Extra-Pulmonary and Pulmonary Tuberculosis among Elderly Peruvian Patients
Jeel Moya-Salazar1,2*, Altea RM Nemolato3, Jonathan Samán4, Israel A Pasco5 and Jose Maria Olivo-López6
1National Teaching Hospital Madre Niño San Bartolomé, Lima 51001, Peru
2Faculty of Health Science, Continental University, Huancayo 64001, Peru
3Department of Biological Sciences, Vanvitelli University, Caserta 811000, Italy
4CENEX, Hipólito Unanue National Hospital, Lima 51001, Peru
5Faculty of Health Science, Norbert Wiener University, Lima 51001, Peru
6Service of Microbiology, National Institute of Child Health, Lima 51001, Peru
- Corresponding Author:
- Moya-Salazar J,
Hospital Nacional Docente Madre Niño San Bartolomé, Lima 51001, Peru
Tel: +33635562148
E-mail: jeelms@outlook.com
Received date: March 29, 2018; Accepted date: April 30, 2018; Published date: May 05, 2018
Citation:Jeel Moya-Salazar, Altea RM Nemolato, Jonathan Samán, Israel A Pasco and Jose Maria Olivo-López (2018) Extra-Pulmonary and Pulmonary Tuberculosis among Elderly Peruvian Patients. J Immunol Microbiol Vol.2 No.1:4
Copyright: © 2018 Moya-Salazar J, et al. This is an open-access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original author and source are credited.
Abstract
Background: Tuberculosis (TB) is one of the main causes of mortality worldwide and in Peru, it represents a national health priority since >35 thousand people suffer from the disease annually. The aim of the study was to evaluate the frequency of extra-pulmonary (EPTB) and pulmonary Tuberculosis (PTB) among older patients (≥ 90 years old) during 2015-2017 in a poor district with a high-prevalence of TB in Lima, Peru.
Methods and findings: This cross-sectional study evaluated elderly patients of El Agustino district (population density of 15 416.19 hab/km²). The samples included were from the TB Control Program (PCT), from outpatient clinics, and patients over 90 years old of both sexes. All the extra pulmonary specimens (gastric aspirate, pleural fluid, etc.) were obtained in the respective services and were sent immediately for analysis. The culture medium for TB was Ogawa-Kudoh agar and the conventional sputum smear method was used. Of the 584 patients included 296 (51%) were women (93 ± 3 years). In 408 (69.7%) sputum and 177 (30.3%) extra pulmonary samples, we diagnosed TB in 16 (2.74%). Of the 11 (1.8%) cases of PTB, only two had positive results in both sputum smear and culture. The 103% of patients with EPTB had no diagnosis or previous treatment. Of the 5 (0.9%) cases with contaminated culture, 3 (0.5%) came from the Emergency Service.
Conclusion: This first Peruvian study on TB in the elderly population showed a low frequency, with more cases reported in men aged between 90 years without prior treatment.
Keywords
Tuberculosis; Extra-pulmonary tuberculosis; Elderly; Mycobacterium tuberculosis; Peru
Abbreviations
TB: Tuberculosis; EPTB: Extra-Pulmonary and Pulmonary Tuberculosis; PTB: Pulmonary Tuberculosis
Introduction
Tuberculosis (TB) is one of the main causes of mortality worldwide that leads to important problems of Global Public Health. In 2016, 6.5 million new cases were reported worldwide, and TB mortality is estimated at 3% per year [1]. There is a marked difference in the epidemiology of TB between highincome countries and low-and-middle-income countries (LMIC). In the LMIC, TB causes >90% of cases, mainly affecting vulnerable populations, such as children and the elderly (≥ 65 years) [2,3]. In the Americas region, there are >260,000 TB cases annually, 60% of cases correspond to Brazil, Peru, Mexico, and Haiti. Peru is the third country with the highest TB incidence rate (101 per 100 000 inhabitants) and has high multidrug-resistant TB (MDR-TB) burden [1,4]. In Peru, TB is not only a national problem but is a health priority due to its high rates of MDR-TB [1]. In Lima, the capital of Peru, the district of El Agustino is one of the districts with the highest incidence of pulmonary TB (PTB) with >70% positive sputum smears [5,6]. Extra pulmonary tuberculosis (EPTB) means that infection caused by M. tuberculosis, which affects tissues and organs external to the lungs; this is 20-25% of cases of tuberculosis disease [7]. Extra pulmonary TB represented 15% of the 6.3 million incident cases that were notified in 2016 [1]. Regardless of the ethnic group and the age group, the world population is aging, and there are high estimates of the elderly population for the year 2050 [8]. As mentioned since the 70s, TB in older patients is a challenge for healthcare systems and governments around the world [2,9-11]. Recently, high rates of TB and unusual clinical manifestations have been reported in the elderly Hispanic population, which, as in other regions, leads to problems in the diagnosis of this disease that has high mortality rates [12-15]. It has long been recognized in high-income countries that older people are very vulnerable to the development of tuberculosis; however, this situation differs from the reality of healthcare programs of the LMIC [3].
Seventy-five percent of elderly cases include PTB, and both PTB and PTB have a considerable increase in their incidence and mortality as they get older. To demonstrate the significant frequency of TB in the elderly population, highlighting the distribution of EPTB and PTB, we focused this study towards a "very-old" population (≥ 90 years), since it represents a forgotten group without previous studies, and because the guidelines for the clinical-epidemiological management of TB do not include regulations to address this community group of progressive increase [8,16,17]. The aim of the study was to evaluate the frequency of extra-pulmonary and pulmonary Tuberculosis among older patients (≥ 90 years) during 2015-2017 in a poor district with a high-prevalence of TB in Lima, Peru.
Method
A non-experimental, prospective cross-sectional study was designed and developed at Hipólito Unanue National Hospital in Lima, Peru. The study had the approval of the Committee of Ethics and Research from the Research Support Department of the external institution (HONADOMANI SB-2018). Lima is divided into 43 districts, El Agustino is a district of downtown Lima in the historic center of the city (12°4′0″S, 77°1′0″W). This district has one of the highest rates of TB prevalence among the population, has about 200 thousand inhabitants, and its population density is one of the highest in Lima (15 416.19 hab/km2) [18,19]. Concerned about the high rates of mortality due to TB in this district, the Ministry of Health of Peru has a center of excellence for the diagnosis of TB, where the study was conducted.
Processing of the sample
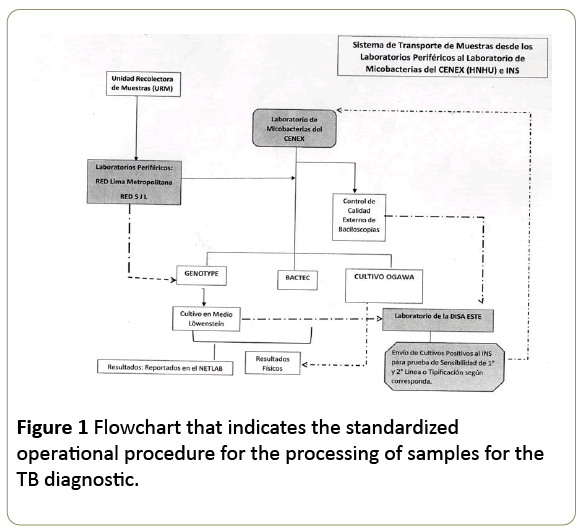
The samples included in this study were from: the TB control Program (PCT) and the outpatient clinics of the hospital, and patients over 90 years old of both sexes. The samples with extensively drug-resistant TB (XDR-TB) or Multidrug-resistant TB (MDR-TB) schemes were not included. All the samples were derived from the Microbiology Area and Department of Research for the diagnosis and treatment of the TB by the Standardized Operational Procedure (SOP) (Figure 1).
All patients attending the diagnostic service for Tb will compulsorily obtain an application from the attending physician after their consultation, to include them in the free tb control program. in the case of extra pulmonary specimens such as gastric aspirate, pleural fluid, cerebrospinal fluid, etc., the samples were obtained in the respective services (i.e., neurology) of the hospital and were sent immediately for analysis in the laboratory. All the patients were included in the sample-registry for the bacteriological research of TB with its own and standardized code of the institution.
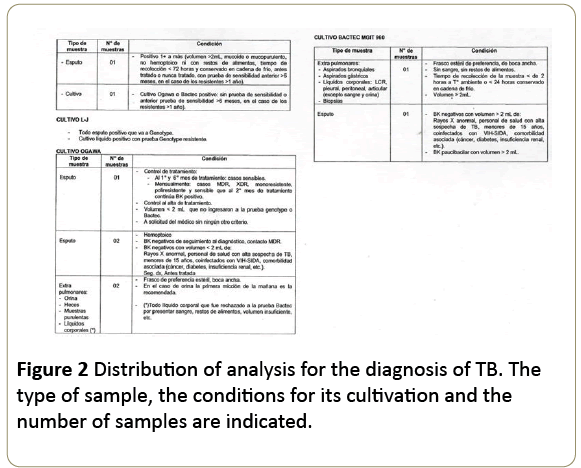
All the samples were evaluated with the criteria and the conformity of the Smear-processing area - called in Spanish Área de Baciloscopía - (level II) and culture area (Level III). In each, the quality of the samples was evaluated and under their conformity, they are processed according to the protocols established for its corresponding diagnosis (Figure 2).
For sputum smear and culture of TB, reagents were used that had strict internal quality control (by the health staff of the hospital) and external quality control (performed by the National Institute of Health of Peru), respectively. The conventional sputum smear method was used as before reported [20]. The culture medium for TB was Ogawa-Kudoh agar (Merck, Darmstadt, Germany), which followed the international requirements of several institutions [21-23].
Technical data collection and statistical analysis
Data coding was performed from MS-Excel 2010 (Redmond, USA) (laboratory database) to EPIDAT v4.1 (Xunta de Galicia, Spain) for Windows. Descriptive statistics and non-parametric Spearman correlation were used. The data processing was performed considering a confidence interval of 95% and a pvalue <0.05 as statistically significant. Statistical analysis was performed with IBM SPSS v20.0 (Armonk, USA) for Windows.
Results
We included 584 patients analysed during the study period whose average age was 93.1 ± 2.9 years (CI95% 92.8 to 93.3). Two hundred and ninety-six (51%) were women whose average age (93 ± 2.9) was significant to the group of 288 men (93 ± 2.8) (p<0.001). of the total cases, we included 408 (69.7%) sputum samples and 177 (30.3%) extra pulmonary samples. Among patients with extra pulmonary samples, 217 (37.1%) were women, 198 (33.8%) of these had no prior treatment (first diagnosis), while 152 (26%) of the 191 (32.6%) men did not receive treatment (Table 1).
| Characteristics | Normal | Tuberculosis | Total | |
|---|---|---|---|---|
| PTB* | EPTB | |||
| Sex | ||||
| Women | 289 (49.5) | 4 (0.7) | 2 (0.34) | 296 (50.7) |
| Men | 279 (47.7) | 7 (1.2) | 3 (0.5) | 288 (49.3) |
| Age (Years) | ||||
| 90-99 | 549 (94.1) | 11 (1.8) | 4 (0.7) | 564 (96.6) |
| >100 | 19 (3.2) | --- | 1 (0.2) | 20 (3.4) |
| Treatment | ||||
| BT** | 46 (7.9) | 2 (0.34) | 1 (0.2) | 49 (8.4) |
| NT | 488 (83.5) | 9 (1.5) | 3 (0.5) | 500 (85.6) |
| NR | 34 (5.8) | --- | 1 (0.2) | 35 (6) |
| Study Period | ||||
| 2015 | 198 (33.9) | 8 (1.4) | 4 (0.7) | 216 (36) |
| 2016 | 175 (30) | 2 (0.34) | 1 (0.2) | 180 (30.8) |
| 2017 | 191 (32.7) | 1 (0.2) | --- | 194 (32.2) |
| Type of sample | ||||
| Sputum | 397 (68) | 11 (1.8) | --- | 408 (69.8) |
| Gastric aspirate | 95 (16.3) | --- | 3 (0.5) | 98 (16.8) |
| Pleural Liquid | 35 (5.9) | --- | --- | 35 (5.9) |
| Bronchial aspirate | 24 (4.3) | --- | 1 (0.2) | 26 (4.5) |
| Post bronchial aspirate | --- | --- | 1 (0.2) | 1 (0.2) |
| Urine | 4 (0.7) | --- | --- | 1 (0.7) |
| Stool | 2 (0.34) | --- | --- | 2 (0.34) |
| Others ¶ | 10 (1.7) | --- | --- | 10 (1.7) |
Table 1: Baseline findings in Peruvian patients with Extrapulmonary and pulmonary Tuberculosis during the 2015-2017 trienniums. *Diagnosis with both sputum smear and culture are included. **Includes patients with previous diagnosis and treatment control. ¶ We included the 3 (0.5) sample of the cerebrospinal fluid, 2 (0.34) of the acetic acid serous fluid and a sample (0.2) of tracheal aspirate, pericardial biopsy & endotracheal tube. Abbreviations: EPTB: Extra Pulmonary Tuberculosis; PTB: Pulmonary Tuberculosis; NT: Never Treated; BT: Before Treated; NO: No Report.
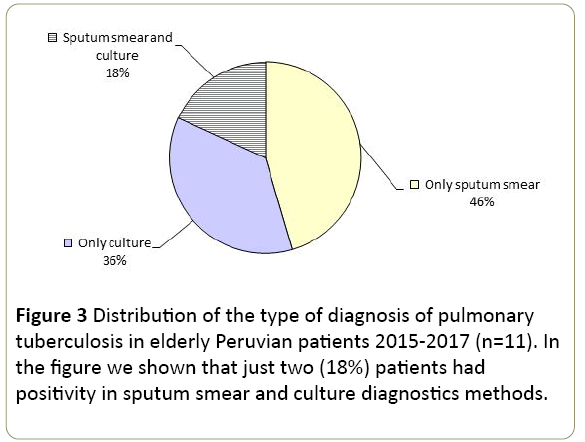
TB was diagnosed in 16 (2.74%) patients. One patient >100 years presented with EPTB in gastric aspirate. One hundred percent of patients with EPTB had no diagnosis or previous treatment. Four (0.7%) patients were admitted to the hospital in the Emergency Service due to various complications, resulting in the diagnosis of EPTB. Three (0.5%) of the samples reported bloody samples and 2 (0.34%) patients had smear-positive (result 2++ and 4 AFB/100 Fields) and respectively contaminated and positive culture. The bronchial samples had a negative X-ray result. We report between 1 (0.2%) and 6 (1%) colonies in culture medium (average 3.5 colonies). The age of patients did not show significant differences (p>0.05). We identified 11 (1.8%) cases of PTB and only in 2 positive results were obtained in sputum smear and culture (Figure 3). Almost all, two (0.34%) patients had previous treatment, but only one had a positive result with sputum smear. The samples were mucopurulent (0.9%), muco-salivary (0.5%), salivary (0.34%) and bloody (haemoptysis) (0.2%). Of the two (0.34%) patients with PTB who were admitted by emergency, both were diagnosed only with smear microscopy. One patient had a negative smear and positive X-rays (2++) for TB. The average of isolated colonies was 4.6 ± 3 colonies (range 2 to 6 colonies). The diagnostic results with sputum smear were in the range of 6 AFB/100 fields to 3 (+ ++).
Five (0.9%) patients had contaminated results, one with smear-positive (2++) specimen from gastric aspirate. All these contaminated samples were from patients of ninety years and corresponded with samples of bronchial aspirate (0.5%) and sputum, urine and gastric aspirate (these three with 0.2%). Three (0.5%) contaminated samples came from the Emergency Service. The sputum sample volume was 1.54 ± 1 ml (range: 0.5 to 6 ml). No correlation was found between the contaminated samples and the sample volume (p=0.102). There was a significant difference between the periods of study (p=0.01) and between the diagnoses per year (p=0.008).
Discussion
This first Peruvian study on TB in the elderly population showed a low frequency, with more cases reported in men aged between 90 years without prior treatment. The main strength of our study is that it was the first Peruvian study focused on people over 90 years of age with pulmonary and extra pulmonary TB in a centre of excellence for the diagnosis of TB. The main limitation of this study is that we did not have access to the molecular results (Expert® MTB/RIF, Gen expert Omni®, both Cepheid, US) of drug resistance data, or other complementary tests such as X-rays, biochemical parameters, etc., for all patients included in the study. Another limitation was that we do not monitor patients during treatment.
As a result of the diagnosis and treatment of 153 million people during 2000-2016, the rate of TB in countries with high incomes was reduced. However, in the LMIC there are still limitations in the prevention and control of TB and difficulties in including population groups at risk, such as the elderly. The Lima Metropolitan area is responsible for approximately 82% of MDRTB cases and 93% of XDR TB cases in Peru; however, in many peri-urban and rural areas, TB rates have not yet been fully estimated [24]. In general, Peru has contradictoriness between its high rate of MDR-TB (estimated at 6.3% of new cases) and its success in treatment [1].
Despite Peru's leading economic growth, ~ 40 000 people suffer from TB. These populations live in infectious foci, as in the district of El Agustino, with low sanitary maintenance, and in a constant transmission of diseases, such as TB [1,5,6,25]. Moreover, this district has a high population density which has had progressive changes since 1981 (19 781.5 inhabitants/km2), 1993 (12 456.5 inhabitants/km2), to 2018 (>19,800 inhabitants/ km2) [19,26]. This situation of population increase, mainly provincial migrant population, could promote overcrowding since this district does not possess the necessary resources for the prevention of the disease and is considered a poor district within a low-income country.
The systemic manifestations of aging (biological, immunological, metabolic, nutritional changes, etc.) currently constitute barriers to prevent TB. Also, these are the risk factors for the development of the disease in the elderly. In a recent review of the state-of-the-art of TB in Peru, it has been described that during 2015, 11% of the total TB cases corresponded to people ≥ 65 years, mainly males [27]. However, in El Agustino district it has been reported that TB is more frequent in young adults (~ 33 years), males, who have a low general perception of health [28]. Our study showed that 2.74% of the elderly ≥ 90 years had TB, mainly PTB, with males being the most affected. This would represent an approximate annual 1.8% if it is estimated with the total positive cases of the hospital (7962 cases of annual TB approx.) [6,16].
It has been noted that patients >50 years have 51% of the Disability- Adjusted Life Years by TB [3] and we can infer for this that veryelderly patients will surely have high mortality rates. Because TB in the elderly is rarely considered in the health context of LMICs, this age group may be severely affected by TB and is possibly being neglected nowadays. For example, in Peru, the National TB guide lacks protocols on the management, diagnostic considerations or treatment of elderly people with TB and therefore, urgently needs to incorporate new strategies organized to meet the criteria of a clinical-practice guide useful and appropriate to reality [14,15,29,30].
Regarding the age of involvement by TB, a previous review showed that the most affected age group are adults between 18-40 years old, although more than a third correspond to patients ≥ 50 years [27,28,30]. The limitations in the screening and inclusion of elderly patients with TB may be because asymptomatic patients are not being included because they do not present classic signs of TB, to problems with sputum smear and culture, due to the difficulty in obtaining samples by the patients, organic complications of age and low priority as a group target in the district. Due to the objectives of the study, we could not determine the site of TB infection in the elderly, but we know that all patients live in their homes with their relatives. TB cases have been reported in nurses homes [2,14], in hospitalized elderly [30] and in non-hospitalized (uninstitutionalized) patients where they have been shown to participate in the chain of transmission [12]. Furthermore, the evidence suggests that hospitalized elderly are at greater risk of reactivation of latent TB.
Regarding the diagnosis of TB in the elderly, we showed a manageable diagnosis because one sample had a low amount of bacilli in the sputum analysis and few samples were hemoptitized (0.2%), which could be explained by Perez--Guzman's previous meta-analysis [31] that indicates that the low frequency of samples with hemoptysis is related to low pulmonary cavitary infiltration and depends on the immune response [32]. Likewise, a low frequency of positive smear has been reported in the elderly [12,31]. The analysis of EPTB is much more accurate than the diagnosis of sputum smear. The Ogawa-Kudoh method is an excellent tool for diagnosing pulmonary TB. It is easy to perform, requires less biosafety equipment, has a low cost, and has good sensitivity for detecting of M. tuberculosis [33]. Eighty percent of TB cases affect the lungs, our findings agree with these previous results on the adult population [10]. If the diagnosis of PTB in this group of patients presents with difficulty, being usually a problem recognized only in post-mortem studies, the EPTB is a problem that has not been evaluated and therefore almost unknown in this group of patients.
We must consider two other relevant aspects of TB: 1) the most of TB isolations in the elderly are drug-sensitive strains [2]. However, Peru has high rates of MDR-TB and in Lima metropolitan area this is evidenced by high rates in the districts of El Agustino and El Callao, where these patients probably have acquired MDR-TB. 2) In this district not only high TB rates have been reported, but there are cases of contagion by health personnel (0.2% cases per triennium) [34]. However, the rate of this occupational disease in the National Hospital Hipolito Unanue coincides with the risk of infection in high-income countries [35].
As in other regions, the socioeconomic level influences the relationship between TB in the elderly and in poor populations; this is a key factor for their control. Further, there is an increase in the global old age rate, which could explain TB rates in various countries [10-14]. The treatment of TB in the elderly is at high risk of adverse drug reactions, these reactions must be monitored to avoid serious complications [10,12]. Another problem is that the difficulty in handling the treatment of these patients is often suspended for short periods due to the unavailability of the patient, adverse reactions, little insistence that the patient takes the pill, exhaustion of the therapy by the relatives and the patient, in others. Adherence to treatment depends on knowledge about TB [36]. These patients require the support of their families during antituberculous treatment, and must also feel supported by their government and community [37]. Further, immediate considerations are required for several types of clinical evaluation systems [17] and diagnosis could fail with these patients [12,21-24].
Conclusion
In conclusion, this first Peruvian study on TB in the elderly population (≥ 90 years old) showed a low frequency in the District of El Agustino. Likewise, we report more cases in men of 90 years old without previous treatment.
Acknowledgement
We thank all the staff of the Hospital for their invaluable work and help in the development of this study.
Funding
Self-funded for the authors.
Conflicts of Interests
The authors declare that there are no conflicts of interest.
References
- World Health Organization (2017) Global tuberculosis report 2017. Geneva.
- Yoshikawa TT, Rajagopalan S (2001) Tuberculosis and aging: A global health problem. Clin Infect Dis 7: 1034-1039.
- Negin J, Abimbola S, Maraisbd BJ (2015) Tuberculosis among older adults time to take notice. Int J Infect Dis 32: 135-137.
- Pan American Health Organization (2012) Tuberculosis in the Americas: Regional report 2012. Epidemiology, Control and Financing. Washington.
- Bonilla AC (2008) Situation of tuberculosis in Peru. Acta Méd Peruana 25: 163-170.
- Ramírez-Lapausa M, Menéndez-Saldaña A, Noguerado-Asensio A (2015) Extrapulmonary tuberculosis (Abstract in English). Rev Esp Sanid Penit 17: 3-11.
- Unite Nations (2015) World Population Ageing. New York: Department of Economic and Social Affairs Population Division.
- Davies PD (1994) Tuberculosis in the elderly. J Antimicrob Chemother 34: 93-100.
- Gisselbrecht M (2004) Tuberculosis in elderly people in institutions. Rev Resp Dis 21: 106-113.
- Cruz-Hervert LP, García-García L, Ferreyra-Reyes L, Bobadilla-Del-Valle M, Cano-Arellano B, et al. (2012) Tuberculosis in ageing: high rates, complex diagnosis and poor clinical outcomes. Age Ageing 41: 488-495.
- Cantalice Filho JP, Bóia MN, Sant`Anna CC (2017) Analysis of the treatment of pulmonary tuberculosis in elderly patients at a university hospital in Rio de Janeiro, Brazil. J Bras Pneumol 33: 691-698.
- Toyota M, Sasaki Y (2010) The issue of tuberculosis in the elderly in Japan. Kekkaku 85: 881-94.
- Shipovalova MA, Svistunova VP, Malkova MV (2013) Tuberculosis of the lungs of the elderly and old age at the stage of inpatient management of patients. Med Healthc 2: 19-22.
- Ministry of Health (2006) Technical Health Standard for the Control of Tuberculosis. Lima: MINSA, General Directorate of People's Health, National Health Strategy for Prevention and Control of Tuberculosis.
- Cordeiro CE, Rosário Souza ICC, Penha de Oliveira SMI, Araújo SN, Santos das Neves OE (2003) Epidemiological, clinical and evolutionary aspects of tuberculosis in the elderly.
- Chaves CE, Carneiro RS, Oliveira-Santos MIP, Araújo Sarges ND (2017) clinical and evolutionary aspects of tuberculosis among elderly patients of a university hospital in Belém. Pará Rev Bras Geriatr Gerontol 20: 47-58.
- United Nations (2015) World urbanization prospects. The 2014 revision. New York: Department of Economic and Social Affairs, Population Division (ST/ESA/SER.A/366).
- National Institute of Statistics and Informatics (INEI) (2015) Population estimates and projections. Lima: INEI.
- Sequeira de Latini MD, Barrera L (2008) Manual for the bacteriological diagnosis of tuberculosis: Standards and technical guide. Part I Bacilloscopy. Washington, D.C: Pan American Health Organization (PAHO/PAHO).
- Rivas C, Coitinho C, Dafond V, Corbo M, Baldjian M (2010) Performance of the Ogawa-Kudoh method for isolation of mycobacteria in a laboratory with large-scale workload. Rev Argentina Microbiol 42: 87-90.
- Asencios Sl, Quispe TN, Vásquez CL (2012) Manual for the external quality control of culture media for the bacteriological diagnosis of tuberculosis. Lima: Ministry of Health, National Institute of Health.
- Gutierrez J (2011) Correlation of cough frequency with treatment efficacy in pulmonary tuberculosis patients in Lima, Peru. [Master's Thesis] Connecticut: University of Connecticut Graduate School.
- World Bank Group (2015) PERU building on success, boosting productivity for faster growth. Washington, D.C. GMFDR, International Bank for Reconstruction and Development, International Development Association or the World Bank.
- Alfaro FM (1996) National Institute of Statistics and Informatics (INEI). Metropolitan Lima: Socio-Demographic Profile. Lima: INEI.
- Alarcón V, Alarcón E, Figueroa C, Mendoza-Ticona A (2017) Tuberculosis in Peru: Epidemiological situation, advances and challenges for its control. Rev Peru Med Exp Salud Publica 34: 299-310.
- Loayza ALG (2016) Perception of quality of life in patients with pulmonary tuberculosis in the second phase of antituberculous treatment at the El Agustino health center.
- Canelo-Aybar C, Balbin G, Perez-Gomez A, Florez ID (2016) Clinical practice guidelines in Peru: Evaluation of their quality using the AGREE II instrument. Rev Peru Med Exp Public Health. 33: 732-738.
- Zagaria AEM (2008) Tuberculosis: A preventable cause of death in the elderly. US Pharm 33: 23-25.
- Perez-Guzman C, Vargas MH, Torres Cruz A, Villareal -Velarde H (1999). Does aging modify pulmonary tuberculosis? A meta-analytical review. Chest 116: 961-967.
- Gruver AL, Hudson LL, Sempowski GD (2007) Immunosenescence of ageing. J Pathol 211: 144-156.
- Silva FSB, Castilho AL, Maltempe FG, Pina RZ, Takao EKH, et al. (2013) Use of the Ogawa-Kudoh method to isolate mycobacteria in a tuberculosis reference laboratory in northwestern Paraná, Brazil. Braz J Pharm Sci 49: 567-570.
- Hipólito Unanue National Hospital (2015) Nosocomial tuberculosis report in health personnel in years 2000-2015. HNHU/MINSA: Office of Epidemiology and Environmental Health, Occupational Health Unit, Report of Occupational Diseases.
- Menzies D, Fanning A, Yuan L, Fitzgerald M (1995) Tuberculosis among health care workers. N Engl J Med 332: 92-98.
- Tacuri TME (2009) Relationship between adherence and level of knowledge about the treatment of patients with tuberculosis at the Primavera El Agustino Health Center, 2009. [Thesis] Lima: National University of San Marcos.
- Del Pilar Quevedo CLN, Sanchez RRL, Villalba PFK, Velásquez CD (2015) Relationship of family and social support in compliance with the treatment of patients with pulmonary tuberculosis in health centers. Rev Enferm Herediana 8: 11-16.
- Urday FD, Chimaja PA (2014) Mobilization of Social Capital for the Control of Tuberculosis in the Jurisdiction of Cerro San Cosme: The Case of the TBcero Plan. [Master Thesis] Lima: Pontificia Universidad Católica Del Perú, Graduate School.
- Soto A, Solari L, Agapito J, Acuna-Villaorduna C, Lambert ML, et al. (2008) Development of a clinical scoring system for the diagnosis of smear-negative pulmonary tuberculosis. Braz J Infect Dis 12: 128-132.
Open Access Journals
- Aquaculture & Veterinary Science
- Chemistry & Chemical Sciences
- Clinical Sciences
- Engineering
- General Science
- Genetics & Molecular Biology
- Health Care & Nursing
- Immunology & Microbiology
- Materials Science
- Mathematics & Physics
- Medical Sciences
- Neurology & Psychiatry
- Oncology & Cancer Science
- Pharmaceutical Sciences