grafts for ridge augmentation is, on the other hand, recommended by most authors, due to the intrinsic properties of the bone. This case report is to restore the function and aesthetics of a patient with iatrogenic loss of maxillary anterior tooth with severe bone loss and a vertical maxillary deficiency with a contemporary multidisciplinary approach using Le fort I osteotomy, inlay and onlay bone graft, palate pedicle flap and eventual implant placement.
Keywords
Alveolar bone loss; Vertical maxillary deficiency; Orthognathic surgery
Introduction
Various techniques have been reported to increase the amount of bone for maintain the architecture of the residual jaw bone crest, which decides the ideal placement of dental implants. Disagreement is still present among clinicians about ideal treatment as direct comparison among procedures is virtually impossible [1-3]. The use of autogenous bone grafts for ridge augmentation is, on the other hand, recommended by most authors, due to the intrinsic properties of the bone [4].
Nowadays, precise technique in orthognathic surgery is more and more important with the development of digital technology, 3D printing techniques, navigation technology and special surgical instruments for orthognathic surgery [5-8]. The reliability and precision of computer-assisted orthognathic surgery have been widely reported so a comprehensive preoperative analysis and surgical plan assisted with 3D sterolithographic model and guided implant placement has made it more precise to analyze the outcome of surgery and desired results.
In this case report is to restore the function and aesthetics of a patient with iatrogenic loss of maxillary anterior tooth with severe bone loss and a vertical maxillary deficiency with a contemporary multidisciplinary approach using Le fort I osteotomy, in lay and on lay bone graft, palate pedicle flap and eventual implant placement.
Case Report
A 19-year old female patient approached the department of oral and maxillofacial surgery with the chief complaint of loss of maxillary anterior teeth after an orthodontic mal treatment in another hospital; her chief complaint was to restore the aesthetics and her missing teeth replacement.
The intra oral examination revealed loss of maxillary anterior along with malocclusion. After radiographic evaluation we found there was severe horizontal and vertical loss of alveolar bone in the maxillary anterior region limiting the implant placement, and after Delaire architectural cephalometric analysis we found vertical maxillary deficit with a concave facial profile and a steep curve of spee, a comprehensive surgical plan was made which included Le fort I osteotomy and variety of bone grafts to achieve the desired aesthetics and sufficient bone and soft tissue for implant placement.
There was no previous history of any systemic pathology, past medical and familial history were non-contributory.
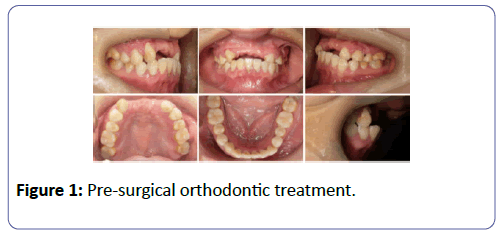
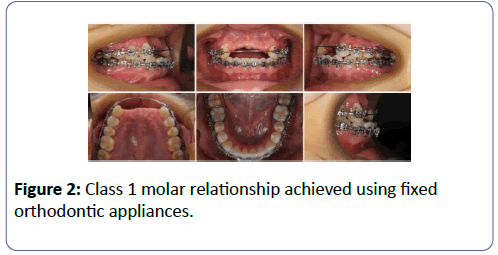
Pre-surgical orthodontic treatment was started in June 2011 by giving the patient a removable partial denture for bilaterally missing central and lateral incisors and fixed orthodontic appliances to achieve class 1 molar relationship and by august 2012 we were able to achieve it (Figures 1 and 2).
Orthognathic surgery
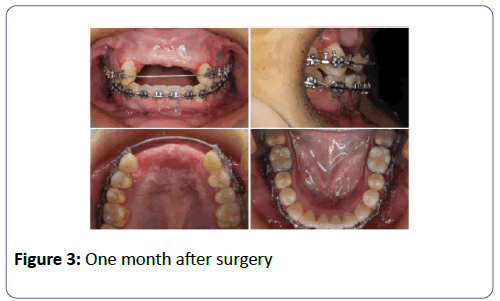
Before proceeding to the surgical incision for Le fort I osteotomy a solution of local anesthetic with epinephrine (2% lidocaine with 1:100000 epinephrine) is infiltrated into the buccal mucosa along the entire surface of the, maxilla was repositioned forward and downward based on the 3 d paint analysis. The obtained mandibular rami interposition bone graft are also secured to the atrophic maxilla using 1.8 mm titanium screws bilaterally (Figure 3).
The maxillary midline was checked in relation to the external reference, for stability, 2-mm L-shaped plates, placed on each of the maxillary buttresses, and closed with an absorbable suture. This is done with a 3.0 or 4.0 Vicryl suture in a horizontal mattress-type fashion to ensure a watertight closure.
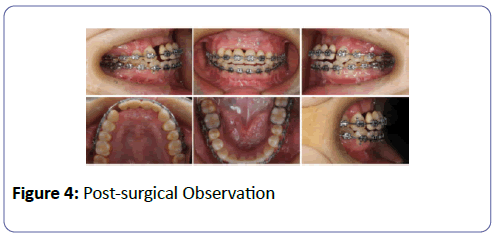
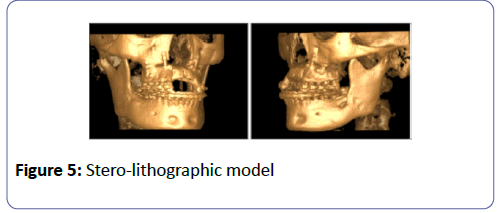
After 6 months we checked the post-surgical results on analysis we observed the amount of bone regenerated was not enough to obtain implant support esthetic outcome, but we were able to achieve better facial profile and aesthetics (Figures 4 and 5).
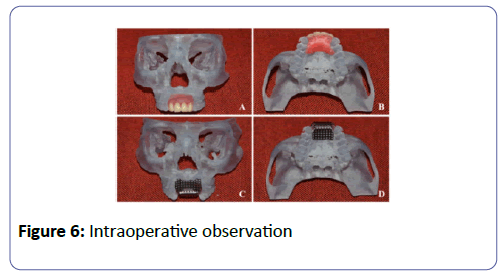
We planned bone grafting a 3 d stero-lithographic model using calvarium chips, iliac marrow and bios auto graft secured by titanium mesh, the stereo-lithographic model was available, the mesh was shaped and adjusted on the resin model before surgery. The incisions were extended pericoronally and horizontally to raise the flap, over the mesh 0.2-mm-thick mesh systems were used,Micro Dynamic Mesh (Howmedica Lei-binger GmbH & Co., KG, Freiburg, Germany) and Modus 1,5 Mesh (Institut Straumann AG, Waldenburg, Switzerland).The mesh was customized and modified to the resemble the individual anatomy and maintain and secure the foundation of the graft (Figure 6).
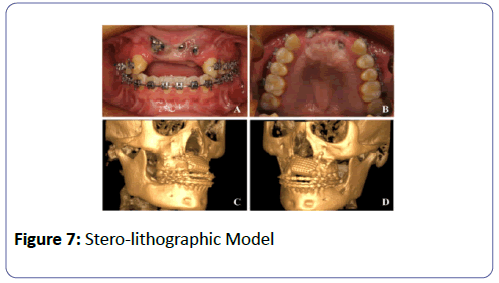
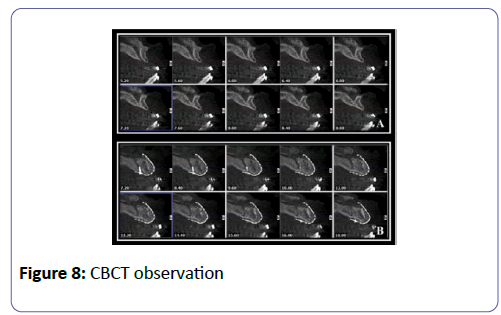
After 4 months a CBCT was performed which revealed enough vertical and horizontal bone and the density of bone was good to plan placement of implants using the normal surgical guide (Figures 7 and 8).
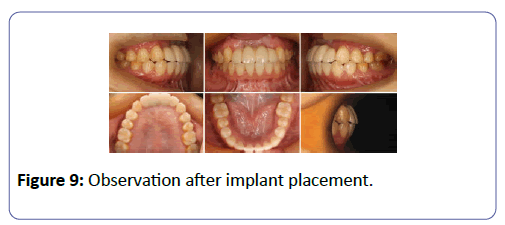
After 4 months, a second surgery was performed at the recipient site. After the removal of titanium screws and mesh, a full thickness of palatal mucosa tissue in the middle of palate was incision and transplanted to reconstruct the front alveolar gum and the depth of the vestibule was reduced 2 Thommen ELEMENT RF 4.0 × 11 implants were placed, in a non-submerged fashion, a connective tissue graft was transferred from the palate and it was sutured onto the area to obtain thicker marginal tissues around the implants (Figure 9).
Discussion
Bone grafting concurrently with Le Fort I osteotomy inlay grafting to increase facial vertical dimension and immediately improved profile, Delaire architectural analysis and CBCT can be an available tool for measurement of both skeletal and softtissue changes enabling 3D assessment of morphologic changes, repositioning of the maxilla to compensate for maxillary deficiency could be achieved by placing inlay grafts obtained from mandibular chin region. Autogenous bone from chin was reported to present minimal discomfort for the patients [9-11]. In our experience, however, the morbidity of chin bone harvesting was in accordance [12,13].
The results of this clinical investigation suggest that vertical ridge augmentation with Ti-mesh and mixture of autogenous bone, iliac marrow and bios auto graft is predictable and high quality does not go through major resorption; In spite of a small band of fibrous tissue formed, even if mesh exposure occurs. Implants can be inserted 4 to 6 months following surgical placement of the autograft.
This study favors the use of a delayed approach when using autogenous bone grafts and titanium implants for reconstruction of the severely atrophied maxilla. The possible clinical advantages of this technique include:
• The applicability to severe vertical deficit associated with large reduction in width;
• The reduction of total time for the rehabilitation;
• The lack of major complications if soft-tissue dehiscence and mesh exposures do occur and
• The decrease of risk of injuries to neurovascular bundle or sinus and/or fractures.
The excellent biocompatibility of titanium and the easy handling of the titanium micro-mesh systems allowed reconstruction of large bony defects. The ridge was augmented to receive the implants needed in the desired position and angulation with no major complication. The most likely hypothesis that can explain the apparent benefits of the mesh lies in its probable protective effect during the healing time following bone grafting, as already found with non-resorbable membranes [14,15].
Tedious planning of implant placement not only facilitates minimal invasive treatment and reduced chair time but also enables the clinician to bring surgery and restoration to a desired level. Contemporary 3D imaging technologies provide clinician with an accurate overview of the availability of bone for the procedures like distraction and implant placement, together with the consideration of critical anatomical structures. More years of observation are, however, necessary to verify if osseo-integration in this type of augmented bone can equally be maintained over a long period of time [16,17].
References
- Oh YW, Han KT, Ahn ST (1990) The complication of mandibular angle reduction. J Korean Soc Plast Reconstr Surg 17: 645-652.
- Hwang K, Han JY, Kil MS, Lee SI (2002) Treatment of condyle fracture caused by mandibular angle osteotomy. J Cranio Fac Surg 13: 709-712.
- Kane AA, Lo LJ, Chen YR, Hsu KH, Noordhoff MS (2000) The course of the inferior alveolar nerve in the normal human mandibular ramus and in patients presenting for cosmetic reduction of the mandibular angles. Plast Reconstr Surg 106: 1162-1174.
- Antoun H, Sitbon JM, Martinez, H, Missika P (2001) A prospective randomized study comparing two technique of bone augmentation: onlay graft alone or associated with a membrane. Clin Oral Implants Res 12: 632-639.
- Hernandez-Alfaro F, Guijarro-Martinez R (2013) New protocol for three-dimensional surgical planning and CAD/CAM splint generation in orthognathic surgery: an in vitro and in vivo study. J Oral Maxillo Fac Surg 42: 1547-1556.
- Hsu SS, Gateno J, Bell RB (2013) Accuracy of a computer-aided surgical simulation protocol for orthognathic surgery: a prospective multicenter study. J Oral Maxillo Fac Surg 71: 128-142.
- Plooij JM, Maal TJ, Haers P, Borstlap WA, Kuijpers-Jagtman AM, et al. (2011) Digital three-dimensional image fusion processes for planning and evaluating orthodontics and orthognathic surgery: a systematic review. J Oral Maxillo Fac Surg 40: 341-352.
- Lee TS (2015) Standardization of surgical techniques used in facial bone contouring. J Plast Reconstr Aesthet Surg 68: 1694-1700.
- Jodia K, Sadhwani BS, Parmar BS, Anchlia S, Sadhwani SB (2014) Sinus elevation with an alloplastic material and simultaneous implant placement: a 1-stage procedure in severely atrophic maxillae. J Maxillofac Oral Surg 13: 271-280.
- Kher U, Mazor Z, Stanitsas P, Kotsakis GA (2014) Implants placed simultaneously with lateral window sinus augmentation using a putty alloplastic bone substitute for increased primary implant stability: a retrospective study. Implant Dent 23: 496-501.
- Ozan O, Seker E, Kurtulmus-Yilmaz S, Ersoy AE (2012) Clinical application of stereolithographic surgical guide with a handpiece guidance apparatus: a case report. J Oral Implantol 38: 603-609.
- Sarment DP, Sukovic P, Clinthorne N (2003) Accuracy of implant placement with a stereo-lithographic surgical guide. Int J Oral Maxillofac Implants 18: 571-577.
- Pikos MA (1996) Facilitating implant placement with chin grafts as donor sites for maxillary bone augmentation-Part II. Dent Implantol update 7: 1-4.
- Bahat O, Fontanesi RV (2001) Complications of Grafting in the Atrophic Edentulous or Partially Edentulous Jaw. Int J Perio Rest Dent 21: 487-495.
- Weber HP, Fiorellini JP, Jeffcoat MC (1997) Clinical trials on placemen To implantsin existing bone. Annals of Periodontology 2: 315-328.
- Williamson RA (1996) Rehabilitation of the resorbed maxilla and mandible using autogenous bone grafts and osseo integrated implants. Int J Oral Maxillofac Implants 11: 476-488.
- Zeiter DJ, Ries WL, Sanders JJ (2000)The use of a bone block graft from the chin for alveolar ridge augmentation. Int J Periodontics Restor Dentistry 20: 619-627.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences