Investigating the Use of Education on Diet and Medical Comorbidities to Reduce Cataract Surgery Screening Failure in a Rural Community in Imo State, Nigeria
Aaron Anderson1, Christina Friedl1, Adaure Nwaba2, Victoria P Rajamanickam3, Kelechi Mezu-Nnabue4, Emmanuel Esenwah5, Ikoro C Nwakaego5, Chandra Suresh6 and Olachi Mezu-Ndubuisi1
1Department of Pediatrics, University of Wisconsin, Madison, United States
2Johns Hopkins University, Baltimore
3Department of Statistics, University of Wisconsin, Madison, United States
4Mezu International Foundation, Pikesville
5Department of Optometry, Federal University of Technology, Owerri, Nigeria
6Department of Ophthalmology and Visual Sciences, University of Wisconsin, Madison, United States
- *Corresponding Author:
- Olachi J Mezu-Ndubuisi
Assistant Professor
Department of Pediatrics
University of Wisconsin Madison, United States
Tel: 6082653397
Email: olachimezu@pediatrics.wisc.edu
Received Date: December 14, 2018; Accepted Date: January 15, 2019; Published Date: January 21, 2019
Citation: Anderson A, Friedl C, Nwaba A, Rajamanickam VP, Mezu-Nnabue K, et al. (2018) Investigating the Use of Education on Diet and Medical Comorbidities to Reduce Cataract Surgery Screening Failure in a Rural Community in Imo State, Nigeria. J Eye Vis .2:1
Abstract
Introduction
Cataracts are one of the leading causes of preventable blindness worldwide. A community health assessment in rural south-East Nigeria showed that lack of finances and poor knowledge were contributory factors to early cataracts. Free cataract surgeries were scheduled, but only 10 out of 100 patients qualified due to untreated medical comorbidities like hypertension, diabetes, glaucoma and anemia. This study aims to investigate the feasibility of using an electronic (E)-based educational program to educate patients on managing medical comorbidities in order to reduce the cataract surgery screening failure rate in the community.
Methods
Using a questionnaire format, a cross-sectional study was administered to 40 males and 43 females aged 45-85 years with a diagnosis of mature cataracts. Questions focused on socioeconomic status, quality of life, diet diversity and E-learning readiness.
Findings
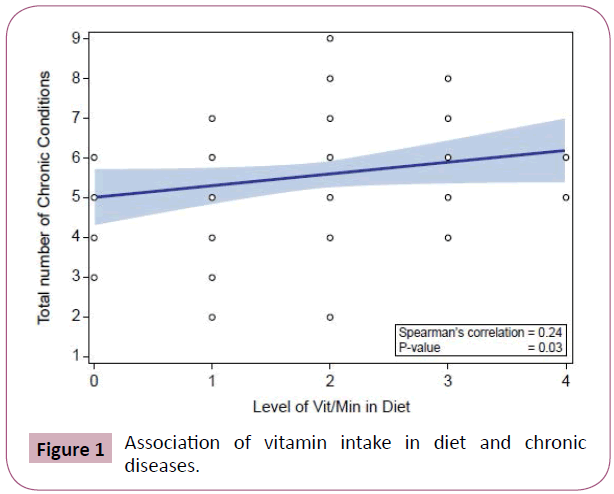
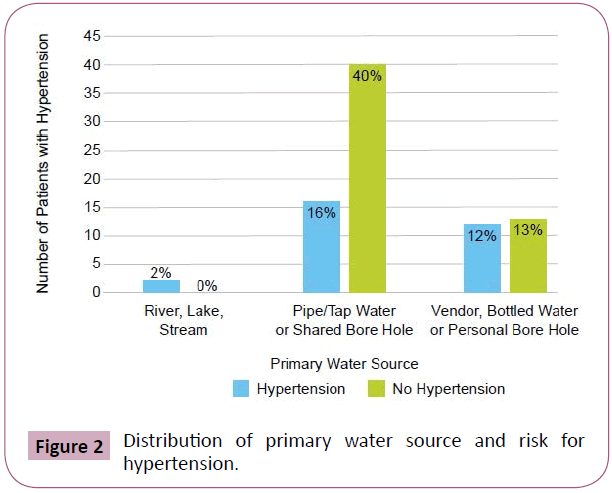
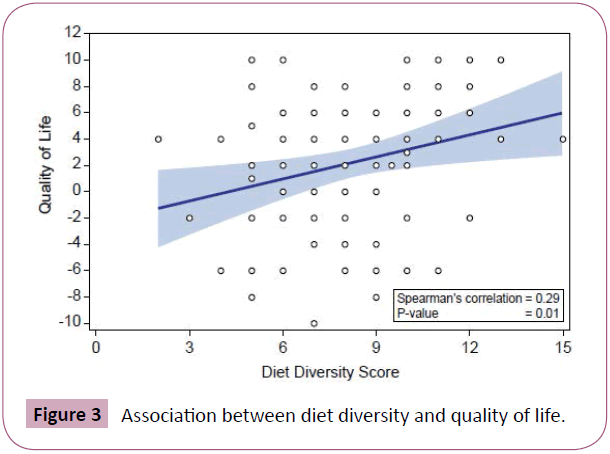
74% of the subjects had hypertension, 42% had anemia, 16% had diabetes and 51% had glaucoma. There were positive associations between Socioeconomic Status (SES) and quality of life (QOL) (p=0.021) as well as E-learning (p=0.04) scores. Drinking bottled water or from a personal borehole was correlated with hypertension (p=0.037). A vitamin-predominant diet correlated positively with number of chronic conditions (p=0.03). There was a positive correlation between diet diversity and quality of life (p=0.01). Only 2% of the patients were E-learning ready.
Conclusion
A higher SES and access to clean water source were associated with hypertension, likely indicative of access to poorer health choices. A diet high in vitamins and minerals was associated with higher numbers of chronic diseases, an indication of poor diet diversity. Majority of cataract patients were not E-learning ready. Education on diet diversity and management of chronic illness could empower patients to improved health practices and potentially improve cataract screening success rates in the community.
Keywords
Cataract; Global Health; E-learning; Education; Quality of Life; Diet diversity
Introduction
South-Eastern Nigeria is a resource-poor area with limited health care access and significant disease burden, critically sustained by humanitarian missions. Chronic diseases are even more burdensome for rural populations due to lower income, longer travel times and delayed presentation to the medical system [1]. Mezu International Foundation (MIF), a non-profit foundation dedicated to international humanitarian services, conducts research during annual medical missions in rural Owerri, Imo State, Nigeria. In 2014 MIF collaborated with the University of Wisconsin Shapiro Program to perform a needs assessment in the community which revealed that cataracts affected 64% of adults above 40-years-old, leading to poor socioeconomic outcome [2]. Although cataracts are among the leading causes of preventable blindness worldwide [3], the prevalence in the working population of this community was unusually high.
The rural community studied is located in Owerri, the capital of Imo State, which has an economy primarily based on agriculture and commerce. In a follow-up study in 2015, MIF investigated risk factors within the community of patients with and without cataracts using a case-control study and revealed that lack of knowledge about cataracts, poor general health knowledge and lack of access to vision care services significantly contributed to poor vision health [4]. This led to collaboration with Combat Blindness International (CBI) in 2016 to provide free cataract surgeries for up to forty-five individuals. However, only ten patients qualified for surgery out of one hundred screened due to the presence of untreated significant medical comorbidities, such as hypertension, diabetes and anemia, making same-day surgeries high-risk.
Comorbidities like uncontrolled diabetes and hypertension have been shown to be risk factors for developing cataracts in the first place [5-7]. Studies have explored the pathological formation of cataract development and Lee et al. reported that hypertension could lead to an alteration of the structural conformation of lens capsule proteins exacerbating cataract formation [8]. There is a linear positive correlation between blood pressure and cataract risk [9,10] as well as longer duration of hypertension and increased risk of cataracts [11]. A national population-based survey of participants 40 years or older in Nigeria, showed that there is an increased prevalence of diabetes in patients with hypertension compared to normotensive individuals (4.4% vs 2.4%) [12]. Metabolic syndrome, anemia and hypercholesterolemia have also been associated with cataracts [13,14]. High dietary salt has been associated with the development of hypertension, the formation of cataracts and accelerating myopic shift while a diet rich in fruits has been shown to decrease the risk of cataracts [15,16]. Additionally, research in a random sampling of patients in a Nigerian community showed that there was significantly reduced albumin concentration in hypertensive patients with cataracts compared to hypertensive patients without cataracts [17]. This suggests a dietary link between the developments of cataracts in patients with hypertension. Chronic medical comorbidities, like hypertension and type 2 diabetes, have been shown to be treated effectively with diet and lifestyle changes [18,19]. Therefore, a community intervention focused on addressing these comorbidities through dietary education could be effective towards preventing cataracts and reduce comorbidity burden. MIF sought to explore whether an electronic educational based intervention could increase the number of patients that qualify for free cataract surgeries.
Early studies on E-learning programs have proven to be useful tools for patient education and a novel way to deliver counseling in the developing world [20]. Mobile phones are prevalent in Africa. In 2010, mobile phone access in rural Africa was reported to be as high as 64% [21]. Mobile applications have been effectively utilized to educate health care workers, provide education and counseling to patients and improve medication compliance and enhance smoking cessation rates in the developing world [22- 24]. Mobile software has also been shown to improve control of chronic conditions commonly associated with cataracts. In patients with diabetes, mobile applications have been shown to lead to statistically significant decreases in Hemoglobin A1c [25]. In addition, mobile education applications have been shown to improve health counseling for maternal health in Nigeria [26]. Mobile-based retinal disease detectors have been shown to offer fast detection and have high accuracy rates of diagnosing retinal diseases including cataracts and are very easy to be operated by any mobile user [27].
While there have been few investigations into the efficacy of mobile applications as an education device in patients with cataracts, studies have shown the efficacy of visual aids and videos which are utilized in E-learning applications. Visual aids were shown to improve patient understanding and retention of information on cataract surgery in rural South India [28] and in the USA [29]. With regards to enhancing efficacy in mobile applications, learning modules with greater technologic accessibility, usability, applicability, learner control and modeling have been shown to have greater success [30]. Although research has shown mobile phones to be prevalent in Africa, there have been no investigations into the prevalence of electronic devices and usability of E-learning applications for cataract patients in Imo State, Nigeria.
This study seeks to investigate dietary habits, Socioeconomic Status (SES), Quality of Life (QOL) and E-learning readiness of cataract patients in order to identify potential targets for educational intervention to facilitate early identification and treatment of chronic medical comorbidities. The findings from this study may be useful to promote better health practices in the community, guide the development of an electronic education program to help manage comorbidities prior to cataract surgery and hopefully influence improved local health policies in the larger community.
Methods
This research followed the guidelines of the Declaration of Helsinki and received Institutional Review Board approval by the Federal University of Technology Owerri (FUTO). Informed consent was obtained by patients and caregivers prior to participation in the study.
Selection of Subjects
During the annual MIF medical mission, a cross-sectional study using a questionnaire was administered to patients aged 45 to 85 years old with a diagnosis of mature cataracts (2+ Nuclear sclerosis or higher), as determined by a licensed optometrist.
Questionnaire design: SES was determined using a scoring tool from prior MIF research [4]. QOL, Diet Diversity and E-learning scores were designed for this study. SES questions were based on questions regarding living situation, transportation and sources of food and water. QOL scores were determined by asking about specific activities of daily living impacted by cataracts. Diet was investigated using a combination of 24-hour recall and specific diet-related questions to come up with a composite “diet diversity” score. Specifically, the 24-hour recall was tabulated based on major food groups like fats/oils, vitamins/minerals, carbohydrates and protein. E-learning readiness explored how useful an electronic learning application (app) would be determining local access to the internet, ability to download an app without assistance, etc. Sample questions used in the survey are shown in Table 1. All subjects underwent detailed medical exams by a licensed physician and ocular exam by a licensed optometrist to identify comorbidities and correlated with data from questionnaires.
| Personal Information • Chief complaint • Head of household • When was your last visit to a doctor? • Where do you obtain medication? • Highest level of education attained by patient |
| Clinical Information • Current medications • Vital signs • Hgb, blood glucose, intraocular pressure • Past medical history |
| Socioeconomic Status • What type of home do you live in? • What personal electronics do you own? • Sleeping Arrangements (number of people per bed) • Main source of drinking water (score highest option given) • What type of toilet facilities does your household use? • Do you receive food from charity or street aid? • How many times a week do you/your family struggle to eat 3 meals a day? • What is your main source of transportation? |
| Quality of Life • Do you have difficulty reading labels on medicine bottles or food labels? • Do you have difficulty reading a newspaper, book, or filling out forms? • Do you have difficulty recognizing people when they are close to you? • Do you have difficulty seeing steps, stairs, or gutters on the street? • Do you have difficulty sewing, knitting, writing letters? • Do you have difficulty pouring a drink from a jug to a cup and drinking it? • Is it hard to see at night or during the day? • Do you go to church or attend meetings by yourself without help? |
| Feasibility of E-Learning Platforms • Do you own a laptop or computer? • Do you own a phone with a touch screen? • Can you download or use an app on a phone without assistance? • Do you have access to the internet at home, at work or at school? • Do you have difficulty looking at and pointing to pictures in a book? |
| Diet Diversity - 24-hour diet recall • How many times do you eat fruit in a typical week? • How many times do you eat chicken, meat, or fish in a typical week? • How many carb items do you eat with your meals? • Where do you mainly get your food from? • What is the greatest barrier preventing you from eating healthy? |
| Subjective Medical Questions • Have you ever been diagnosed with any medical conditions? • How much do you think your diet contributes to these conditions? • How would you rate your overall activity? • Do you smoke or drink alcohol, and if so, how much? • What is the greatest barrier preventing you from seeking medical care? • Which doctor do you go to for your cataracts and for cataract surgery? |
Table 1 Questionnaire design.
Data analysis: The descriptive statistics of all demographics and variables of interest were obtained. Fisher exact tests were used for association of discrete variables with SES, QOL and E-learning categories. For continuous variables, the Wilcoxon rank sum test was used to determine if categories differ between patient’s characteristics. For correlation between the variables, Spearman’s correlation was computed. All tests were 2 sided and a p-value <0.05 was considered statistically significant. SAS software (version 9.4, SAS Institute, Cary, NC) was used for all statistical analyses.
Results
Demographics
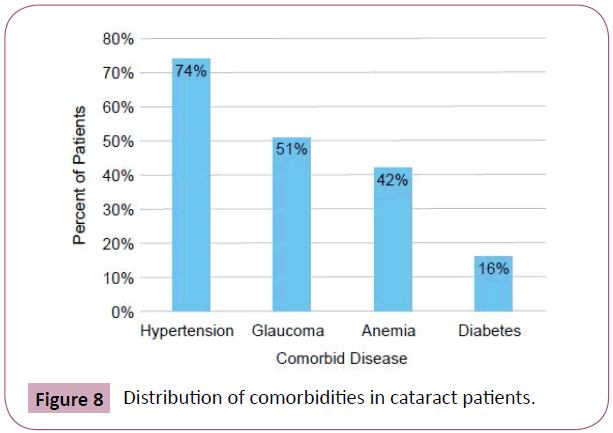
During the four days of the annual medical outreach in rural Owerri, Nigeria, over 2,700 people were seen and 1,500 were screened for cataracts. 115 people met survey criteria, but 32 questionnaires weren’t included in the analysis due to incomplete forms or missing patient information. The analyzed data included 40 males and 43 females aged 45-85 years. 100% of our respondents had at least one additional medical co-morbidity other than cataracts. 82.5% of the respondents reported having 3 or less chronic conditions and 92.5% had 4 or more ongoing diagnoses. 74% of subjects had hypertension (n=61), 42% had anemia (n=35, Hgb <12 g/dL), 16% had diabetes (n=13) and 51% had glaucoma (n=42) (Figure 1).
Socioeconomic status and quality of life assessment
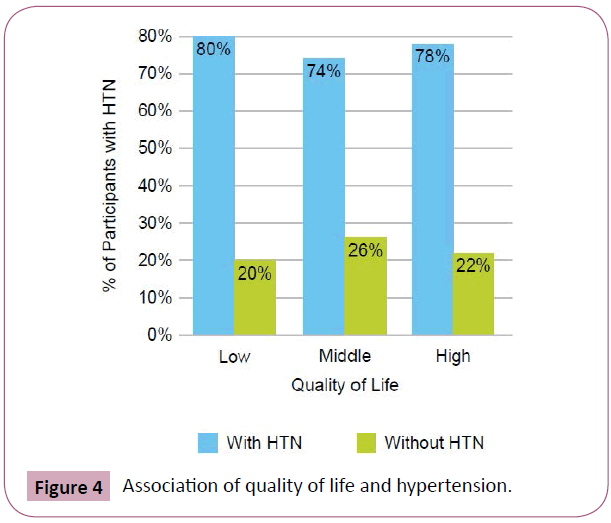
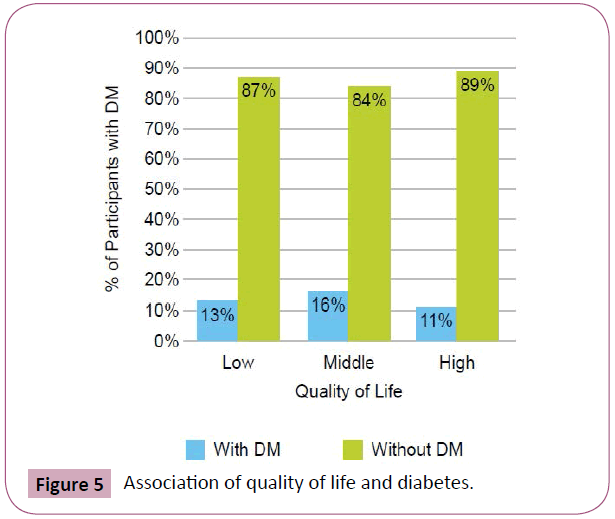
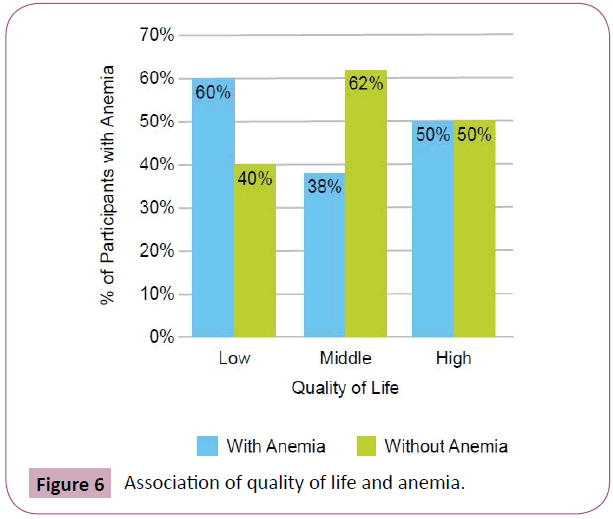
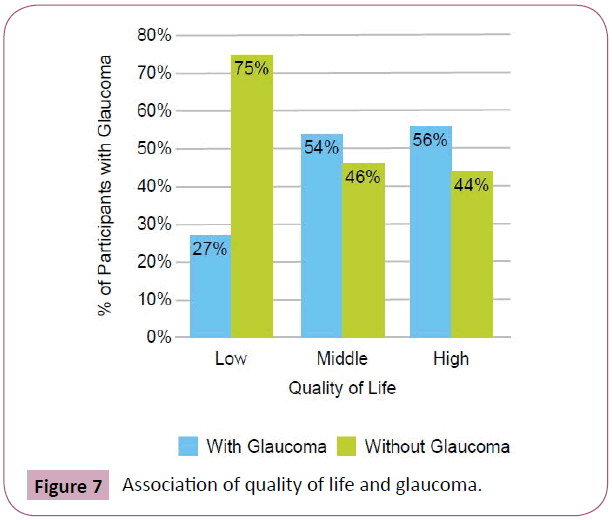
Using the SES tool, drinking bottled water or having a personal borehole was associated with hypertension (p=0.0373) (Figure 2). We found that 71% of subjects who consumed tap water did not have hypertension compared to 48% of subjects who consumed water from other sources. 12% of patients had a low QOL score, 55% had moderate and 33% had high QOL scores. There was no association between QOL scores and percentage of carbohydrates, protein, vitamins/minerals, or fats/oils in the diet (p>0.05). However, there was a positive correlation between QOL scores and diet diversity scores (p=0.01, Spearman’s correlation=0.29) (Figure 3). People with lower QOL scores were not more likely to have anemia (p=0.5172), hypertension (p=0.3298), diabetes (p=0.8242), or glaucoma (p=0.1737) (Figures 4-7). There was a significant positive association between SES and QOL score (p=0.021).
Figure 4: Association of quality of life and hypertension.
Figure 5: Association of quality of life and diabetes.
Figure 6: Association of quality of life and anemia.
Figure 7: Association of quality of life and glaucoma.
Diet diversity
There was a positive correlation between the level of dietary vitamins and minerals and the number of chronic conditions patients had (P=0.03, Spearman’s correlation=0.24) (Figure 8). However, there was no significant correlation between the level of carbohydrates, protein and fats/oils and the number of chronic conditions (P>0.05).
E-Learning readiness
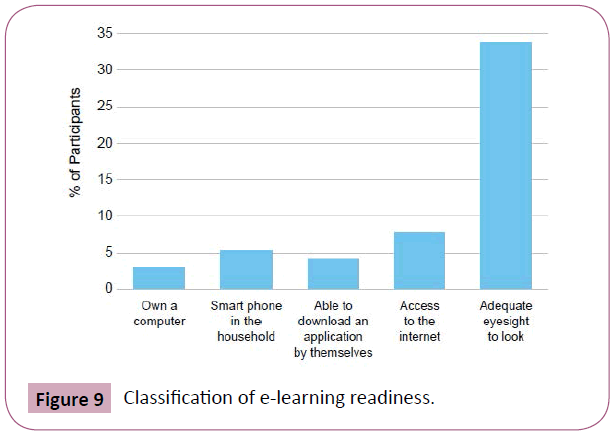
Only 2.4% (n=2) were E-learning ready. 67.5% had adequate eyesight to navigate an E-learning application, however, only 16.9% had access to a computer or smartphone and 15.7% had access to the internet (Figure 9). Lower SES scores were associated with lower E-learning readiness scores (p=0.04).
Association between SES scores, quality of life and E-learning readiness
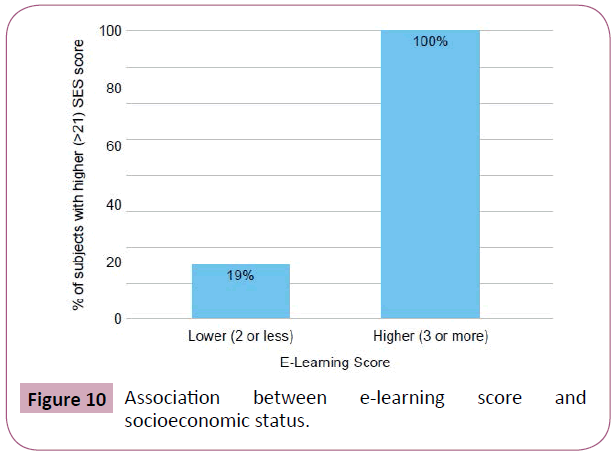
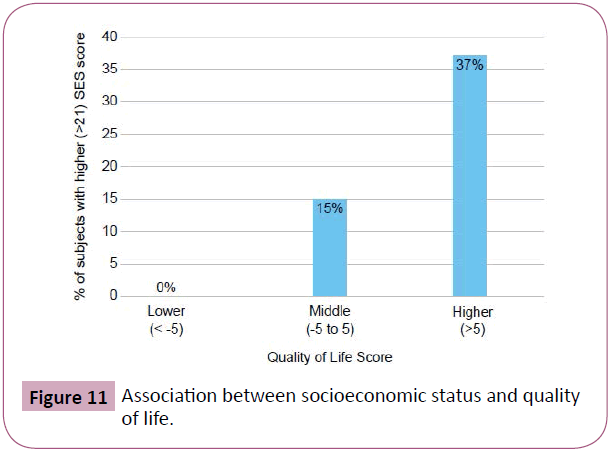
19% of patients who were not E-learning ready had a high SES score (defined as >21). In contrast, 100% of patients who were E-learning ready had a high SES score (Figure 10). 0% patients with a low quality of life score (<-5), 15% of patients with a middle QOL score (-5 to 5) and 37% of patients with a high QOL score (>5) had a high SES score (Figure 11).
Discussion
This study investigates the influence of diet and socioeconomic status on chronic medical conditions in cataract patients in Owerri, Nigeria in order to identify potential educational interventions to identify and manage their medical comorbidities using electronic education methods. These findings indicate a high prevalence of medical comorbidities in cataract populations, their need for health and risk factor education and their lack of E-learning readiness. This information will guide future educational programs within MIF outreach.
Our study showed that patients with access to private boreholes were at higher risk for hypertension. This suggests an association between the ability to afford clean water source processed foods or sugar-sweetened beverages to the prevalence of chronic disease. Research into dietary trends in India and China have shown that calorie-rich foods have been associated with obesity and dietrelated chronic comorbidities and that these changes are most pronounced in urban residents and high-income rural residents [31]. Additionally, some studies have found that increased salinity of groundwater associated with cyclone-induced storm surges is correlated with higher rates of hypertension due to the higher salt intake [32]. Therefore, future studies on access to poor health choices and the chemistry of the well water in the area could further elucidate direct associations between various exposures and the development of chronic conditions like hypertension.
A diet high in vitamins and minerals was found in our study to be associated with higher numbers of chronic diseases. Increased diet diversity has been shown to be associated with higher energy intake, body composition and biochemical markers, such as serum albumin, iron, Vitamin D and folate levels, etc. [33]. These imply that higher vitamin predominance in a diet alludes to lower diet diversity in these populations, contributing to chronic disease. In our study, higher diet diversity was associated with a higher quality of life score and may be a better predictor of patient health in cataract patients.
There was a discrepancy between patient knowledge of their health and awareness of chronic conditions seen in our study. This only underscores the deficiency in long-term medical care and low patient health literacy within the community. One study in Auchi, Nigeria, found that 89% of people with hypertension did not know they could be hypertensive and asymptomatic, while 58% did not know there were risk factors to developing hypertension [34]. Interventions aimed at improving health literacy on chronic illness and patient education on risk factors and diet diversity could facilitate better compliance with followup care and empower patients to adopt better healthier choices.
To utilize E-learning platforms to educate cataract patients on health literacy and management of chronic conditions, E-learning readiness would need to be improved in the community since 97.6% of participants in our study were not E-learning ready. This is consistent with previous studies in Africa, which report poor user familiarity with technology as a barrier to mobile health application success [35]. An important distinction is that while most cataract patients do not have access to the internet or smartphone technology, they are visually able to use an E-learning platform. This is consistent with previous studies which revealed the success of visual aids and tapes in educating patients with cataracts [28,29]. Mobile learning has also been shown to be successful in the visually impaired, using an audio-based device [36]. The most vulnerable were the least E-learning ready in the current study, since people with lower SES scores had a lower QOL and were less E-learning ready. Previous studies have shown that lack of access to internet, electrical instability and familiarity computers with remain barriers for E-learning interventions in Nigeria [37]. Since access and usability are two of the most important factors to successful E-learning, interventions by MIF aimed at improving electronic access and ability in the community, such as by providing iPads and E-learning technology at the MIF clinic site, would be critical to the successful implementation of an app based on management of chronic medical conditions.
Some limitations of this study include potential bias from selfreporting in the setting of a busy clinic, especially during diet recall. The study questionnaire also relied on the use of several translators. Although all translators were college graduates or health care professionals, one cannot rule out the role of cultural and language barriers in the quality of translation. The sample was also limited to the patients who came to the clinic to seek care. E-learning readiness assessed was limited to the age group studied and may not be reflective of the larger community since younger generations could be more E-learning ready and may be useful in assisting older family members in use of proposed educational apps to manage their chronic medical conditions [38].
Conclusion
This study highlighted the need for diet diversity, preventive health culture and improved knowledge of medical conditions in the community irrespective of SES status. Improving E-learning readiness could enable the development of educational aids to increase knowledge of diet diversity and chronic illness. This study revealed the feasibility and challenges of implementing E-learning educational interventions in the rural community and will allow more effective use of E-learning applications to meet the socioeconomic and economic needs of cataract patients and hopefully reduce the chronic disease burden and improve cataract surgery screening rate in the community. This could empower the community to better health practices and hopefully guide regional dissemination of health education and positively influence state-wide health policies.
References
- Janssens W, Goedecke J, de Bree GJ, Aberibigbe SA, Akande TM, et al. (2016) The financial burden of non-communicable chronic diseases in rural nigeria: wealth and gender heterogeneity in health care utilization and health expenditures. PLOS One 11: e0166121.
- Mezu-Ndubuisi OJ, Mezu-Nnabue K, Vo T, Adesina B, Vo L, et al. (2014) Ocular and systemic conditions in a medical mission population in south east nigeria: Transitioning from integrated medical missions to a community medical center model. APHA 142nd Annual Meeting and Expo. American Public Health Association.
- Dineen B, Gilbert CE, Rabiu M, Kyari F, Mahdi AM, et al. (2008) The nigeria national blindness and visual impairment survey. BMC Ophthalmol 8: 17.
- Rolnick K, Buck S, Mezu-Nnabue K, Eickhoff J, Esenwah E, et al. (2017) Influence of socioeconomic status and educational achievement on cataract formation in a rural community in Imo State, South-Eastern Nigeria. Cogent Medicine 4: 1326212.
- Rowe N, Mitchell P, Cumming RG, Wans JJ (2000) Diabetes, fasting blood glucose and age-related cataract: The Blue Mountains Eye Study. Ophthalmic Epidemiology 7: 103-114.
- Tang Y, Wang X, Wang JC, Jin L, Huang W, et al. (2017) Risk factors of age related cataract in a Chinese adult population: The Taizhou Eye Study. Clinical & Experimental Ophthalmology 46.
- Hiller R, Sperduto RD, Ederer F (1986) Epidemiologic associations with nuclear cortical, and posterior subcapsular cataracts. Am J Epidemiol 124: 916-925.
- Ferrie JE, Kivimaki M, Shipley MJ, Smith GD, Virtanen M (2014) Job insecurity and incident coronary heart disease: The Whitehall II prospective cohort study. Atherosclerosis 227: 178-181.
- Horng CT, Lee YL, Wu HC, Lai HY, Hsu JY, et al. (2014) High salt diet induced the rapid myopic shift of cataract formation. Life Science Journal 11: 396-399.
- Guan R, Zhang Q, Zhang R, Zhang X, Li L (2016) Association between dietary fruit intake and age-related cataract: a meta-analysis. International Journal of Clinical and Experimental Medicine 9.
- Phaswana-Mafuya N, Peltzer K, Crampin A, Ahame E, Sokhela Z (2017) Prevalence of self-reported diagnosed cataract and associated risk factors among elderly South Africans. Int J Environ Res Public Health 14: 1523.
- Rim THT, Kim MH, Kim WC, Kim TI, Kim EK (2014) Cataract subtype risk factors identified from the korea national health and nutrition examination survey 2008–2010. BMC Ophthalmol 14: 4.
- Appel LJ, Brands MW, Daniels SR, Karanja N, Elmer PJ, et al. (2006) Dietary approaches to prevent and treat hypertension: a scientific statement from the American Heart Association. Hypertension 47: 296-308.
- Fowler MJ (2010) Diagnosis, classification, and lifestyle treatment of diabetes; clinical diabetes, American Diabetes Association 28: 79-86.
- Kyari F, Tafida A, Sivasubramaniam S, Murthy GV, Peto T, et al. Prevalence and risk factors for diabetes and diabetic retinopathy: Results from the nigeria national blindness and visual impairment survey. BMC Public Health 14: 1299.
- Richter GM, Torres M, Choudhury F, Azen SP, Varma R (2013) Risk factors for cortical, nuclear, posterior subcapsular, and mixed lens opacities: The los angeles latino eye study. Ophthalmology 119: 547-554.
- Sreevinas V, Prabhakar AK, Badrinath SS, Fernandez T, Roy IS, et al. (1999) A rural population based case-control study of senile cataract in India. J Epidemiol 9: 327-336.
- Mukesh BN, Le A, Dimitrov PN, Ahmed S, Taylor HR (2006) Development of cataract and associated risk factors: The visual impairment project. Archives of Ophthalmology 124: 79-85.
- Oladunjoye ZA, Quadri JA, Ojure MA (2017) Assessment of albumin status in hypertensive patients with or without cataract in eyes. American Journal of Biomedical and Life Sciences 5: 73-77.
- Nguyen HQ, Carrieri-Kohlman V, Rankin SH, Slaughter R, Stulbard MS (2003) Internet-based patient education and support interventions: a review of evaluation studies and directions for future research. Comput Biol Med 34: 95-112.
- Kunutsor SJ, Walley J, Katabira E, Muchuro S, Balidawa H, et at. (2010) Using mobile phones to improve clinic attendance amongst an antiretroviral treatment cohort in rural uganda: a cross-sectional and prospective study. AIDS Behav 14: 1347-1352.
- Kallander K, Tibenderana JK, Akpogheneta OJ, Strachan DL, Hill Z, et al. (2013) Mobile health (Mhealth) approaches and lessons for increased performance and retention of community health workers in low- and middle-income countries: A review. J Med Internet Res 15: e17.
- Behera BK, Satish K, Jena SK, Hussain MA, Samal S (2012) Prevalence of hypertension and diabetes mellitus among people seeking cataract surgery in rural South India. Internet Journal of Epidemiology 10.
- West DM (2015) Using mobile technology to improve maternal health and fight Ebola: A case study of mobile innovation in Nigeria. Center for Technology Innovation.
- Osborn CY, van Ginkel JR, Marrero DG, Robard D, Huddleston B, et al. (2017) One drop | mobile on iPhone and apple watch: An evaluation of HbA1c improvement associated with tracking self-care. JMIR Mhealth and Uhealth 5: e179.
- McNabb M, Chukwu E, Ojo O, Shekhar N, Gill CJ, et al. (2015) Assessment of the quality of antenatal care services provided by health workers using a mobile phone decision support application in northern nigeria: A pre/post-intervention study. PLoS One 10: e0123940.
- Bourouis A, Feham M, Hossain MA, Zhang L (2014) An intelligent mobile based decision support system for retinal disease diagnosis. Decision Support Systems 59: 341-350.
- Karan AM, Campbell DJ, Mayer HR (2011) The effect of a visual aid on the comprehension of cataract surgery in a rural, indigent South Indian population. Digit J Ophthalmol 17: 16-22.
- Shukla AN, Daly MK, Legutko P (2012) Informed consent for cataract surgery: Patient understanding of verbal, written, and videotaped information. Journal of Cataract and Refractive Surgery 38: 80-84.
- Noesgaard SS, Ørngreen R (2015) The effectiveness of e-learning: An explorative and integrative review of the definitions, methodologies and factors that promote e-learning effectiveness. Electronic Journal of e-Learning 13: 278-290.
- Popkin BM, Horton S, Kim S, Mahal A, Shuigao J (2001) Trends in diet, nutritional status, and diet-related noncommunicable diseases in china and india: The economic costs of the nutrition transition. Nutr Rev 59: 379-390.
- Butler AP, Hoque MA, Mathewson E, Ahmed KM, Vineis P, et al. (2016) Impact of saline water sources on hypertension and cardiovascular disease risk in coastal Bangladesh. Geophysical Research Abstracts 18.
- Bernstein MA, Tucker KL, Ryan ND, O'Neill EF, Clements KM, et al. (2002) Higher dietary variety is associated with better nutritional status in frail elderly people. J Am Diet Assoc 102: 1096-1104.
- Iyalomhe GBS, Iyalomhe SI (2010) Hypertension-related knowledge, attitudes and life-style practices among hypertensive patients in a sub-urban Nigerian community. J Public Health Epidemiol 2: 71-77.
- Zurovac D, Talisuna AO, Snow RW (2012) Mobile phone text messaging: Tool for malaria control in Africa. PLoS Medicine 9: e1001176.
- Sanchez J, Flores H, Saenz M (2008) Mobile science learning for the blind. Florence: CHI EA ’08: 3201-3206.
- Aminu H, Rahaman S (2014) Barriers thrusting e-learning to the backseat. Nigeria a case study. IEEE Canada International Humanitarian Technology Conference 1-4.
- Quinn CC, Khokhar B, Weed K, Barr E, Gruber-Baldini AL (2015) Older adult self-efficacy study of mobile phone diabetes management Diabetes Technol Ther 17: 455-461.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences