Food Bee Honey versus Conventional Antiseptic in Local Management of Acute Infected Wounds
1Department of General Surgery, Benha Teaching Hospital, General Organization for Teaching Hospitals and Institutes, Egypt
2Department of General Surgery, Faculty of Medicine, Zagazig University, Egypt
3Department of Histology and Cytology, Faculty of Veterinary Medicine, Zagazig University, Zagazig, Egypt
- *Corresponding Author:
- Mohamed Aly Elhorbity
Department of General Surgery
Benha Teaching Hospital
General Organization for Teaching Hospitals and Institutes, Egypt
Tel: +00201005137060
E-mail: mohamed_elhorbity@hotmail.com
Received Date: Feb 15, 2018; Accepted Date: Feb 28, 2018; Published Date: Mar 08, 2018
Citation: Elhorbity MA, Gertallah LM, Mansour MI, Arafa AS, Mahmoud BR, et al. (2018) Food Bee Honey versus Conventional Antiseptic in Local Management of Acute Infected Wounds. J Surgery Emerg Med 1: 15
Copyright: © 2018 Elhorbity MA, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Honey is a popular sweetener and a common household product throughout the world. It is nonirritant, nontoxic, easily available and cheap. It has been used from ancient times as a method of accelerating wound healing. During twentieth century, it was reported that honey as having good antimicrobial properties along with therapeutic potential in wound healing. Methods: Between Feb 2014 and December 2016, a total of 100 patients; aged between 20 and 60 years old, 56 male and 44 female patients, complaining from acute wound infection, all patients after proper investigation and proper surgical treatment with adequate drainage and or debridement under general anesthesia. Local management of the wound was done either by daily wound dressing with food bee honey or local antiseptic povidone iodine 10% solution. All patients were randomized into 2 groups. Group A (honey local dressing of acute infected wound of 50 patients) and group B (povidone iodine local dressing of acute infected wound of 50 patients). Results: Marked clinical improvement was seen in most cases of group A, using food honey local treatment of wounds, compared with group B using povidone iodine in daily wound dressing and most of the wounds were closed, clean and free of infection from 10 days to 6 weeks, except 2 cases of diabetic foot wounds needed another local drainage and debridement under general anesthesia followed by complete wound healing after about 4 weeks on daily honey local treatment and one case of diabetic male 52 years old was complaining of neglected perianal abscess complicated with scrotal Fournier gangrene and after surgical drainage and debridement and excision of about 50% of scrotal skin due to Fournier gangrene, complete healing of both, perianal wound and scrotal wound in about 8 weeks on daily wounds dressing with honey. In group B, povidone iodine local wound treatment, wound healing and closure from 2 weeks to 8 weeks, except 4 cases of diabetic foot wounds, two from them needed another local drainage and debridement under general anesthesia after 2 weeks from the first drainage and needed about 4 to 6 weeks for wound healing from the second drainage, and another two cases changed to chronic wounds and complete healing after about 3 months from the second wound drainage and debridement. Conclusion: The present investigation can conclude that the bee honey has significant efficacy in local management of infected wound compared with local conventional antiseptic povidone iodine, as shortly time of healing, economic, more patient satisfy, comfort with less pain, final better wound scare formation that is more cosmetics compared with povidone iodine.
Keywords
Bee honey; Antiseptic; Wound; Dressing; Povidone iodine
Introduction
Several studies all over the world have reported the emergence of multi-resistant bacteria in human and veterinary medicine. For this reason, honey was repurposed for wound care since it offers a good alternative to conventional antimicrobial drugs [1-4]. Honey is a viscous concentrated solution of sugars produced by bees (Apis mellifera) that collect and process the blossom nectar (flowers or floral honey) or sweet juices on certain plant species (honeydew or forest honey). The ancient Egyptians, Assyrians, Chinese, Greeks and Romans employed honey for wounds and diseases of the gut [5].
Zumla and Lulat [6] investigated that the ancient Egyptians used honey as a wound treatment as early as 3000 BC and it has been found in Egyptian tombs. Its prescription for a standard wound salve discovered in the Smith papyrus (an Egyptian text dating from between 2600 and 2200 B.C.).
Most microorganisms do not grow in honey, so sealed honey does not spoil, even after thousands of year [7].
It quickly reduces the inflammation, swelling, pain, and unpleasant odors. It also facilitates separation of necrotic tissue without the need for debridement [8]. The acidity of honey further aids in antibacterial activity [9].
It has been reported to contain about 200 substances. Honey is composed primarily of fructose and glucose but also contains fructo-oligosaccharides and many amino acids, vitamins, minerals and enzymes [10].
More recently, honey has been reported to have an inhibitory effect to around 60 species of bacteria including aerobes and anaerobes, gram-positives and gram-negatives [11]. An antifungal action has also been observed for some yeasts and species of Aspergillus and Penicillium [12].
The clearing of infection seen when honey is applied to a wound may reflect more than just antibacterial properties. There is an established research show that the proliferation of peripheral blood B-lymphocytes and T-lymphocytes in cell culture is stimulated by honey at concentrations as low as 0.1%; and phagocytes are activated by honey at concentrations as low as 0.1% [13].
Aim of Work
The present study was performed to investigate, evaluate and assess the role of honey in local management of acute infected wounds compared with conventional use of local antiseptic dressing; povidone iodine.
Subjects and Methods
Between Feb 2014 and December 2016, a total of 100 patients, complaining from acute wound infection, all patients after proper investigation and proper surgical treatment with adequate drainage and or debridement under general anesthesia. Local management of the wound was done either by bee honey or local antiseptic povidone iodine 10% solution daily wound dressing. All patients were informed about the purpose of the study with ethical aspects and a written consent was done.
All patients were randomized into 2 groups. Group A (honey local dressing of acute infected wound of 50 patients) and group B (povidone iodine local dressing of acute infected wound of 50 patients).
Inclusions criteria
All the patients included in this study aged between 20 and 60 years old, 56 male and 44 female patients. All wounds are acute infected wounds postoperative and after surgical drainage and debridement after proper investigations including radiology; X-ray and ultrasound and routine laboratory; random blood sugar, complete blood picture, renal and liver functions and coagulation profile. Wound size minimum 3 cm and maximum 20 cm. All patients received intravenous antibiotic third generation cephalosporin ceftriaxone, one gram each 12 hour from the start, until the patients clinically no systemic manifestation of infection (fever, chills, or any organ dysfunction) and laboratory normal leucocytic count, except one case of Fournier gangrene in group A, received ciprofloxacin 400 mg slowly intravenous each 12 hour, plus metronidazole 500 mg slowly intravenous each 8 hour in addition to ceftriaxone, until the patients clinically no systemic manifestation of infection (fever, chills, or any organ dysfunction) and laboratory normal leucocytic count. Oral antibiotics are based on bacterial wound culture report. Pus swap culture and sensitivity done weekly from the wound until the result clarified sterile wound (no growth) in the 2 groups.
Exclusion criteria
We excluded all patients with known hypersensitivity to any bee honey products or iodine products, patients with diabetic foot osteomyelitis or arterial or venous insufficiency and also, patients with autoimmune disease.
Technique of local wound dressing
In group A, the wound is washed first with normal saline 0.9% and cleaned from any pus or debris then putting the honey till filling the wound cavity and covering the edges (about 20 to 30 ml in wound surface area 10 x 5 cm) then cover the wound with sterile dressing (gauze, cotton pads and bandage).
In group B, the wound is washed first with normal saline 0.9 and cleaned from any pus or debris then washing with 10% povidone iodine solution and sterile gauze soaked with it putted in the wound cavity (about 10 to 15 ml in wound surface area 10 x 5 cm) then sterile dressing (gauze, cotton pads and bandage).
Assessment of the wound healing status in all patients
Wound dressing done daily in all patients in the 2 groups, and the observation of the wound healing status were assessed each 10 days, clinically via verbal pain scale from zero to 3 (Figure 1), the patient describe pain as no pain, mild pain, moderate pain, severe pain from period of wound dressing to the another day. Meanwhile, laboratory done via white blood cells counts and neutrophils, and wound swab culture for bacteriological examination, and finally measurement of the size of the wound closure with ruler compared with the original size from the start. Any adverse reaction to honey or povidone iodine were recorded.
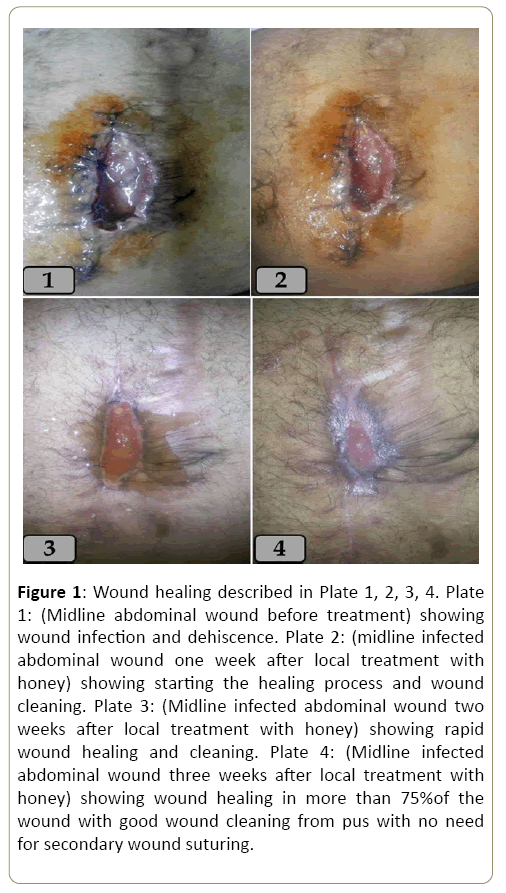
Figure 1: Wound healing described in Plate 1, 2, 3, 4. Plate 1: (Midline abdominal wound before treatment) showing wound infection and dehiscence. Plate 2: (midline infected abdominal wound one week after local treatment with honey) showing starting the healing process and wound cleaning. Plate 3: (Midline infected abdominal wound two weeks after local treatment with honey) showing rapid wound healing and cleaning. Plate 4: (Midline infected abdominal wound three weeks after local treatment with honey) showing wound healing in more than 75%of the wound with good wound cleaning from pus with no need for secondary wound suturing.
All the wounds in the 2 groups were examined and assessed daily for the cleanliness from infection, the process of wound healing and time of complete wound healing. Laboratory complete blood picture were done each three day until white blood cells return to normal. In addition, each two weeks, the wound swab culture and sensitivity were done until the wound became sterile and evaluation the difference between the 2 groups.
Results
Marked clinical improvement was seen in most cases of group A, with honey local treatment of wounds, and most of the wounds were closed, clean and free of infection from 10 days to 6 weeks, except 2 cases of diabetic foot wounds needed another local drainage and debridement under general anesthesia followed by complete wound healing after about 4 weeks on daily honey local treatment and one case of diabetic male 52 years old was complaining of neglected perianal abscess complicated with scrotal Fournier gangrene and after surgical drainage and debridement and excision of about 50% of scrotal skin due to Fournier gangrene, complete healing of both, perianal wound and scrotal wound in about 8 weeks on daily wounds dressing with honey with no need to another stage operation of scrotal skin grafting as we planned before using honey.
In group B, povidone iodine local wound treatment, wound healing and closure from 2 weeks to 8 weeks, except 4 cases of diabetic foot wounds, two from them needed another local drainage and debridement under general anesthesia after 2 weeks from the first drainage and needed about 4 to 6 weeks for wound healing from the second drainage and another two cases changed to chronic wound and complete healing after about 3 months from the second wound drainage and debridement.
Swabs from wounds of group A, wounds with bacteria became sterile within one to two weeks, while in group B, wounds became sterile within one week to four weeks. Laboratory leucocytic count became normal within 3 to 7 days in wounds of group A, while in group B, within 3 to 10 days.
Regarding, sensation of comfort and pain in the 24 hours after local wound treatment, patients with group A, feel more comfort and less pain sensation according to verbal pain scale from zero to 3 (Figure 2). Only 3 patients in group A, described localized stinging sensation and moderate pain during wound dressing with honey, and rapidly improvement short time after dressing.
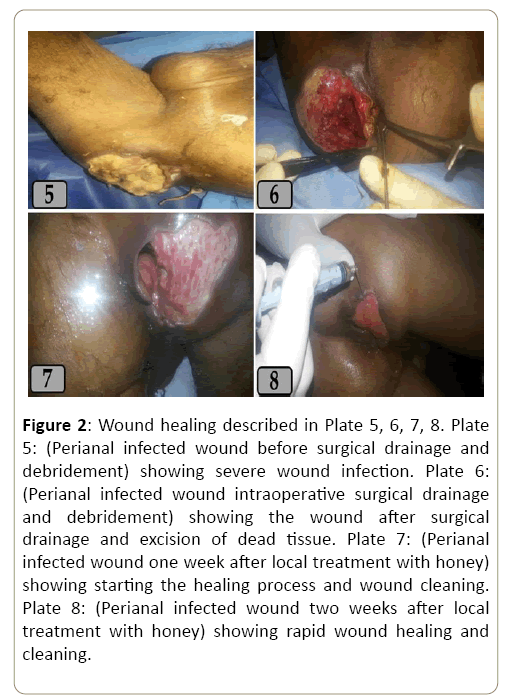
Figure 2: Wound healing described in Plate 5, 6, 7, 8. Plate 5: (Perianal infected wound before surgical drainage and debridement) showing severe wound infection. Plate 6: (Perianal infected wound intraoperative surgical drainage and debridement) showing the wound after surgical drainage and excision of dead tissue. Plate 7: (Perianal infected wound one week after local treatment with honey) showing starting the healing process and wound cleaning. Plate 8: (Perianal infected wound two weeks after local treatment with honey) showing rapid wound healing and cleaning.
Patients with group A received oral non-steroidal diclofenac tab 50 mg/8 h for 3 days and tramadol 50 mg slowly IV when needed, compared with 7 days oral non-steroidal diclofenac tab 50 mg/8 h and also, tramadol 50 mg slowly IV when needed in group B.
Finally, we clarified marked excellent effect of bee honey in the process of the wound healing and marked elimination of wound infection in short period compared with using povidone iodine.
Discussion
In two observational groups, complete healing was gained in group A of patients treated with honey within 10 days to 6 weeks, a good improvement was observed in most of the cases, while in case of group B of patients treated with povidone iodine, healing was gained within 14 days to 8 weeks where patients reported improvement but with longer time. Furthermore, the bee honey is highly effective in local management of infected wound compared with local conventional antiseptic povidone iodine, shortly time of healing, economic, cost effective about 50%, more patients satisfies, comfort with less pain, final better wound scare formation that is more cosmetics compared with povidone iodine.
It has been for a long time that honey is using to accelerate the wound healing [14]. It is an excellent adjuvant for acceleration of wound healing, is widely accepted in folk medicine. The exact molecular mechanism of wound healing using honey is yet to be elucidated. Studies showed that it act by reducing ROS levels, besides this it exert antibacterial activity and low pH and high free acid content may assist wound healing [15]. However, several recommendations are made regarding appropriate wound dressing with honey. Type of wound and degree of severity will effects efficacy. It should cover and extend beyond the wound margins. Better results occur when applied on dressing than on wound. All the cavities should be adequately filled with honey and occlusive dressing applied to prevent oozing from the wound [16] (Figure 3). The effect of honey in wound healing is the result of the combined effects of chemical debridement of dead and devitalized tissues from ulcers by catalase, absorption of edema by the hygroscopic properties of honey, the promotion of granulation and epithelization from wound edges, the bactericidal and fungicidal properties of honey, its nutritional properties and the production of hydrogen peroxide [16]. Honey comprises 40% glucose, 40% fructose, 20% water, with organic acids, vitamins, enzymes, and minerals; it has specific weight of 1.4 and pH of 3.6 [16,17]. The treatment with honey is simple and in expensive, and honey need not to be sterile as it already possesses a bactericidal property [14], because of its high viscosity it forms a physical barrier, creating a moist environment which appears to be helpful and accelerates wound healing [18].
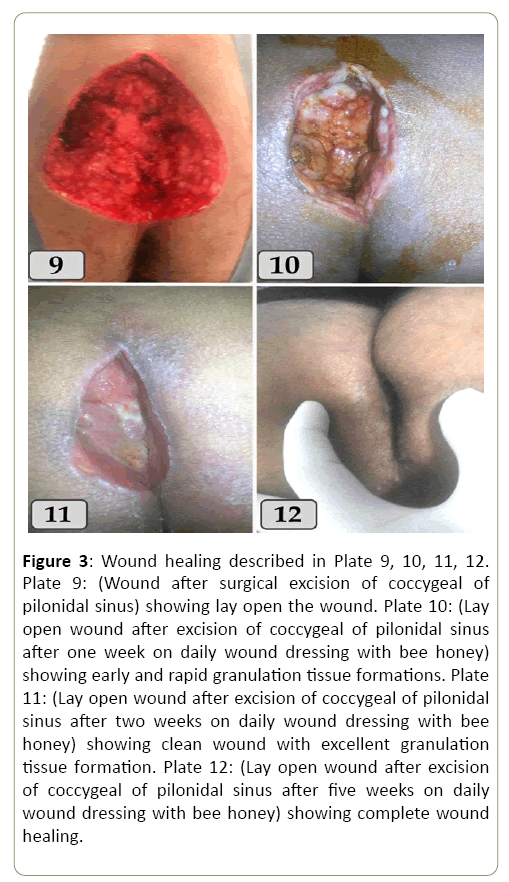
Figure 3: Wound healing described in Plate 9, 10, 11, 12. Plate 9: (Wound after surgical excision of coccygeal of pilonidal sinus) showing lay open the wound. Plate 10: (Lay open wound after excision of coccygeal of pilonidal sinus after one week on daily wound dressing with bee honey) showing early and rapid granulation tissue formations. Plate 11: (Lay open wound after excision of coccygeal of pilonidal sinus after two weeks on daily wound dressing with bee honey) showing clean wound with excellent granulation tissue formation. Plate 12: (Lay open wound after excision of coccygeal of pilonidal sinus after five weeks on daily wound dressing with bee honey) showing complete wound healing.
Moreover, Medhi et al. [19] concluded that application of honey has significant efficacy in treatment of wounds as it demonstrated in observational studies but in controlled clinical studies observed, its modest efficacy, so clinicians and researchers should look for clinical evidence and more randomized double blind trials that will provide the scientific evidence to support the use of honey in wound healing management. So base on above observations it can be concluded that topical application of honey is very useful for the treatment for wound healing.
Conclusion
From our results, we can conclude that the bee honey is highly effective in local management of infected wound compared with local conventional antiseptic povidone iodine, shortly time of healing, economic, cost effective about 50%, more patients satisfies, comfort with less pain, final better wound scare formation that is more cosmetics compared with povidone iodine.
References
- Basualdo C, Sgroy V, Finola MS, Marioli JM (2007) Comparison of the Antibacterial Activity of Honey from Different Provenance against Bacteria usually Isolated from Skin Wounds. Vet. Microbiol 124: 375-381.
- George NM, Cutting KF (2007) Antibacterial Honey (Medi-Honey™): In-Vitro activity against Clinical Isolates of Mrsa, Vre and other Multiresistant Gram-Negative Organisms Including Pseudomonas Aeruginosa. Wounds 19: 231-236.
- Mohapatra DP, Thakur V, Brar SK (2011) Antibacterial Effcacy of Raw and Processed Honey. Biotechnol Res Int 6.
- Vica ML, Glevitzky M, Dumitrel GA, Junie LM, Popa M (2014) Antibacterial activity of different natural honeys from Transylvania, Romania. J Environ Sci Health 49: 176-181.
- Al-Jabri AA (2005) Honey, Milk and Antibiotics. Afr J Biotechnol 4: 1580-1587.
- Zumla A, Lulat A (1989) Honey-A Remedy Rediscovered. J Royal Soc Med 82: 384-385.
- Geiling N (2013) The Science behind honey's Eternal Shelf Life.
- Molan PC (2006) The Evidence Supporting the use of Honey as a Wound Dressing. Int J Low Extrem 5: 40.
- Efem SEE (1988) Clinical observations on the Wound healing Properties of Honey. Br J Surg 75: 679-681.
- Chow J (2002) Probiotics and Prebiotics: A Brief Overview. J Ren Nutr 12: 76-86.
- Molan PC (1992) The Antibacterial Activity of Honey. The nature of the Antibacterial activity. Bee World 1: 5-28.
- Brady NF, Molan PC, Harfoot CG (1997) The Sensitivity of Dermatophytes to the Antimicrobial Activity of Manuka Honey and other Honey. Pharm Sci 2: 1-3.
- Abuharfeil N, Al-Oran R, Abo-Shehada M (1999) The Effect of Bee Honey on the Proliferative Activity of Human B and T Lymphocytes and the activity of Phagocytes. Food Agric Immunol 11: 169-177.
- Efem SE (1998) Clinical Observation on the Wound Healing Properties of Honey. Br J Surg 75: 679-681.
- Phuapradit, Sarapola N (1992) Topical Application of Honey in Treatment of Abdominal Wound Disruption. Aust NZ J Obstetrics Gynaecol 32 4: 381-384.
- Gethin G, Cowman S (2005) Case Series of Use of Manuka Honey in Leg Ulceration. Int Wound J 1: 10-15.
- Van den Berg AJ, van den Worm E, van Ufford HC, Halkes SB, Hoekstra MJ, et al. (2008) An in Vitro Examination of the Antioxidant and Anti-Inflammatory Properties of Buckwheat Honey. J Wound Care 4: 172-78.
- Bansal V, Medhi B, Pandhi P (2005) Honey A Remedy Rediscovered and its Therapeutic Utility. Kathmandu Univ Med J 3: 305-309.
- Medhi B, Puri A, Upadhyay S, Kaman L (2008) Topical Application of Honey in the Treatment of Wound Healing: A Metaanalysis, JK Science 4: 166-169.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences