Immunosuppression Associated Sinonasal Ebv B-cell Lymphoma Presenting as Complicated Sinonasal Infection: Challenges in Diagnosis and Treatment Approach
1Department of Ear, Nose and Throat, Royal Hospital for Sick Children, Edinburgh, United Kingdom
2Department of Ear, Nose and Throat, Forth Valley Royal Hospital, Larbert, United Kingdom
- Corresponding Author:
- Rasads Misirovs
MRCS (ENT), Department of Ear
Nose and Throat, Forth Valley Royal Hospital
Larbert, United Kingdom
E-mail: rasads.misirovs@nhs.net
Received Date: August 14, 2018; Accepted Date: September 10, 2018; Published Date: September 17, 2018
Citation: Amir I, Misirovs R, Starritt N (2018) Immunosuppression Associated Sinonasal Ebv B-cell Lymphoma Presenting as Complicated Sinonasal Infection: Challenges in Diagnosis and Treatment Approach. Research J Ear Nose Throat. Vol.2 No.1: 3.
Copyright: © 2018 Amir I, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution and reproduction in any medium, provided the original author and source are credited.
Abstract
We describe a case of sinonasal lymphoma in a child with immunosuppression who presented with symptoms of complicated acute rhinosinusitis with orbital abscess. Despite appropriate medical and surgical therapies, patient developed intracerebral extension. Histopathology confirmed EBV-positive B-cell lymphoma and this was thought to be related to Immunosuppression-Associated Lymphoproliferative Disorders (IALD). Disease progression halted and later regressed with appropriate chemotherapy. Although rare, this case highlights the importance of having high index of suspicion and consideration of all possibilities including lymphoma in immunosuppressive patient. In this report, we also present review of literature relating to IALD with sinonasal manifestation.
Keywords
Rhinosinusitis; Sinonasal lymphoma; Immunosuppression
Introduction
It is well recognized that patients with immunosuppression have a higher risk of developing lymphoproliferative disorders. Immunosuppression associated lymphoproliferative disorders (IALD) usually present in extranodal sites, have rapid clinical progression when untreated, B-cell derived and Epstein Barr Virus (EBV) related [1]. While lymphomas of the sinonasal tracts are uncommon, those associated with IALD are rare [2,3]. In IALD related to post-organ transplant, sinonasal is the most common site of involvement [4]. Due to its nonspecific presentations of clinical signs and symptoms of sinonasal lymphoma, diagnostic delay tends to occur. We report an interesting case of a child with IALDs related sinonasal lymphoma who presented with signs and symptoms of acute rhinosinusitis.
Case Presentation
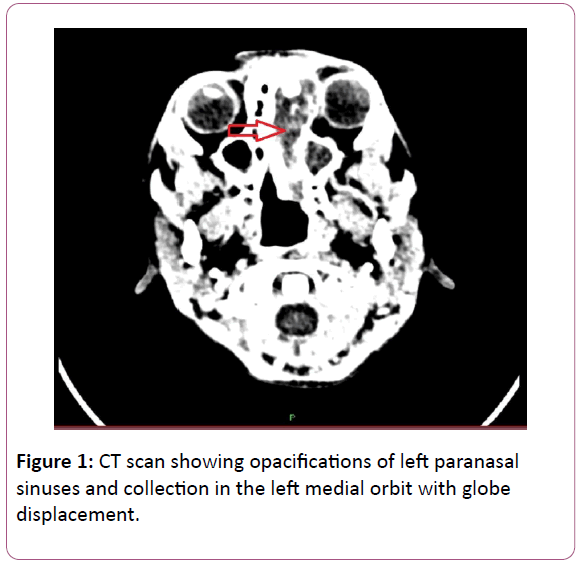
A 9-year old boy presented to the Ear, Nose and Throat (ENT) with a 2-week history of fever, nasal obstruction, rhinorrhoea and left eyelids oedema. At the time of presentation, he was in remission from Acute Lymphoblastic Leukaemia (ALL) which was diagnosed 2 years ago, and was receiving a weekly parenteral methotrexate as a maintenance therapy. He had only just been discharged from hospital with febrile neutropenia 7 days prior to his presentation to ENT. Initial clinical examinations revealed congested nasal mucosa with thick nasal discharge and evidence of pre-septal periorbital cellulitis. He was also found to be neutropenic on admission. A working diagnosis of acute rhinosinusitis with periorbital cellultis was made and intravenous antibiotic therapies with meropenem and gentamicin were commenced. Patient was also started on appropriate topical nasal decongestant, nasal steroid and saline nasal rinse. However, due to lack of clinical improvement after more than 48 hours on medical therapies, a computed tomography (CT) scan was performed. This showed opacifications of left paranasal sinuses and collection in the left orbit with globe displacement Figure 1. Patient underwent an urgent endoscopic drainage of left orbital collection and anterior ethmoidectomy. Intra-operative findings revealed necrotic tissue around the left middle turbinate, dehiscence of lamina papyracea and copious amount of pus from medial orbital cavity. Despite the surgical intervention and resolved neutropenic state, patient continued to experience regular spiking of temperature and showed little clinical improvement.
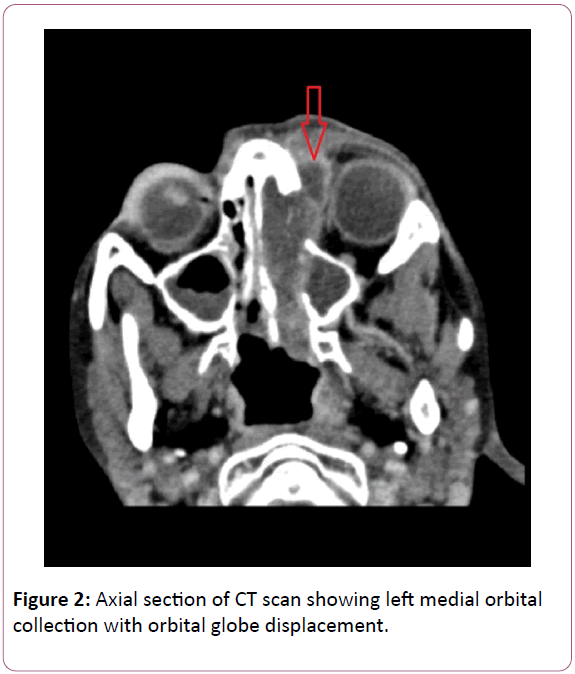
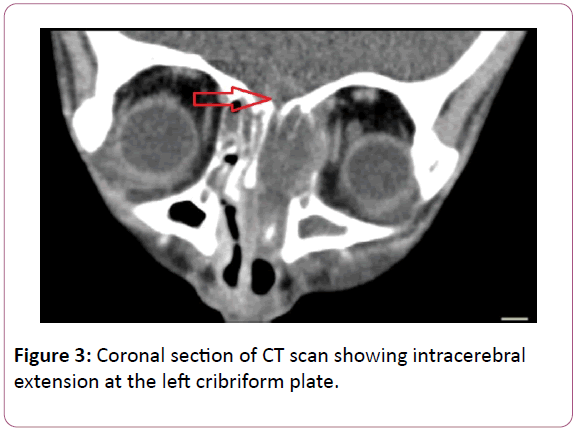
A repeat CT scan imaging performed a couple of days later revealed worsening left orbital collection with very small intracerebral extension at the cribriform plate (Figures 2 and 3). An external drainage of the orbital collection and endoscopic debridement of necrotic sinonasal mucosa were performed. Amphotericin B was also added to cover a possible invasive fungal sinusitis. Patient made a gradual but good recovery following these interventions. Patient’s visual acuity, colour vision and visual field have all returned to normal.
All microbiology cultures taken at intra-operatively were negative. Histopathology examination of left middle turbinate and ethmoid sinus mucosa demonstrated the glandular tissue of the nasal cavity to be extensively infiltrated by a population of large atypical appearing lymphocytes with large pleomorphic nuclei, prominent nucleoli and moderately abundant cytoplasm. There was evidence of EBV infection with the majority of the large cells being positive for EBERs and EBNA-2, and a proportion was positive for LMP-1. The appearances were consistent with an EBV-positive diffuse large B cell lymphoma. In the context of immunosuppression this was thought to be best regarded as falling into the category of the iatrogenic immunosuppression-associated lymphoproliferative disorders (IALDs). Patient underwent parenteral and intrathecal chemotherapy with Rituximab, Vincristine and Cyclophosphamide. Monthly surveillance with magnetic resonance imaging (MRI) scan showed no evidence of disease in the last 12 months since completion of treatment.
Discussion
Immunosuppression-associated lymphoproliferative disorders (IALDs) can occur due to primary immune disorder or acquired immunosuppressive state such as infections with human immunodeficiency virus (HIV), post organ or bone marrow transplantations, or following immunosuppressive therapies [5]. Approximately 30-50% of IALDs are EBV-positive and they tend to occur in extranodal sites, such as the gastrointestinal tract, skin, liver, lung, and kidney. Although, the occurrence of IALDs related lymphoma in the sinonasal is rare [3], sinonasal tract is the most common site in the head and neck IALDs lymphomas in post-transplant paediatric patients [4,6].
Symptoms of sinonasal lymphoma are generally non-specific, and may include recurrent acute rhinosinusitis, nasal obstruction, pain, headache and facial oedema. B symptoms (fever >38°C, nocturnal sweating, and 10% weight loss in six months) occur in majority of the cases [7]. As the disease evolves and progresses, necrosis and bone lysis set in, producing complications such as orbital, skull base and intracerebral involvement. High grade B-cell lymphomas are associated with soft tissue or bony destruction, particularly involving the orbit resulting in associated proptosis [8]. Our patient presented with nasal obstruction, periorbital cellulitis, headache and proptosis in left eye; which were the result of both tumour involvement of anterior skull base and the left orbit, and obstruction of sinuses resulting in acute rhinosinusitis and its complications (periorbital cellulitis and orbital abscess). In this case, patient was initially treated as having a complicated acute rhinosinusitis. A diagnosis of invasive fungal sinusitis was also considered given patient’s immunosuppressive state, clinical history and radiological evidence of bony destruction and therefore amphotericin B was started empirically [9]. There has been at least 2 reported cases of IALD of sinonasal region mimicking a fungal sinusitis [10,11]. CT scan is important in evaluating the involvement of and extent of destruction of the sinuses, the skull base, and the orbit. MRI scan is also recommended where erosion of the cribriform is suspected [11]. Skull base involvement associated with sinonasal lymphoma is rare; however their occurrences have been commonly associated with immunosuppressed patients [8]. A biopsy is essential for an accurate diagnosis. As the surface of B-cell lymphomas tends to be associated with necrotic tissue, definitive diagnosis can be challenging. Therefore, repeated and deep biopsies are often required. This difficulty may explain why the diagnosis is often delayed or missed. In our experience, the definitive diagnosis in our patient was only achieved after a repeat biopsy following an endoscopic debridement. The diagnosis of large B-cell lymphoma is based on the histologic appearance of the lesion and the immunophenotype of the atypical cells, and immunohistochemistry is mandatory [12]. In our case, the histopathological findings of ethmoid sinus and middle turbinate are consistent with an EBV-positive diffuse large B cell lymphoma, which is most like related to IALDs. In addition to the above investigations, imaging of the thorax and the abdominal cavity should also be performed for staging of the disease [13]. Bone marrow biopsy may be required in order to rule out any marrow involvement. Systemic chemotherapy is the foundation of treatment and therefore early diagnosis and staging are essential. Due to non-specific nature of sinonasal lymphomas presentation, published case-series reported that approximately two-thirds have intermediate-grade disease at initial presentation [9,14]. It is therefore associated with poor survival outcome with estimated 71% of patients in a case series of paediatric sinonasal lymphoma died within 3 years [15]. Late presentation does not just impact the disease stage and the prognosis but also the morbidity associated with tumour burden such as in this case from orbital and intracranial complications.
Conclusion
IALDs related B-cell EBV lymphoma of sinonasal is uncommon but an important diagnosis to consider in immunocompromised patients. Early diagnosis and appropriate treatment are essential to achieve optimal outcomes, and it is important that otolaryngologists be familiar with its presentation and management.
References
- Oertel SH, Riess H (2002) Immunosurveillance, immunodeficiency and lymphoproliferations. Recent Results Cancer Res 159: 1-8.
- Baier G, Volter C, Steigerwald I, Muller J, Schwager K (2005) Malignant paranasal sinus tumors. Diagnosis, therapy and results. HNO 53: 957-965.
- Pui CH, Evans WE (2006) Treatment of acute lymphoblastic leukemia. N Engl J Med 354: 166-178.
- Herrmann BW, Sweet SC, Molter DW (2005) Sinonasal posttransplant lymphoproliferative disorder in pediatric lung transplant patients. Otolaryngol Head Neck Surg 133: 38-41.
- Carbone A, Gloghini A, Dotti G (2008) EBV-associated lymphoproliferative disorders: Classification and reatment. Oncologist 13: 577-585.
- Herrmann BW, Sweet SC, Hayashi RJ, Canter CE, White FV, et al. (2006) Otolaryngological manifestations of posttransplant lymphoproliferative disorder in pediatric thoracic transplant patients. Int J Pediatr Otorhinolaryngol 70: 303-310.
- Yen TT, Wang RC, Jiang RS, Chen SC, Wu SH, et al. (2012) The diagnosis of sinonasal lymphoma: A challenge for rhinologists. Eur Arch Otorhinolaryngol 269: 1463-1469.
- Cuadra GI, Proulx GM, Wu CL, Wang CC, Pilch BZ, et al. (1999) Sinonasal lymphoma: A clinicopathologic analysis of 58 cases from the Massachusetts General Hospital. Am J Surg Pathol 23: 1356-1369.
- Park AH, Muntz HR, Smith ME, Afify Z, Pysher T, et al. (2005) Pediatric invasive fungal rhinosinusitis in immunocompromised children with cancer. Otolaryngol Head Neck Surg 133: 411-416.
- Hatten KM, Loevner LA, Palmer JN, Adappa ND (2012) Isolated sinonasal posttransplantation lymphoproliferative disorder: A clinical and radiographic invasive fungal sinusitis look-a-like. ORL J Otorhinolaryngol Relat Spec 74: 339-342.
- Gordon AR, Loevner LA, Sonners AI, Bolger WE, Wasik MA (2002) Posttransplantation lymphoproliferative disorder of the paranasal sinuses mimicking invasive fungal sinusitis: Case report. Am J Neuroradiol 23: 855-857.
- Zagolski O, Dwivedi RC, Subramanian S, Kazi R (2010) Non-Hodgkin's lymphoma of the sino-nasal tract in children. J Cancer Res Ther 6: 5-10.
- Ng YY, Healy JC, Vincent JM, Kingston JE, Armstrong P, et al. The radiology of non-Hodgkin′s lymphoma in childhood: A review of 80 cases. Clin Radiol 49: 594-600.
- Hanna E, Wanamaker J, Adelstein D, Tubbs R, Lavertu P (1997) Extra nodal lymphomas of the head and neck. A 20-year experience. Arch Otolaryngol Head Neck Surg 123: 1318-1323.
- Yi JS, Cho GS, Shim MJ, Min JY, Chung YS, et al. (2012) Malignant tumors of the sinonasal tract in the pediatric population. Acta Otolaryngol 132: 21-26.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences