Magnetic Resonance Imaging-guided Focused Ultrasound Unilateral Pallidotomy for Parkinson's Disease: A Case Report
Hisashi Ito1*, Takaomi Taira2, Shigeru Fukutake1, Kazuaki Yamamoto3, Yasuhisa Baba4, Toshio Yamaguchi5 and Tetsumasa Kamei1
1Department of Neurology, Shonan Fujisawa Tokushukai Hospital, Fujisawa, Japan
2Department of Neurosurgery, Tokyo Women’s Medical University, Tokyo, Japan
3Department of Neurosurgery, Shonan Kamakura General Hospital, Kamakura, Japan
4Department of Neurology, University Hospital Mizonokuchi, Teikyo University School of Medicine, Kawasaki, Japan
5Research Institute of Diagnostic Imaging, Shin-Yurigaoka General Hospital, Kawasaki, Japan
- *Corresponding Author:
- Hisashi Ito
Department of Neurology, Shonan Fujisawa Tokushukai Hospital, 251-0041, Fujisawa, Japan
Tel: +81-466-35-1177
E-mail: hisashi.ito@tokushukai.jp
Received date: February 21, 2018; Accepted date: March 14, 2018; Published date: March 19, 2018
Citation: Ito H, Taira T, Fukutake S, Yamamoto K, Baba Y, et al. (2018) Magnetic Resonance Imaging-guided Focused Ultrasound Unilateral Pallidotomy for Parkinson’s Disease: A Case Report. Int J Case Rep 2:3.
Copyright: © 2018 Ito H, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Unilateral pallidotomy has been accepted as an effective therapeutic option for Parkinson’s disease (PD). We herein report a PD patient with wearing-off and dyskinesia who underwent left globus pallidus internus (GPi) pallidotomy using magnetic resonance imaging-guided focused ultrasound (MRgFUS). Her skull density ratio (SDR) was too low to perform MRgFUS procedure; however, it improved with bisphosphonate. Right-sided wrist rigidity, finger movement, and resting tremor improved immediately following the ultrasound energy delivery. Wearing-off improved and dyskinesia abolished after the procedure. No severe adverse events were observed. MRgFUS is a minimally invasive treatment; however, further investigations concerning not only technical problems such as SDR but also long-term efficacy and safety of this new treatment for PD patients should be necessary.
Keywords
Parkinson’s disease; Magnetic resonance imaging-guided focused ultrasound; Pallidotomy
Introduction
The first procedure of human stereotactic neurosurgery is a pallidotomy for a patient with Huntington’s disease. It was soon adopted for Parkinson’s disease (PD) because of its efficacy on most parkinsonian symptoms including levodopa-induced dyskinesias [1]. The posterior and ventral part of the globus pallidus internus (GPi) was confirmed to play an important role and posteroventral pallidotomy had been endorsed as an evidence-based surgical procedure for PD [2,3]. Magnetic resonance imaging (MRI)-guided focused ultrasound (MRgFUS) is a new technology that enables minimum intracranial focal ablation and applied several neurological and psychological disorders [4]. MRgFUS thalamotomy for essential tremor was approved by FDA. However, MRgFUS pallidotomy has not yet been approved for PD and we could find only one case report about unilateral GPi pallidotomy using MRgFUS for PD patient [5]. Herein, we report a 78-year-old Japanese PD patient who underwent left GPi pallidotomy using MRgFUS.
Case Report
A right-handed 78-year-old woman developed resting tremor in right leg at 63 years of age. She was diagnosed with PD and started medication including levodopa, however, she developed disabling wearing-off at 69 years of age and levodopa-induced dyskinesia at 73 years of age. As of February 2017, she was prescribed 450 mg of levodopa/carbidopa, 300 mg of entacapone, 10 mg of selegiline, 0.75 mg of pramipexoleextended release, and 40 mg of istradefylline. Therefore, the levodopa equivalent dose (LED) was 773.5 mg [6]. Off-periods in 7 days prior to the pallidotomy were 3.5 ± 1.6 h on diary. Movement Disorder Society-Sponsored Revision of the Unified Parkinson's Disease Rating Scale (MDS-UPDRS) score was 10 for part I, 14 for part II, 19 (on medication) and 33 (off medication) for part III, and 8 for part IV. Unified Dyskinesia Rating Scale (UdysRS) score was 28. She was not demented and Mini-Mental State Examination was 26/30. Brain MRI showed no abnormal findings. We offered radiological or neurosurgical treatments including deep brain stimulation (DBS), however, she refused them because of the invasiveness.
We scheduled MRgFUS unilateral pallidotomy, which has been approved by the Review Board of Tokushukai Medical Alliance for advanced PD patients suffering from medication-resistant motor-fluctuation and who have refused other procedures involving DBS. The patient provided her written informed consent in accordance with the Declaration of Helsinki before treatment commenced. The skull density ratio, which reflects the amount of ultrasound energy that can penetrate the skull effectively [7], was 0.26 in February 2017 (exclusion criteria: ≤ 0.30). As she was associated with osteoporosis, we administered 35 mg of alendronate per week to elevate SDR to 0.36 after 6 months.
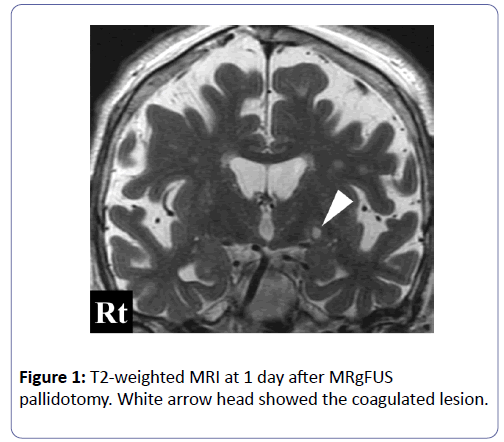
In August 2017, we performed MRgFUS unilateral GPi pallidotomy. MRgFUS ultrasonic bursts (sonications) were performed using a 1.5-Tesla MRI (Signa HDx, GE Healthcare, Milwaukee, USA) and a focused ultrasound system (Exablate 4000®, InSightec, Tirat Carmel, Israel). The day before pallidotomy, we performed T2-weighted MRI to plan the procedure. Based on the patient’s preference, we selected the left GPi as the target. We chose the target for GPi at a point 3 mm anterior to the midpoint between anterior and posterior commissure, 20 mm lateral from the midline, and 1.5 mm below. We stopped her medications for 24 h before MRgFUS to facilitate assessment during the procedure. On the day of the procedure, the patient was placed in a stereotactic head flame which was coupled to 1,024 elements, phased-array ultrasound transducer. After stereotactic targeting using MRI, we gradually increased the total energy of the sonications by either increasing the intensity or extending the sonication duration with marking left optic nerve to monitor its temperature. We finished the sonications when an adequate improvement in right-sided wrist rigidity, finger movement, and resting tremor following 12 sonications with an average maximum sonication time of 24.0 ± 11.6 s (range 10-42 s). The mean energy reached 20229.1 ± 13391.5 J (range 1206-35740 J) with a mean maximum temperature of 46.3 ± 4.0°C (range 39-51°C). We made two lesions in left postventral GPi. T2-weighted MR image following the procedure showed the increased intensity lesion in left GPi and the maximum ablated tissue volume was approximately 71.8 mm3 (Figure 1). Left temporal pain occurred during the sonication, however, we did not observe visual field deficit. Mild swelling of left eyelid occurred after the procedure, which improved within 3 days.
After the procedure, dyskinesia abolished and wearing-off improved. The reduction of UPDRS part I and part II scores were limited, however, UPDRS part III scores reduced over 24 weeks after the procedure (94.7% on medication and 63.6% off medication after 24 weeks, respectively), which enabled us to reduce the parkinsonian medications. UPDRS part IV score reduced after the procedure also. Furthermore, UdysRS score reduced to 0 according to the reduction of the medications (Table 1).
| Baseline | After 4 weeks | After 8 weeks | After 12 weeks | After 24 weeks | |
|---|---|---|---|---|---|
| MDS-UPDRS | |||||
| Part I | 10 | 7 | 10 | 13 | 10 |
| Part II | 14 | 10 | 12 | 12 | 13 |
| Part III (on medication) | 19 | 3 | 1 | 1 | 1 |
| Part III (off medication) | 33 | 12 | 11 | 10 | 12 |
| Part IV | 8 | 8 | 7 | 6 | 3 |
| UdysRS | 28 | 0 | 0 | 0 | 0 |
| LED (mg) | 773.5 | 332.5 | 449 | 449 | 499 |
Table 1: UPDRS scores, UdysRS score, and LED; UPDRS: Unified Parkinson’s Disease Rating Scale; UdysRS: Unified dyskinesia Rating Scale; LED: Levodopa Equivalent Dose.
Discussion
The therapeutic use of focused ultrasound was pioneered by Fry brothers in the 1950s [8]. To date, MRgFUS has been applied for several neurological and psychological disorders such as essential tremor [9], PD [5,10-12], obsessive-compulsive disorder [13], and neuropathic pain [14]. Regarding PD, target lesions are GPi [5], pallidothalamic tract [10], ventral intermediate nucleus (Vim) [11,12], ventro oralis posterior nucleus [12]. Na and colleagues reported the first MRgFUS GPi pallidotomy for PD patient with levodopa-induced dyskinesias, which is the only previous report of GPi pallidotomy using MRgFUS for PD. The patient achieved a 50.0% (on medication) and 61.0% (off medication) reduction in UPDRS part III score without changes in LED at 1 week [5]. We observed better improvements of motor functions despite the reduction of LED, which might have led to the disappearance of dyskinesia.
MRgFUS are characterized by minimum invasiveness, no exposure to radiation, and an immediate therapeutic effect (Table 2) [15]. However, poor permeability and high ultrasound absorption by the skull are a technological barrier. Skull volume and SDR exhibited relationships with the maximum temperature in target lesion. The former was negatively correlated with maximal temperature in the target lesion, whereas the latter showed a positive correlation [7]. We have to exclude MRgFUS candidates occasionally because of low SDR value. As GPi locates more laterally than Vim, reflection of ultrasounds in GPi pallidotomy is higher than that in Vim thalamotomy, which lead to a difficulty to achieve enough elevation of target lesion temperature. Thus, high SDR value is necessary especially in GPi pallidotomy. Because of the comorbid osteoporosis, we could administer bisphosphonate. Alendronate, a second generation bisphosphonate, had been reported to increase the degree and uniformity of bone matrix mineralization and decrease the porosity in cortical bone [16]. Alendronate could be one of the therapeutic options for MRgFUS candidates with low SDR value.
| RF-thermo- coagulation | γ-knife | DBS | MRgFUS | |
|---|---|---|---|---|
| Hair Shaving | Partial | None | Partial | Complete |
| Incision/Burr hole | Must | None | Must | None |
| Radiation | Low (X-ray, CT) | High | Low (X-ray, CT) | Low (screening CT) |
| General Anesthesia | No | No | Yes* | No |
| Therapeutic Duration | 1 h | 1 h | 2~4 h | 3~4 h** |
| Efficacy Onset | Immediate | Delayed upto 1 year | Adjustable | Immediate |
| Bilateral Procedure | Impossible | Impossible | Possible | Unknown |
| Post-treatment MRI | Possible | Possible | Limited*** | Possible |
| Hemorrhagic Complications | Possible | Almost None | Possible | Almost None |
| Infection | Possible | None | Possible | None |
| Long-term data | Yes | Yes | Yes | Unknown |
Table 2: The features of the standard radiological and neurosurgical treatments in functional neurosurgery and MRgFUS [15]; * - for implantation of pulse generator; ** - time spent in MRI room; ***- as a courtesy of InSightec.
MRgFUS GPi pallidotomy might become a viable therapeutic option for PD patients with medication refractory motor fluctuation who do not select standard neuromodulation therapies including DBS. However, not only technical problems but also long-term efficacy and safety of this new treatment for PD patients remain to be elucidated. Further investigations should be necessary.
Conclusion
We report the first experience of unilateral GPi pallidotomy using MRgFUS for PD patient from Japan.
References
- Cif L, Hariz M (2017) Seventy years of pallidotomy for movement disorders. Mov Disord 32: 972-982.
- Goetz CG, Poewe W, Rascol O, Sampaio C (2005) Evidence-based medical review update: pharmacological and surgical treatments of Parkinson’s disease: 2001 to 2004. Mov Disord 20: 523-539.
- Fox SH, Katzenschlager R, Lim SY, Ravina B, Seppi K, et al. (2011) The Movement Disorder Society Evidence-Based Medicine Review Update: Treatments for the motor symptoms of Parkinson’s disease. Mov Disord 26: S2-S41.
- Weintraub D, Elias WJ (2017) The emerging role of transcranial magnetic resonance imaging–guided focused ultrasound in functional neurosurgery. Mov Disord 32: 20-27.
- Na YC, Chang WS, Jung HH, Kweon EJ, Chang JW (2015) Unilateral magnetic resonance-guided focused ultrasound pallidotomy for Parkinson disease. Neurology 85: 549-551.
- Tomlinson CL, Stowe R, Patel S, Rick C, Gray R, et al. (2010) Systematic review of levodopa dose equivalency reporting in Parkinson’s disease. Mov Disord 25: 2649-2653.
- Chang WS, Jung HH, Zadicario E, Rachmilevitch I, Tlusty T, et al. (2016) Factors associated with successful magnetic resonance-guided focused ultrasound treatment: efficiency of acoustic energy delivery through the skull. J Neurosurg 124: 411-416.
- Fry WJ, Mosberg WH, Barnard JW, Fry FJ (1954) Production of focal destructive lesions in the central nervous system with ultrasound. J Neurosurg 11: 471-478.
- Elias WJ, Lipsman N, Ondo WG, Ghanouni P, Kim YG, et al. (2016) A randomized trial of focused ultrasound thalamotomy for essential tremor. N Engl J Med 375: 730-739.
- Magara A, Bühler R, Moser D, Kowalski M, Pourtehrani P, et al. (2014) First experience with MR-guided focused ultrasound in the treatment of Parkinson's disease. J Ther Ultrasound 2: 11.
- Zaaroor M, Sinai A, Goldsher D, Eran A, Nassar M, et al. (2017) Magnetic resonance–guided focused ultrasound thalamotomy for tremor: a report of 30 Parkinson’s disease and essential tremor cases. J Neurosurg 24: 1-9.
- Ito H, Fukutake S, Yamamoto K, Yamaguchi T, Taira T, et al. (2017) Magnetic resonance imaging-guided focused ultrasound thalamotomy for Parkinson’s disease: a case report. Intern Med 9586-17.
- Jung HH, Chang WS, Rachmilevitch I, Tlusty T, Zadicario E, et al. (2015) Different magnetic resonance imaging patterns after transcranial magnetic resonance–guided focused ultrasound of the ventral intermediate nucleus of the thalamus and anterior limb of the internal capsule in patients with essential tremor or obsessive-compulsive disorder. J Neurosurg 122: 162-168.
- Jeanmonod D, Werner B, Morel A, Michels L, Zadicario E, et al. (2012) Transcranial magnetic resonance imaging–guided focused ultrasound: noninvasive central lateral thalamotomy for chronic neuropathic pain. Neurosurg Focus 32: E1. 
- Rohani M, Fasano A (2017) Focused ultrasound for essential tremor: review of the evidence and discussion of current hurdles. Tremor and other hyperkinetic movements. Tremor Other Hyperkinet Mov (NY) 7: 462.
- Roschger P, Rinnerthaler S, Yates J, Rodan GA, Fratzl P, et al. (2001) Alendronate increases degree and uniformity of mineralization in cancellous bone and decreases the porosity in cortical bone of osteoporotic women. Bone 29: 185-191.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences