Hemorrhage under Antivitamins K: A Location Like No Other
Amine Salmi*
Department of Medical and Surgical Emergencies, University Hospital Center Mustapha, Algiers, Algeria
- *Corresponding Author:
- Amine Salmi
Department of Medical and Surgical Emergencies
University Hospital Center Mustapha
Algiers, Algeria
Tel: 0663503399
E-mail: salmi86amine@gmail.com
Received Date: Nov 17, 2017; Accepted Date: Nov 19, 2017; Published Date: Nov 25, 2017
Citation: Salmi A (2017) Hemorrhage under Antivitamins K: A Location Like No Other. J Surgery Emerg Med 1: 9
Copyright: © 2017 Salmi A. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Accidents with oral anticoagulants have been widely described, but epidural localization remains exceptional, leading to a misleading clinical picture, the main consequence of which is delayed treatment. The objective of this presentation is to bring out the diagnostic difficulties that arise, to draw the clinician's attention to this location based on a questioning quality. The notion of taking anticoagulants in a patient with neck pain unusual with neurological signs (sensory or motor) is very suggestive, then justify a rapid radiological exploration of the spine. We report the case of a 34-year-old woman with a mechanical prosthesis in the mitral position (St. Jude), on oral anticoagulant acenocoumarol (Sintrom®) who consults for cervicalgia, overdose with antivitamin K. A cervical scan showed limited epidural hematoma between C3-C6.
Keywords
Epidural hematoma; Vitamin K antagonists; Misleading location; Diagnostic and Therapeutic emergency
Introduction
Oral anticoagulants are usually prescribed for various indications. Their wider use has been noted in recent years, probably exposing more frequent hemorrhagic complications. If, typically, the bleeding is digestive, genitourinary or intracranial, the epidural hematoma, exceptional or even underestimated localization, is rarely reported in the literature. It is characterized by its diagnostic problems on the one hand and by the possible evolutionary complications, in case of late management. Spinal imaging, CT scanning or magnetic resonance imaging (MRI) are very interesting diagnostic tools.
Case Presentation
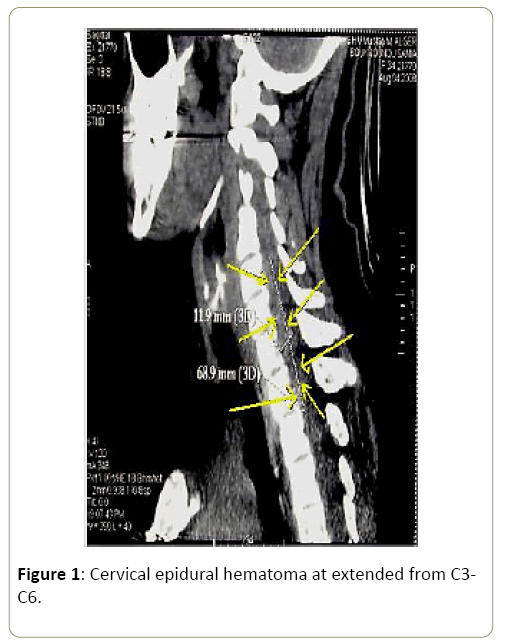
A young 34 years old patient, treated chronically with acenocoumarol (Sintrom®) at a dose of 2 mg per day following a mitral valvuloplasty rather 3 months (St. Jude type), admitted for persistent neck pain, continuous, sudden onset, disobedient to banal analgesic. Physical examination revealed a conscious patient, febrile, without deficit signs or sensory disorders, who complained of severe neck pain, and any attempt to mobilize the cervical spine was impossible. Laboratory tests were not anomalies, outside an INR 7.The brain scan was normal. A cervical spinal cord injury was suspected and CT of the cervical spine then concluded, cervical epidural hematoma at extended from C3-C6 (Figure 1).
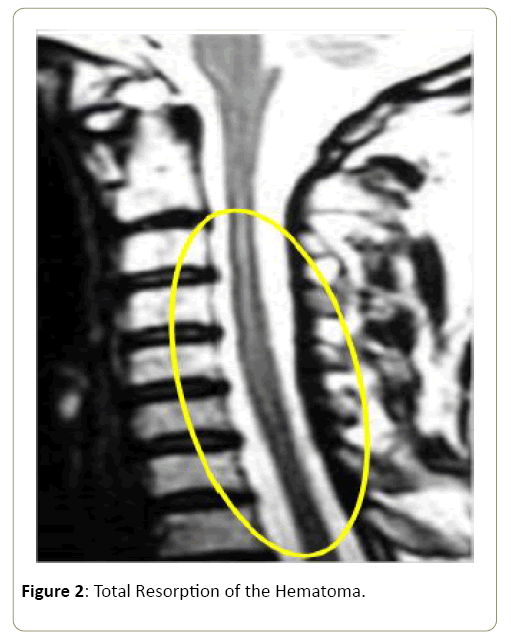
All data, clinical and radiological, and absence of any notion of trauma, were in favor of a spontaneous cervical extramedullary hematoma complicating anticoagulation. Anticoagulant therapy was stopped, and the therapeutic management was symptomatic corrected INR (INR <1.5), development of a cervical neck brace for analgesic and clinical monitoring, biological and radiological. The clinical outcome was favorable with disappearance of neck pain and cervical spinal MRI performed a month later, revealed a total resorption of the hematoma (Figure 2).
Discussion
The epidural hematomas (EH) pose a diagnostic problem, given the rarity of this complication, and to our knowledge, we report in this observation the third case of spontaneous EH to overdose on vitamin K, after the two cases cited by Hentschel [1]. The headquarters of the spinal hematoma perished predominates to cervicothoraciques regions, highly mobile regions including the clinical signs depend on two essential elements are: the location and the size of the hematoma [2,3]. On the etiological, our patient had no obvious cause for the fall of the TP, and outside any context of trauma, are the causes of EH [4]:
• The coagulopathy and anticoagulant therapy (30%),
• The arterio-venous malformations (4%),
• Tumor cases (4%),
• 30-64% of cases, no cause is found.
• The risk factors are
• Ankylosing spondylitis,
• Bone and ligament aberrations
Thus, 7 cases in EH in the child with hemophilia [5] have been identified, although hit is a rare complication (2.2 to 7.8%) it is necessary to think about the pain of acute spinal installation and this even before the onset of neurological deficit, and treatment should be started at the end of the extension limit. Thrombolytic [6] may be responsible for this complication and 12 cases were reported, with an installation period, neurological disorders, averaged 12 hours. Treatment [7] of EH can be surgical or conservative, depending on the clinical examination, and are considered good prognostic factors, the following:
• A short time between the installation unrest and surgical time (less than 8 hours),
• Low compression force,
• A partial deficiency before surgery
Conservative treatment [8] has been tried, and 7 cases of epidural hematoma, which resolved were identified. In our case, the treatment was based on the rapid antagonism of vitamin K antagonists to obtain an INR (International Normalized Ratio) less than 1.5 associated with analgesic treatment. The patient was referred to her treating physician for the reintroduction of her anticoagulant treatment. In these situations, it is often possible to restart the antivitamin K 2 weeks after the hemorrhagic event.
The prognosis of EH depends on four essential elements [9]:
• The presence of neurological disorders
• The severity of neurological disorders
• Rapid diagnosis
• And speed of the treatment
Evolutionarily, healing is possible:
It is total in 83% of cases if the deficits in complete, and in 25% of cases in the presence of a complete deficit [10].
Conclusion
The perimedullary hematoma, despite its rarity as a current practice, needs special attention, since the prognosis is directly related to the therapeutic precocity. Careful interrogation and imaging are the diagnostic pillars.
References
- Hentschel SJ, Woolfenden AR, Fairholm DJ (2001) Resolution of Spontaneous Spinal Epidural Hematoma without Surgery: Report of Two Cases. Spine 26: E525-E527.
- Beatty RM, Winston KR (1984) Spontaneous Cervical Epidural Hematoma: A Consideration of Etiology. J Neurosurg 61: 143-148.
- Lin IY, Chong C (2004) Non Traumatic Spinal Epidural Hematoma Mimicking A Brainstem Stroke. Annals of Emergency Medecine 44: 183-184.
- Domenicucci M, Ramieri A, Ciappeta P, Delfini R (1999) Nontraumatic Acute Spinal Subdural Hematoma: Report of five cases and Review of the literature. J Neurosurg 91: 65-73.
- Chretieonnet-Bara C, Guet A, Balzamo E (2001) Hematome Epidural Chez L’enfant Homophile: Difficultes Diagnostiques. Arch Pediatr 8: 828-833.
- Cohen J, Ginsberg H, Emery D, Scwartz M (1998) Fatal Spontaneous Spinal Epidural Hematoma Following Thrombolysis For Myocardial Infarction. Surg Neurol 49: 520-523.
- Groen R, August H, Van Alphen M (1996) Operative Treatment of Spontaneous Spinal Epidural Hematomas: A study of the factors determining postoperative outcome. Neurosurgery39: 494-509.
- Hentschel S, Woolfenden AR, Fairholm DJ (2001) Resolution of Spontaneous Spinal Epidural Hematoma without Surgery: Report of Two Cases. Spine 26: E525-E527.
- Otsu I, Merril D (2004) Epidural Hematoma after Epidural Anesthesia: A Case Report of Non Surgical Management. Acute pain 4: 117-120.
- Cullen D, Bogdanov E, Htut N (2004) Spinal Epidural Hematoma Occurrence in the Absence of Known Risk Factors: A Case Series. J Clinical Anesthesia 16: 376-381.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences